Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Acceledent.co.uk

4 CE credits
written for orthodontists,
dentists, dental hygienists,
and assistants.
Advances in Orthodontic
A Peer-Reviewed Publication
Written by Jeremy J. Mao, DDS, PhD and Chung H. Kau, DDS, MScD, MBA,
PhD, M Orth, FDS, FFD(Ortho), FAMS(Ortho)
This course has been made possible through an unrestricted educational grant. The cost of this CE course is $59.00 for 4 CE credits.
Cancellation/Refund Policy: Any participant who is not 100% satisfied with this course can request a full refund by contacting PennWell in writing.
Patients may elect to forego orthodontic treatment due
The overall goal of this article is to provide dental profession-
to the cost of treatment, the duration of treatment – most
als with information on orthodontic treatment options.
cases traditionally take 1.5–2.5 years to complete – or due to
Upon completion of this course, the participant will be
the appearance of orthodontic appliances (depending on the
able to do the following:
type used). In addition, some patients have difficulty wearing
1. Know the reasons patients request orthodontic treatment,
orthodontic appliances, which can result in patients starting
as well as the reasons they may reject orthodontic treatment
but not completing orthodontic treatment. Dental profes-
2. Know the biomechanics involved in orthodontic tooth
sionals may reject patients for orthodontic treatment due
to an assessment that the patient will be noncompliant with
3. Know the factors that can increase the duration of
treatment or noncompliant with oral hygiene requirements
orthodontic treatment
during orthodontic treatment. The patient's treatment may
4. Understand the role static and cyclic forces play in
also be discontinued due to noncompliance. The duration of
biomechanics and the potential duration of orthodontic
treatment, oral hygiene requirements and appearance during
treatment vary depending on the type of orthodontic treat-ment and appliances used.
Abstract
Functionality and aesthetics are key considerations in patients
Table 2. Rejection of treatment
requesting, and orthodontists recommending, orthodontic
treatment. However, patients may elect to forego orthodontic
Duration of treatment
treatment due to the cost and the duration of treatment. Orth-
Poor aesthetics during treatment
odontic treatment can be provided using removable or fixed
Difficulty wearing an appliance
orthodontic appliances (FOAs), and current options offer
improved aesthetics compared to earlier generation appliances.
Many methods have been explored and developed to reduce
Poor compliance with use (removable)
the duration of treatment. Most recently, a device has been
Poor compliance with adjustment appointments
developed that utilizes the concept of cyclic force application
Poor oral hygiene
to reduce the duration of orthodontic treatment.
Unrealistic patient expectations
Introduction
Orthodontic treatment is requested and recommended for
functionality and aesthetics. Patients seek orthodontic treat-
Orthodontic treatment can be provided using removable or
ment primarily for aesthetic reasons. Orthodontists typically
fixed orthodontic appliances (FOAs). Removable appliances
recommend orthodontic treatment to patients for function.
include acrylic plates with clasps and springs variously posi-
The number of orthodontic cases has continued to grow over
tioned depending on the treatment needs. Simple orthodontic
time. Between 1990 and 1999, the number of orthodontic
cases can be successfully treated using this type of appliance,
cases annually more than doubled, from approximately 25.8
which also relies on the patient wearing the appliance as in-
million cases to more than 61 million cases. The majority of
structed. Since the appliance is removable, patients may be
cases in 1999 were for comprehensive therapy – around 48
noncompliant and leave the appliance out for extended periods
million, with 81.5% of these in the 10–19 age group and just
of time, which can result in slower treatment or "reversal" of
over 14% in adults age 20 and over.1 The number of adult cases
tooth movements. Other removable appliances include those
has increased in the last decade as the importance of aesthetics
designed for specific tooth movements, such as the Schwartz
has increased and affluence has led to an increased demand.
appliance. Removable appliances offer the advantage of being
Treated cases by age and type can be found in Table 1.
able to be removed for oral hygiene procedures, simplifying oral home care, but are subject to noncompliance and lack of
Table 1. Orthodontic cases
use by patients.
A more recent removable option is the use of clear resin
age 10 10 - 19 and above
full coverage "invisible" orthodontic appliances (Invisalign,
Align Technology). These have increased adult orthodontic
case acceptance and adult requests for orthodontia due to
their acceptable aesthetics. Clear, full-coverage, removable
resin appliances are not indicated for all types of cases, and
7,118,200 19.40% 56.90%
three-axis tooth movement is better controlled using standard
Adapted from: American Dental Association. 1999 Survey of dental services rendered
fixed appliances; they can be used stand-alone or after use of a fixed orthodontic appliance. Clear aligners have been found

to be more comfortable for the patient and to result in less
steel bands and archwires. The latest-generation fixed orth-
periodontal inflammation than fixed appliances (noting that
odontic appliances utilize either clear or metal brackets that
such periodontal inflammation has been found to resolve fol-
are bonded onto the buccal/facial surfaces of the teeth with
lowing removal of fixed appliances).2,3 However, Invisalign
the archwire threaded through attachments on the brackets.
and similar products only address crowding up to a few mil-
The ability to successfully bond orthodontic brackets to teeth
limeters and cannot address most cases with bicuspid extrac-
has removed the need to utilize banding encircling the teeth,
tions. Accordingly, Invisalign and similar products only serve
thereby improving aesthetics and reducing discomfort, as
a fraction of the orthodontic patient population.
well as reducing the impact of orthodontic treatment on oral
hygiene requirements and difficulties. In addition, the use of
Figure 1. Clear, full-coverage aligner
clear resin bonded brackets has substantially improved the aesthetics during treatment with FOAs. Currently available appliances frequently incorporate the use of elastics into forces applied during therapy, and nickel-titanium is utilized for the archwires and other wire/spring components. Varia-tions include lingual/palatal appliances designed to achieve tooth movement with improved aesthetics during treatment, and the use of self-ligating brackets, which have simplified the process of attaching archwires to brackets.
Regardless of the design, each generation of orthodontic
appliance to date has utilized static force to move the teeth, i.e., force that is applied continually between visits and is only altered as a result of adjustments during orthodontic
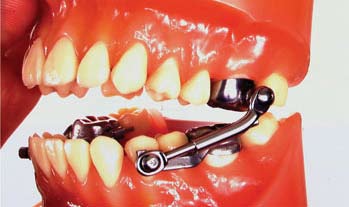
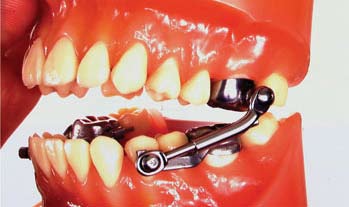
Functional appliances are used to influence and alter the po-
sitioning of the patient's hard tissues (teeth, alveolar bone and jaw positions) by altering the patient's function. These may
Mechanism of Action of Orthodontic Appli-
be fixed or removable. Examples of functional appliances
include the Herbst, which is fixed and therefore does not
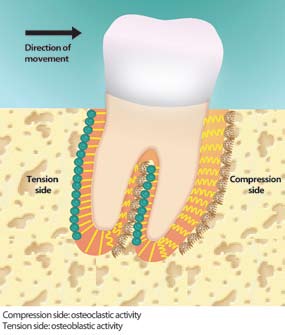
Bone is known to adapt to mechanical forces, including weight-
require patient compliance for wear; the bionator and Frankel
bearing loads and orthodontic (therapeutic) forces, thereby
appliances, which are removable.
biologically balancing the load-bearing capacity of bone with the mechanical stress to which it is subjected.5,6,7 The opposite
Figure 2. Functional appliance (Herbst)
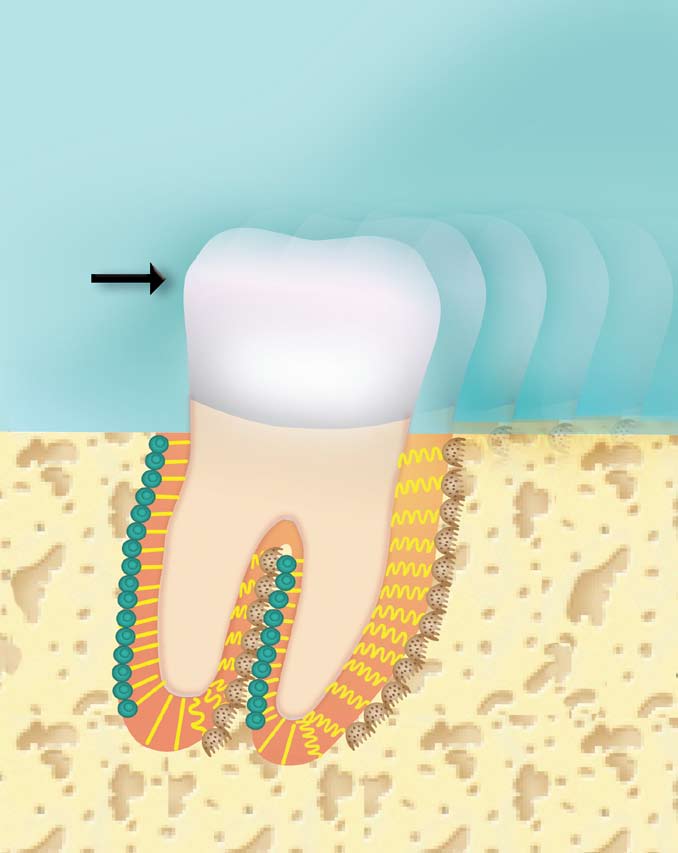
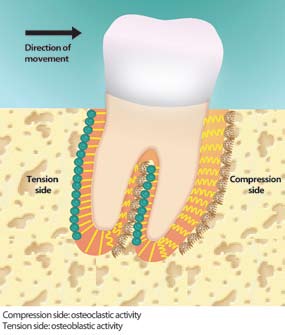
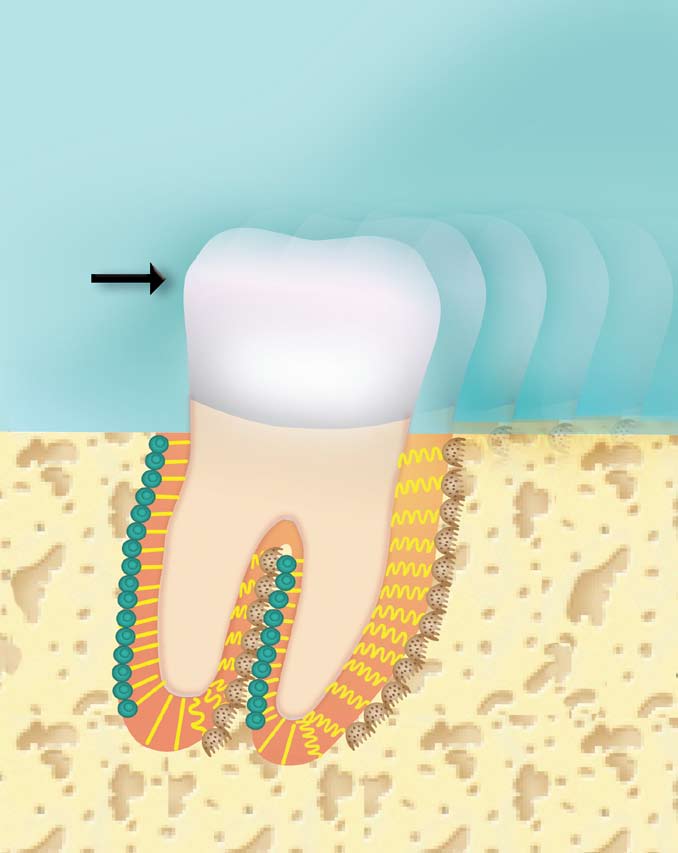
is also seen with disuse atrophy, when loss of bone or muscle mass occurs with disuse, such as during immobilization.8 The application of mechanical force is the premise for orthodontic tooth movement. When a mesial force is placed on a tooth, bone is resorbed on the mesial surface (compression side) and laid down on its distal (tension side) surface.
Orthodontic appliances have relied on static force to induce
bone remodeling and tooth movement, with the duration of treatment depending on the rate of bone remodeling. As force is applied to the tooth, micromovement results in it flexing, and the periodontal ligament and bone on that aspect of the root undergo remodeling, with resorption of the bone. The alveolar bone on the opposite side undergoes bone formation.
Fixed orthodontic appliances are used for the majority of
This combination represents the bone remodeling process
orthodontic cases. Modern fixed orthodontic appliances
during orthodontic treatment. The osteoclasts are respon-
have their genesis in Angle's ribbon arch technique, which
sible for bone resorption, which begins with the attachment
was introduced in the early 20th century. The ribbon arch
of these cells to the bone surface, after which acid dissolution
technique utilized a curved archwire with friction sleeve
of the hydroxyapatite occurs and is followed by destruction
nuts and threaded ends, and bands with lockpins cemented
of the bone's organic matrix. The osteoblasts are the cells
on the teeth. This appliance was the first that could achieve
that develop bone matrix and maintain the bone's structure.9
controlled three-axis tooth movement.4 The ribbon arch tech-
The mechanical forces during orthodontic treatment result
nique was subsequently replaced by the Edgewise technique
in tissue-borne and cell-borne mechanical stresses, which in
in the 1920s. Over time, nickel-silver bands and archwires su-
turn induce interstitial fluid flow. The anabolic or catabolic ef-
perseded gold-platinum, and were later replaced by stainless
fects of this fluid flow rely upon deformation of extracellular
matrix molecules, transmembrane channels, the cytoskeleton
over time, hypothesized to be a result of the bone becoming
and intranuclear structures.10
desensitized to it.19,20 It is known that bone responds to a few
Chemical mediators are involved in the bone remodeling
cycles of large strain, however, it also responds to low mag-
process associated with orthodontic movement, which is an
nitude strain with many cycles or high-frequency vibrations,
inflammatory process. This involves interaction between the
resulting in an increase in bone density.21,22 With static force,
osteoclasts and osteoblasts. The osteoblasts produce Recep-
a balance has been required between the amount of force ap-
tor activator of nuclear factor kappa B ligand (RANKL) in re-
plied and the speed of tooth movement. Too little force can
sponse to the release of prostaglandin (PGE )from osteoclasts.
substantially increase the duration of treatment. Applying
In turn, this ligand expresses osteoprotegerin (OPG), which
too much force may result in more rapid tooth movement,
suppresses osteoclast formation.11,12 Compressive forces on
but with deleterious effects that include root resorption and
periodontal ligament (PDL) cells induce RANKL expres-
the potential for increased discomfort during treatment.
sion with few changes in OPG expression. In contrast, tensile
Root resorption is a natural process that occurs during the
forces on PDL cells cause the up-regulation of both OPG and
exfoliation of the primary dentition. In the permanent
RANKL expression. These differences may explain why the
dentition, root resorption can be associated with previous
compression side of orthodontic tooth movement is associ-
endodontic therapy, trauma, inappropriate use of internal
ated with an increase in bone resorption.13,14,15,16
bleaching agents (i.e., inappropriate use of a chemical agent and/or lack of a coronal seal for the root canal), or inap-
Figure 3. Orthodontic tooth movement
propriate orthodontic forces. The act of intruding teeth has been shown to increase the risk of root resorption compared to extruding teeth. It has also been suggested that the use of anti-inflammatories may inhibit orthodontic root resorption; their use also reduces orthodontic tooth movement by reduc-ing inflammation.23,24,25
The size, amount, and type of orthodontic force applied,
as well as the type of tooth movement being effected all influ-ence external root resorption, as do individual risk factors that probably include genetic predisposition.26,27
Table 3. Factors in treatment duration
Complexity of the caseAmount of tooth movement requiredType of appliance usedComplianceOral hygieneAmount of forceType of force
Considerations in the Duration of Orthodon-
Medication use – anti-inflammatories
tic Treatment
The duration of treatment is influenced by the complex-
ity of the case, the amount of tooth movement required, and
Reducing the Duration of Treatment
the type of appliance used. For similar malocclusion cases,
The lengthy duration of orthodontic treatment can deter
noncompliant patients are likely to have a longer duration of
patients from receiving treatment and can result in increased
treatment than compliant patients; it is also known that pa-
noncompliance or in patients aborting treatment.28 Lengthy
tients who are noncompliant with oral hygiene are more likely
orthodontic treatment is more likely to elicit aberrant root
to be the patients who attend recall adjustment appointments
resorption. Many methods have been explored to reduce the
with irregularity.
duration of treatment. Treatment planning has improved and
Treatment duration is also influenced by the amount and
become more sophisticated, with staging of tooth movements
type of force applied to the teeth as a function of bone re-
based on linear and rotational velocities, which has enabled
modeling dynamics. It has been shown that dynamic forces,
simultaneous movement of all teeth, rather than a few at a
rather than static forces, result in increased bone formation
time. This also results in more space between the teeth during
and the anabolic effects of mechanical loading.17,18 Further-
movement, rather than relying on interproximal reduction.29
more, the response to a long-duration static load decreases
In vivo experiments utilizing chemical mediators associated

with orthodontic tooth movement have also shown that the in-
ened cortical plate, with the alveolar crest height maintained
troduction of exogenous OPG reduces the rate of orthodontic
during treatment. In addition, no significant root resorption
movement, while RANKL increases its rate. This approach
was found, hypothesized to be due to demineralization/
may hold promise for the future in the regulation of the rate
remineralization of the bone rather than resorption and ac-
of tooth movement.30,31,32 However, application of chemical
cretion of bone found with typical orthodontic tooth move-
or biological mediators may have untoward side effects locally
ment.37,38 Partial decortication has been found to increase
in the oral cavity and/or systemically, affecting other organs.
both anabolic and catabolic effects in laboratory studies. The
The development of novel chemical or biological mediators
catabolic effects were found to increase osteoclast activity and
typically takes years if not decades, and requires excessively
reduce bone surface, while the anabolic effects increased bone
large resources. Surgical orthodontics and temporary anchor-
formation. Increased bone turnover was found, localized to
age devices have all been introduced that can also increase the
the area adjacent to the decortication.39
speed of treatment and reduce its duration.
Table 4. Methods of reducing treatment duration
Temporary anchorage devices
Staging of tooth movements (linear and rotational velocities)
The use of temporary anchorage devices (TADs), also known as mini-implants or mini orthodontic screws, can speed up
Temporary anchorage devices
orthodontic treatment in some cases.33,34 TADs produce ab-
solute skeletal anchorage and have been used successfully to
Cyclic force application
treat cases of varying degrees of complexity. Care is required
Use of chemical mediators (experimental)
during their placement to ensure they are correctly positioned and to avoid iatrogenic damage associated with impingement of a TAD on a nerve, root surface or the periodontal liga-
The Application of Cyclic Force
ment. Extra care is also required by the patient to maintain
Research has demonstrated that the use of cyclic forces
oral hygiene around the TAD to avoid infection at the site of
increases the rate of bone remodeling compared to static
forces.40,41,42 In a pilot study in one human subject, a pulsat-ing force device was investigated and was found to enhance
Figure 4. Temporary anchorage device and FOA
and speed tooth movement, although it was never introduced
commercially; both the rate of movement and the total amount of movement were enhanced.43
Cyclic forces have been found to accelerate the rate of
bone remodeling to levels far greater than static forces or intermittent forces.41,42,44,45,46,47 While similar in their noncon-stant nature, cyclic forces – sometimes referred to as pulsatile forces – are different than intermittent forces that are applied for some duration of time, removed, and then reapplied.48 A static force occurs once and affects cells once; an intermittent force is still a static force, the only difference is that it is intro-
duced episodically. In contrast, cyclic forces are oscillatory in nature and change magnitude rapidly and repeatedly, affect-
ing the cells with each oscillation of force magnitude.48,49 The
Surgical orthodontics has been introduced to increase both the
frequency of cyclic forces is never zero. Force frequency is a
amount and speed of tooth movement. One technique, Wil-
concept of critical importance, but has rarely been considered
ckodontics, utilizes a combination of orthodontic treatment
in the field of orthodontics and dentofacial orthopedics until
and alveolar ridge augmentation. Selective partial decortica-
tion of the cortical plates has been found to increase the speed
Cyclic forces cause deformation by changing a structure's
of tooth movement during orthodontic therapy compared to
length multiple times, whereas intermittent and static forces
traditional FOAs. After placement of the FOA, decortication
can only do so once per application. At force frequencies
can be performed several days later, with full-thickness flaps
that are greater than zero, cells are impacted multiple times.
used at the surgical site. This can be accompanied by alveolar
Frequencies of interest for orthodontic application range
bone grafting/augmentation to increase the thickness of the
from several hertz (Hz.) up to 100 Hz. or more. Cyclic forces
bone plate at sites where thicker bone will be desirable. Cases
impact tissue structures and cells multiple times, and this
performed where adjustments were made every two weeks for
seemingly subtle difference has been shown to lead to dra-
the application of static forces have shown that this method
matic differences in biological response in both orofacial and
increases the rate of tooth movement and results in a thick-
long bones.41,42,47,49,50 Multiple cycles of change in force mag-

nitude, or cyclic forces, are significant because cells respond
One portion of the device is a mouthpiece similar to a sports
more readily to rapid oscillation in force magnitude than to
mouthpiece, which the patient bites onto during use. The
constant force.50 A force propagating through a biological
mouthpiece portion is connected to another piece that stays
tissue, such as alveolar bone and the periodontal ligament,
outside the mouth; this portion (activator) houses the com-
is transduced as a tissue-borne and cell-borne mechanical
ponents that provide the cyclic forces (vibration). The acti-
stress that in turn induces interstitial flow.51 Although fluid
vator includes a battery, motor, rotating weights and micro-
flow is a current focus of the mechanotransduction pathways,
processor for storing usage data. The patient connects the
its anabolic and catabolic effects rely upon deformation of
mouthpiece to the activator and uses the device once daily
extracellular matrix molecules, transmembrane channels,
for 20 minutes. The applied force from the device is at 0.2 N
the cytoskeleton and intranuclear structures. 10,50,51 Cells are
(20 grams). This low force is intended to be barely notice-
known to respond more readily to rapid oscillation in force
able and not uncomfortable. The device can be used with
magnitude (i.e., to cyclic forces) than to constant forces.51
all FOAs as well as clear resin aligners (Invisalign). The ac-
Animal studies using cyclic forces of 0.3–5 newtons
tivator is placed in a docking station between uses to both
(N) have demonstrated increased bone remodeling, and the
recharge the activator and show compliance data.
delivery of cyclic forces by a vibrational device applied to molar teeth in the presence of standard static forces from an
orthodontic spring resulted in a significant increase in tooth
A pilot clinical study was conducted with 17 subjects, 14 of
movement compared to no adjunctive device use. There was
whom completed the study. Subjects with a Class I maloc-
also a trend towards less root resorption when cyclic forces
clusion and at least 6 mm of lower anterior crowding were
were applied.46,52,53,54
provided with the device and instructed to use it for 20
Cyclic forces have been used for other parts of the body,
minutes daily for six months during orthodontic treatment.
such as the Juvent system that is used to counteract lost bone
Other selection criteria for the study included estimated level
and muscle.55 A second device using cyclic forces was intro-
of compliance with use of the device in accordance with the
duced to relieve the discomfort associated with orthodontic
instructions and good oral hygiene. Several subjects also re-
adjustments and was found to be safe and effective.56 Recently,
quired extractions and space closure.
a new device has been introduced (AcceleDent, OrthoAccel
Although compliance varied from patient to patient, pa-
Technologies) that utilizes cyclic forces to reduce the duration
tients reported using the device about 80% of the time, while
of orthodontic treatment. The cyclic forces utilized are lower
the device microcomputer documented a 67% usage rate.
than for the pre-existing device used to relieve discomfort.
Patients reported no adverse events during the study. Most patients reported watching television, listening to music, or
playing video games while using the device. The most com-
The AcceleDent device uses the application of cyclic forces
mon word patients used to describe their device use was easy.
to move teeth in bone faster through accelerated bone re-
A cone beam device (Galileos, Sirona) was utilized to ac-
curately measure tooth roots and to estimate any resulting root resorption, with imaging in all three planes (sagittal, axial and
Figure 5. AcceleDent device
coronal views). The study was designed to determine if any root resorption greater than 0.5 mm occurred, or if there were alterations in root lengths. At the conclusion of the study, it was found that the differences in mean root lengths, with mea-surements made to the mesial buccal roots of all teeth except second and third molars, ranged from -0.127 mm to -0.416 mm in both arches. These differences were not statistically significant, and no significant differences were noted between anterior and posterior teeth. It should be noted that 0.5 mm is well below the levels of 2 mm, or one-third of the root length, considered to be clinically significant by researchers.57,58
The study measured distances between teeth using a digi-
tal caliper. The overall distance in millimeters between the front five teeth, both upper and lower, was calculated during the alignment phase. The gap between teeth due to extrac-tions was measured directly. The overall movement rate dur-ing the study was 0.526 mm per week. It was found that this device speeds up orthodontic movement without resulting in
root resorption.
This device increases the rate of orthodontic tooth move-
Static forces that are applied for a time, removed, and then
ment and can be used with either FOAs or clear aligners,
offering flexibility. This is useful given the mix of orthodontic
therapies available and particularly since some patients have
Microscopic movements such as occur in teeth during
combination therapy utilizing both FOAs and clear aligner
orthodontic treatment
therapy. Short-term daily use for 20 minutes is an advantage
Static forces: Forces that are applied once at a constant
Orthodontic treatment is designed to result in improved
1 American Dental Association. The 1999 survey of
aesthetics and/or function of the dentition and the face. Pa-
dental services rendered. 2002.
tients desire orthodontic treatment that is of short duration,
2 Boyd RL. Periodontal and restorative considerations
effective and that does not negatively impact their appearance
with clear aligner treatment to establish a more
during treatment. The introduction first of clear brackets for
favorable restorative environment. Compend Contin
fixed orthodontic appliances has improved aesthetics during
Educ Dent. 2009; 30(5):280-2, 284, 286-8 passim.
3 Kravitz ND, Kusnoto B, BeGole E, et al. How well
A number of methods have been introduced to help
does Invisalign work? A prospective clinical study
evaluating the efficacy of tooth movement with
reduce the duration of treatment. Surgical corticotomies
Invisalign. Am J Orthod Dentofacial Orthop. 2009;
and temporary anchorage devices have been advocated
for shorter-duration treatment. Most recently, a device
4 Dewel BF. The Ribbon arch: its influence in the
has been developed that utilizes the concept of cyclic force
development of orthodontic appliances. Angle
application to reduce treatment time by accelerating bone
Orthod. 1981; 51(4):263-8.
5 Turner CH, Woltman TA, Belongia DA. Structural
Reducing the duration of treatment with effective and
changes in rat bone subjected to long-term, in vivo
safe techniques, and improving aesthetics during treatment,
mechanical loading. Bone. 1992; 13(6):417-22.
increases the acceptability of orthodontic treatment for pa-
6 Rubin CT, Gross TS, McLeod KJ, Bain SD.
tients. The concept of the use of static forces in orthodontics
Morphologic stages in lamellar bone formation
has not been challenged in more than a century of clinical
stimulated by a potent mechanical stimulus. J Bone
practice. New technologies related to the biological impact
Miner Res. 1995; 10(3):488-95.
of force frequencies could represent a paradigm shift in
7 Wolf J. The law of bone remodeling. 1986, New York:
8 Leblanc AD, Schneider VS, Evans HJ, Engelbretson
Glossary of Terms
DA, Krebs JM. Bone mineral loss and recovery after
17 weeks of bed rest. J Bone Miner Res. 1990; 5(8):843-
The effect of promoting metabolism for the buildup of a
9 De Baat P, Heijboer MP, de Baat C. Development,
tissue such as bone or muscle
physiology, and cell activity of bone. Ned Tijdschr
Tandheelkd. 2005 Jul; 112(7):258-63.
The metabolic breakdown of tissues, such as bone or muscle,
10 McLeod KJ, Rubin CT, Otter MW, et al. Skeletal cell
or complex molecules
stresses and bone adaptation. Am J Med Sci. 1998;
Forces with rapidly varying magnitudes during the period of
11 Yasuda H, Shima N, Nakagawa N, Yamaguchi K,
Kinosaki M, et al. Osteoclast differentiation factor
is a ligand for osteoprotegerin/osteoclastogenesis-
The removal of the outer layer of a structure (e.g., bone)
inhibitory factor and is identical to TRANCE/
RANKL. Proc Natl Acad Sci. 1998; 95(7):3597-602.
The wasting of tissues (typically bone and muscle) due to
12 Tsukii K, et al. Osteoclast differentiation factor
mediates an essential signal for bone resorption
induced by 1 alpha,25-dihydroxyvitamin D3,
prostaglandin E2, or parathyroid hormone in the
A unit of frequency defined as the number of complete cycles
microenvironment of bone. Biochem Biophys Res
per second. It is the basic unit of frequency in the Intern
Commun. 1998; 246(2):337-41.
tional System of Units (SI), and is used worldwide in both
13 Nakao K, et al. Intermittent force induces high
general-purpose and scientific contexts. Hertz can be used to
RANKL expression in human periodontal ligament
measure any periodic event.
cells. J Dent Res. 2007; 86(7):623-8.
Intermittent forces:
14 Kanzaki H, et al. Periodontal ligament cells under
mechanical stress induce osteoclastogenesis by
malocclusions. J Dent Educ. 2008 Aug; 72(8):948-67.
receptor activator of nuclear factor kappaB ligand
30 Dunn MD, Park CH, Kostenuik PJ, Kapila S,
up-regulation via prostaglandin E2 synthesis. J Bone
Giannobile WV. Local delivery of osteoprotegerin
Miner Res. 2002; 17(2):210-20.
inhibits mechanically mediated bone modeling in
15 Tsuji K, et al. Periodontal ligament cells under
orthodontic tooth movement. Bone. 2007;41(3):446-
intermittent tensile stress regulate mRNA expression
of osteoprotegerin and tissue inhibitor of matrix
31 Kanzaki H, et al. Local RANKL gene transfer to
metalloprotease-1 and -2. J Bone Miner Metab. 2004;
the periodontal tissue accelerates orthodontic tooth
movement. Gene Ther. 2006; 13(8):678-85.
16 Grieve WG III, et al., Prostaglandin E (PGE) and
32 Kanzaki H, et al. Local OPG gene transfer to
interleukin-1 beta (IL-1 beta) levels in gingival
periodontal tissue inhibits orthodontic tooth
crevicular fluid during human orthodontic tooth
movement. J Dent Res. 2004; 83(12):920-5.
movement. Am J Orthod Dentofacial Orthop. 1994;
33 Luzi C, Verna C, Melsen B. Immediate loading of
orthodontic mini-implants: a histomorphometric
17 Liskova M, Hert J. Reaction of bone to mechanical
evaluation of tissue reaction. Eur J Orthod. 2009;
stimuli. 2. Periosteal and endosteal reaction of tibial
diaphysis in rabbit to intermittent loading. Folia
34 Melsen B. Mini-implants: Where are we? J Clin
Morphol (Praha). 1971; 19(3):301-17.
Orthod. 2005; 39:539-547.
18 Rubin CT, Lanyon LE. Regulation of bone formation
35 Rossouw PE, Buschang PH. Temporary orthodontic
by applied dynamic loads. J Bone Joint Surg [Am].
anchorage devices for improving occlusion. Orthod
Craniofac Res. 2009 Aug; 12(3):195-205.
19 Lanyon LE. Functional strain as a determinant for
36 Cho HJ. Clinical applications of mini-implants as
bone remodeling. Calcif Tissue Int. 1984; 36 Suppl
orthodontic anchorage and the peri-implant tissue
reaction upon loading. J Calif Dent Assoc. 2006;
20 Umemura Y, et al. Five jumps per day increase bone
mass and breaking force in rats. J Bone Miner Res.
37 Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ.
1997; 12(9):1480-5.
Rapid orthodontics with alveolar reshaping: two case
21 Lanyon, LE. The success and failure of the adaptive
reports of decrowding. Int J Periodontics Restorative
response to functional load-bearing in averting bone
Dent. 2001 Feb; 21(1):9-19.
fracture. Bone. 1992; 13 Suppl 2:S17-21.
38 Ferguson DJ, Wilcko WM, Wilcko MT. Accelerating
22 Rubin C, et al. Mechanical strain, induced
orthodontics by altering alveolar bone density. Good
noninvasively in the high-frequency domain, is
Practice. 2001; 2:2-4.
anabolic to cancellous bone, but not cortical bone.
39 Sebaoun JD, Ferguson DJ, Kantarci A, Carvalho RS,
Bone. 2002; 30(3):445-52.
van Dyke TE. Trabecular Bone Modeling and RAP
23 Abuabara A. Biomechanical aspects of external root
Following Selective Alveolar Decortication. Available at
resorption in orthodontic therapy. Med Oral Patol
Oral Cir Bucal. 2007 Dec 1; 12(8):E610-3.
24 Kehoe MJ, et al. The effect of acetaminophen,
ibuprofen, and misoprostol on prostaglandin E2
40 Mao JJ, Wang X, Kopher RA. Biomechanics of
synthesis and the degree and rate of orthodontic tooth
movement. Angle Orthod. 1996; 66(5):339-49.
craniofacial sutures: orthopedic implications. Angle
25 Chumbley AB, Tuncay OC. The effect of indomethacin
Orthod. 2003; 73:128-135.
(an aspirin-like drug) on the rate of orthodontic tooth
41 Mao JJ, Wang X, Mooney MP, et al. Strain induced
movement. Am J Orthod. 1986; 89(4):312-4.
osteogenesis in the craniofacial suture upon controlled
26 Brezniak N, Wasserstein A. Root resorption after
delivery of low-frequency cyclic forces. Front Biosc.
orthodontic treatment. Part 2: Literature review. Am
J Orthod Dentofacial Orthop. 1993 Feb; 103(2):138-
42 Mao JJ. Calvarial development: cells and mechanics.
Curr Opin Orthopaed. 2005; 16:331-337.
27 Ngan DC, Kharbanda OP, Byloff FK, Darendeliler
43 Shapiro E, Roeber FW, Klepmner LS. Orthodontic
MA. The genetic contribution to orthodontic root
resorption: a retrospective twin study. Aust Orthod J.
piezoelectricity. Am J Orthod. 1979; 76(1):59-66.
2004 May; 20(1):1-9.
44 Mao JJ. Mechanobiology of craniofacial sutures. J
28 Roykó A, Dénes Z, Razouk G. The relationship
Dent Res. 2002; 81:810-816.
between the length of orthodontic treatment and
45 Wang X, Mao JJ. Accelerated chondrogenesis of
patient compliance. Fogorv Sz. 1999 Mar; 92(3):79-
the rabbit cranial base growth plate upon oscillatory
mechanical stimuli. J Bone Min Res. 2002; 17:1843-
29 Boyd RL. Esthetic orthodontic treatment using
the Invisalign appliance for moderate to complex
46 Peptan AI, Lopez A, Kopher RA, et al. Responses
of intramembranous bone and sutures upon in vivo
editorial board of Medical Engineering and Physics and
cyclic tensile and compressive loading. Bone. 2008;
Frontiers of Bioscience. Dr. Mao is the editor of a new book
42: 432-438.
entitled "Translational Approaches in Tissue Engineering
47 Mao JJ, Nah HD. Growth and development:
and Regenerative Medicine." Dr. Mao is also the editor of
Hereditary and mechanical modulations. Am J
an upcoming textbook entitled "Principles of Craniofacial
Orthod Dentofac Orthoped. 2003; 125:676-689.
Growth and Development." Dr. Mao is currently a standing
48 Wise GE, King GJ. Mechanisms of tooth eruption
member of the Musculoskeletal Tissue Engineering Study
and orthodontic tooth movement. J Dent Res. 2008;
Section of the NIH and serves on a number of review panels
49 Konoo T, Kim YJ, Gu GM, et al. Intermittent force
for NIH, NSF, US Army as well as many other grant review
in orthodontic tooth movement. J Dent Res. 2001;
panels in over 18 different countries. Dr. Mao has been in-
vited to give lectures at over 130 national and international
50 Gross TS, Edwwards JUL, McLeod KJ, et al. Strain
conferences. He has also organized and chaired a number of
gradients correlate with sites of periosteal bone
scientific conferences including NIH-sponsored Stem Cells
formation. J Bone Miner Res. 1997; 12:982-988.
and Tissue Engineering Conference. Dr. Mao's laboratory is
51 Duncan RL, Turner CH. Mechanotransduction and
currently funded by several research grants from the National
the functional response of bone to mechanical strain.
Institutes of Health and also from industry. Dr. Mao is a
Calcif Tissue Int. 2005; 57:344-358.
consultant to Tissue Engineering and Regenerative Medicine
52 Kopher RA, Mao JJ. Suture growth modulated by the
Centers in the United States and overseas.
oscillatory component of micromechanical strain. J.
Bone and Min Res. 2003; 18(3):521-528.
Chung H. Kau, DDS, MScD, MBA, PhD, M Orth,
53 Vij K and Mao JJ. Geometry and cell density of
FDS, FFD(Ortho), FAMS(Ortho)
rat craniofacial sutures during early postnatal
Dr. Kau completed his dental training at the Faculty of
development and upon in-vivo cyclic loading. Bone.
Dentistry at the National University of Singapore and his
orthodontic specialty and academic training at the Cardiff
54 Nishimura, et al. Periodontal tissue activation by
vibration: intermittent stimulation by resonance
University in Wales, UK. Dr. Kau is an active researcher
vibration accelerates experimental tooth movement
with a keen interest in three-dimensional research. He is an
in rats. Am J Orthod Dentofacial Orthop 2008;
invited speaker on this topic and has shared his work on the
international stage that includes North America, Western
55 www.juvent.com.
and Central Europe, the Baltic States, Hungary and the Far
56 Marie SS, Powers M, Sheridan JJ. Vibratory stimulation
East. He actively contributes and publishes in the orthodontic
as a method of reducing pain after orthodontic
literature and currently has over 150 publications and confer-
appliance adjustment. J Clin Orthod. 2003;37(4):205-
ence papers. His other research interests include multi-centre
randomized control trials in orthodontics and the clinical
57 Lupi JE, Handelman CS, Sadowsky C. Prevalence and
management of hypodontia. Dr. Kau also serves on the in-
severity of apical root resorption and alveolar bone
ternational educational level and is on the Panel of Examin-
loss in orthodontically treated adults. Am J Orthod
ers for the Royal College of Surgeons in Edinburgh and an
Dentofacial Orthop. 1996 Jan; 109(1):28-37.
international examiner for the College in Cairo, Egypt. Ad-
58 Sameshima GT, Sinclair PM. Predicting and
ditionally, he is on the editorial review board for the American
preventing root resorption. Part 2: Treatment factors.
Journal of Orthodontics and Dento-facial Orthopaedics and
Am J Orthod Dentofacial Orthop. 2001 May;
ad hoc reviewer for a number of other journals which include the Journal of Orthodontics, Angle Orthodontist, Cleft Lip and Palate Journal, International Journal of Computer As-
sisted Radiology and Surgery and Evidence Based Dentistry
Jeremy J. Mao, DDS, PhD
Dr. Mao is currently Professor and Director of the TissueEngineering and Regenerative Medicine Laboratory at Co-lumbia University. Dr. Mao has published over 100 scientific papers and book chapters in the area of tissue engineering,
stem cells and regenerative medicine. He currently serves on
Dr. Jeremy Mao has an interest in OrthoAccel.
the editorial board of several scientific journals including Tis-sue Engineering, Journal of Biomedical Material Research,
International Journal of Oral and Maxillofacial Surgery, and
We encourage your comments on this or any PennWell course.
Journal of Dental Research, and has served as an Associate
For your convenience, an online feedback form is available at
Editor of Stem Cells and Development, as well as on the
Online Completion
Use this page to review the questions and answers. Return to
www.ineedce.com and sign in. If you have not previously purchased
the program select it from the "Online Courses" listing and complete the
online purchase. Once purchased the exam wil be added to your Archives page where a Take Exam link will be provided. Click on the "Take Exam" link, complete all the program questions and submit your answers. An im-mediate grade report wil be provided and upon receiving a passing grade your "Verification Form" wil be provided immediately for viewing and/or printing. Verification Forms can be viewed and/or printed anytime in the future by returning to the site, sign in and return to your Archives Page.
1. The majority of orthodontic cases in 1999 11. In the permanent dentition, root
22. Selective partial decortication of the
were for comprehensive therapy, with
resorption can be associated with
cortical plates has been found to increase
81.5% of these in the 10–19 age group.
the speed of tooth movement during
b. inappropriate orthodontic forces
2. Patients may elect to forego orthodontic
c. inappropriate use of internal bleaching agents
treatment due to the .
d. all of the above
a. cost of treatment
12. Bone responds to low magnitude strain
b. duration of treatment
with many cycles or high-frequency
23. Temporary anchorage devices produce
c. rapid results achieved
vibrations, resulting in an increase in
relative skeletal anchorage.
3. Dental professionals may reject patients
for orthodontic treatment due to an
assessment that the patient will be
24. Cyclic forces _.
13. The use of anti-inflammatories may
noncompliant with treatment or non-
reduce orthodontic tooth movement.
a. change magnitude rapidly and repeatedly
compliant with oral hygiene requirements
b. affect the cells with each oscillation of force
during orthodontic treatment.
c. are oscillatory in nature
d. all of the above
14. The mechanical forces during orth-
odontic treatment result in _.
4. Simple orthodontic cases can only be
25. Research has demonstrated that the use
a. tissue-borne mechanical stresses
successfully treated with fixed orthodontic
b. cell-borne mechanical stresses
of cyclic forces increases the rate of bone
c. the induction of interstitial fluid flow
remodeling compared to static forces.
d. all of the above
15. Lengthy orthodontic treatment is more
5. Removable appliances offer the advantage
likely to elicit aberrant root resorption.
26. A device using cyclic forces was
a. being able to be removed for oral hygiene
introduced to relieve the discomfort
b. simplifying compliance
16. Osteoclasts develop bone matrix and
associated with orthodontic adjustments
c. simplifying oral home care
maintain the bone's structure.
and was found to be safe and effective.
6. Clear, full-coverage, removable resin
appliances are not indicated for all types
17. The bone remodeling process associ-
of cases.
ated with orthodontic movement is an
27. An orthodontic device using cyclic
inflammatory process.
forces has been found to _.
a. speed up orthodontic movements
7. The ability to successfully bond
b. slow down orthodontic movements
orthodontic brackets to teeth has
18. The response of bone to a long-
c. be safe and effective
duration static load _.
a. removed the need to utilize banding
a. decreases over time
b. improved aesthetics during treatment
b. increases over time
28. Cells are known to respond more read-
c. reduced discomfort for patients
c. remains the same over time
ily to rapid oscillation in force magnitude
d. all of the above
d. none of the above
than to constant forces.
8. The application of _ force is
19. The staging of orthodontic tooth
the premise for orthodontic tooth move-
movements based on linear and rotational
a. has enabled simultaneous movement of all teeth
29. Anabolic effects involve the metabolic
b. results in more space between the teeth during
breakdown of tissues, such as bone or
d. none of the above
c. reduces the duration of treatment
muscle, or complex molecules.
9. Orthodontic treatment duration is
d. all of the above
influenced by _.
20. Removable appliances can be success-
a. the amount and type of force applied to the teeth
fully used for all orthodontic cases.
b. the complexity of the case
30. Reducing the duration of treatment
c. the type of appliance used
with effective and safe techniques, and
d. all of the above
21. _ may speed up orthodontic
improving aesthetics during treatment,
10. Bone is known to adapt to mechanical
treatment.
increases the acceptability of orthodontic
forces, including weight-bearing loads
a. Molecular devices
and orthodontic (therapeutic) forces.
treatment for patients.
b. Permanent anchorage devices
c. Surgical orthodontic procedures
Advances in Orthodontic Treatment
Telephone: Home ( )
Requirements for successful completion of the course and to obtain dental continuing education credits: 1) Read the entire course. 2) Complete all information above. 3) Complete answer sheets in either pen or pencil. 4) Mark only one answer for each question. 5) A score of 70% on this test will earn you 4 CE credits. 6) Complete the Course Evaluation below. 7) Make check payable to PennWell Corp.
If not taking online, mail completed answer sheet to
Academy of Dental Therapeutics and Stomatology,
1. Know the reasons patients request orthodontic treatment, as well as the reasons they may reject orthodontic treatment
A Division of PennWell Corp.
P.O. Box 116, Chesterland, OH 44026
2. Know the biomechanics involved in orthodontic tooth movement
or fax to: (440) 845-3447
3. Know the factors that can increase the duration of orthodontic treatment
For ImmeDIATe results,
4. Understand the role static and cyclic forces play in biomechanics and the potential duration of orthodontic treatment
go to www.ineedce.com to take tests online.
Answer sheets can be faxed with credit card payment to
(440) 845-3447, (216) 398-7922, or (216) 255-6619.
�Payment of $59.00 is enclosed.
Please evaluate this course by responding to the following statements, using a scale of Excellent = 5 to Poor = 0.
(Checks and credit cards are accepted.)
If paying by credit card, please complete the
1. Were the individual course objectives met?
Objective #1: Yes No Objective #3: Yes No
following: MC Visa AmEx Discover
Objective #2: Yes No Objective #4: Yes No
2. To what extent were the course objectives accomplished overall? 5
Charges on your statement will show up as PennWell
3. Please rate your personal mastery of the course objectives.
4. How would you rate the objectives and educational methods?
5. How do you rate the author's grasp of the topic?
6. Please rate the instructor's effectiveness.
7. Was the overall administration of the course effective?
8. Do you feel that the references were adequate?
9. Would you participate in a similar program on a different topic?
10. If any of the continuing education questions were unclear or ambiguous, please list them.
11. Was there any subject matter you found confusing? Please describe.
12. What additional continuing dental education topics would you like to see?
PLEASE PHOTOCOPY ANSWER SHEET FOR ADDITIONAL PARTICIPANTS.
AUTHOR DISCLAIMER
COURSE CREDITS/COST
Dr. Jeremy Mao has an interest in OrthoAccel.
All questions should have only one answer. Grading of this examination is done
All participants scoring at least 70% (answering 21 or more questions correctly) on the
PennWell maintains records of your successful completion of any exam. Please contact our
manually. Participants will receive confirmation of passing by receipt of a verification
examination will receive a verification form verifying 4 CE credits. The formal continuing
offices for a copy of your continuing education credits report. This report, which will list
form. Verification forms will be mailed within two weeks after taking an examination.
education program of this sponsor is accepted by the AGD for Fellowship/Mastership
all credits earned to date, will be generated and mailed to you within five business days
This course was made possible through an unrestricted educational grant from
credit. Please contact PennWell for current term of acceptance. Participants are urged to
OrthoAccel Technologies, Inc. No manufacturer or third party has had any input into
EDUCATIONAL DISCLAIMER
contact their state dental boards for continuing education requirements. PennWell is a
the development of course content. All content has been derived from references listed,
The opinions of efficacy or perceived value of any products or companies mentioned
California Provider. The California Provider number is 4527. The cost for courses ranges
and or the opinions of clinicians. Please direct all questions pertaining to PennWell or
in this course and expressed herein are those of the author(s) of the course and do not
from $49.00 to $110.00.
Any participant who is not 100% satisfied with this course can request a full refund by
the administration of this course to Machele Galloway, 1421 S. Sheridan Rd., Tulsa, OK
necessarily reflect those of PennWell.
contacting PennWell in writing.
74112 or [email protected].
Many PennWell self-study courses have been approved by the Dental Assisting National
Completing a single continuing education course does not provide enough information
Board, Inc. (DANB) and can be used by dental assistants who are DANB Certified to meet
2009 by the Academy of Dental Therapeutics and Stomatology, a division
COURSE EVALUATION and PARTICIPANT FEEDBACK
to give the participant the feeling that s/he is an expert in the field related to the course
DANB's annual continuing education requirements. To find out if this course or any other
We encourage participant feedback pertaining to all courses. Please be sure to complete the
topic. It is a combination of many educational courses and clinical experience that
PennWell course has been approved by DANB, please contact DANB's Recertification
survey included with the course. Please e-mail all questions to: [email protected].
allows the participant to develop skills and expertise.
Department at 1-800-FOR-DANB, ext. 445.
Source: http://acceledent.co.uk/images/uploads/4A-i-Continuing-Education-Peer-Reviewed-Advances-in-Ortho-Treatment1.pdf
Gemeindeseite vom 1. März 2008 Gemeinde Sevelen Gemeinderatsverhandlungen vom 25. Februar 2008 Direkt unter Gemeindewappen platzieren: Kontaktstunde mit dem Gemeindepräsidenten für jedermann Datum und Zeit: Dienstag, 4. März 2008, 17.00 bis 18.00 Uhr Rathaus Sevelen, 1. OG,
Medicina, Psicologia, Biologia, Normativa e Scienze varie: tutto cio' che fa cultura SCIENZA E PROFESSIONE Anno 7 numero 10 Sospeso il Rosiglitazone (Avandia, Avandamet Avaglim) Incertezze sul rapporto rischio-beneficio. I pazienti dovranno essere guidati a modificare la cura, ma senza allarmismi. Multe effettuate sclerosi multipla Nulle dal 2007 in vero utile se il can-