Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Pii: s0002-9149(98)01016-9
Potential Benefit of Biventricular Pacing
in Patients with Congestive Heart Failure
and Ventricular Tachyarrhythmia
Christoph Stellbrink, MD, Angelo Auricchio, MD, Bjo¨rn Diem, MD,
Ole-Alexander Breithardt, MD, Michael Kloss, MD, Friedrich A. Scho¨ndube, MD, PhD,
Helmut Klein, MD, Bruno J. Messmer, MD, and Peter Hanrath, MD
Treatment of congestive heart failure (CHF) aims for
class I: 50.8 6
13.6 years, p <0.001 each) and mean
symptomatic relief and reduction of mortality both from
QRS duration was longer with advanced CHF (NYHA
sudden death and pump failure. The implantable car-
class III 127.8 6
30 msec; class II 119.4 6
27.7 msec;
dioverter defibrillator (ICD) is highly effective in the pre-
class 0 –I: 103.9 6
17.7 msec, p <0.001, analysis of
vention of sudden death, but no mortality benefit in
variance) as was the mean PR interval (NYHA class III
advanced CHF has yet been shown. Biventricular pacing
189.9 6
33.5 msec; class II 176.1 6
29.3 msec; class 0–I
may lead to functional improvement in selected patients
162.7 6
45.9 msec, p <0.001, analysis of variance). The
with CHF. Thus, a biventricular pacemaker with defibril-
incidence of atrial fibrillation was higher in class III (25.5%)
lation capabilities may be ideal for patients with ad-
compared with class 0–I (16.9%) and class II patients
vanced CHF. We retrospectively analyzed the data from
(14.1%, p 5
0.043, chi-square test). A total of 28 patients
384 patients (age 59 6
12 years, 322 male and 62
(7.3%) fulfilled eligibility criteria for biventricular pacing if
female) with regard to New York Heart Association
NYHA class III patients were considered candidates and 48
(NYHA) CHF class, mean QRS duration, mean PR inter-
val, presence of a QRS >120 msec and incidence of
(12.5%) if patients with NYHA II CHF and ejection fraction
<
atrial fibrillation at the time of ICD implantation. Based
30% were included. Thus, biventricular pacing may offer
on eligibility criteria from studies in biventricular pacing,
a promising therapeutic approach for a significant propor-
we analyzed how many patients may benefit from
tion of patients with CHF at risk for ventricular
biventricular pacing. Patients with CHF were older
tachyarrhythmia. Q
1999 by Excerpta Medica, Inc.
(NYHA class III: 60.9 6
9.7, class II: 61.3 6
10 versus
Am J Cardiol 1999;83:143D–150D
Congestive heart failure (CHF) is one of the major an ICD with left or biventricular pacing capabilities
healthcare problems in the world, afflicting 2– 4
may be an attractive therapy for patients with CHF at
million people in the United States and nearly 15
risk for ventricular tachyarrhythmia. Therefore, we
million people worldwide.1–3 The incidence of heart
analyzed the number of patients with an ICD indica-
failure is age dependent: 1–5 per 1,000 population
tion who may be candidates for left or biventricular
each year in the total population to as high as 30 – 40
pacing as an adjunct therapy for CHF.
per 1,000 population each year in people $75 years ofage.2,4 Thus, in an aging society, the prevalence of
PATIENTS AND METHODS
heart failure is increasing despite a reduction in car-
The databases of 2 university hospitals (University
diovascular mortality: in the United States, there was
of Aachen and University of Magdeburg, Germany)
a net growth of the CHF population of 428,000 pa-
were retrospectively analyzed with regard to the clin-
tients in 1990.5 Mortality from CHF remains high: in
ical and electrocardiographic parameters at the time of
the Framingham study the 5-year survival rate from
implantation in 384 consecutive patients who under-
the time of diagnosis was ,40%. Sudden cardiac
went ICD implantation at both institutions. There
death—mostly caused by ventricular tachyarrhyth-
were 322 men (84%) and 62 women (16%). The mean
mia—is a major threat to CHF patients and can be
age at implantation was 59 6 12 years. Underlying
effectively prevented with the implantable cardio-
heart disease was coronary artery disease in 264
verter defibrillator (ICD). However, medical treatment
(68.8%), dilated cardiomyopathy in 71 (18.5%), idio-
remains the most common therapeutic approach for
pathic ventricular fibrillation in 20 (5.2%), arrhythmo-
symptomatic relief. Recent data suggest that left or
genic right ventricular dysplasia in 8 (2.1%), valvular
biventricular pacing therapy may have the potential to
heart disease in 11 (2.9%), and other in 10 patients
improve the functional status of CHF patients. Thus,
(2.6%). Mean left ventricular ejection fraction as de-termined
38.3 6 15.4%. Indication for ICD implantation was
From the Department of Cardiology and Internal Medicine and the
aborted sudden cardiac death in 135 (35.2%), recur-
Department of Thoracic and Cardiovascular Surgery, University of
rent sustained ventricular tachycardia in 162 (42.2%),
Technology, Aachen, Germany; and Department of Cardiology and
and both in 56 patients (14.6%). Recurrent syncope
Internal Medicine, Otto Guericke Universita¨t, Magdeburg, Germany.
with inducible sustained ventricular tachycardia was
Address for reprints: Christoph Stellbrink, MD, Medizinische Klinik
present in 15 patients (3.9%) and nonsustained ven-
I, Universita¨tsklinikum der RWTH Aachen, Pauwelsstr. 30, D-52072Aachen, Germany.
tricular tachycardia with inducible but nonsuppress-
1999 by Excerpta Medica, Inc.
All rights reserved.
TABLE I Inclusion and Exclusion Criteria of the Pacing Therapies for Congestive Heart
Failure (PATH-CHF) Trial
Inclusion Criteria
Exclusion Criteria
CHF NYHA functional class III–IV (.6 mo) Life expectancy ,6 mo
Dilated cardiomyopathy (any etiology)
QRS $120 msec ($2 leads)
AF within the last 6 mo
PR interval $150 ms
History of sustained VT/VF*
Ability to tolerate anesthesia/surgery
Patient on optimal individual drug therapy Pacemaker indication
Sinus rate .55 beats/min
Angina pectoris CCS class III–IV
Able to perform CPX testing
Unexplained syncope*
Concomitant cardiac surgery
Renal insufficiency requiring hemodialysis
MI within the last 3 months
Patients dependent on IV inotropes
Previous valve replacement or reconstruction*
Severe aortic or mitral valve disease
AF 5 atrial fibrillation; CCS 5 Canadian Cardiac Society; CHF 5 congestive heart failure; COPD 5 chronic
obstructive pulmonary disease; CPX 5 cardiopulmonary exercise testing; FEV1 5 forced expiratory volume in 1second; HOCM 5 hypertrophic obstructive cardiomyopathy; ICD 5 implantable cardioverter defibrillator; IV 5intravenous; MI 5 myocardial infarction; NYHA 5 New York Heart Association; VF 5 ventricular fibrillation;VT 5 ventricular tachycardia.
*Not used for eligibility analysis.
ible sustained ventricular tachycardia in late postin-
farction patients in 16 patients (4.2%). The incidence
Table II summarizes the results for the patients in
of symptomatic CHF (New York Heart Association
the different functional stages of CHF. Both patient
[NYHA] class $2) was 82% (315 patients). All pa-
groups with CHF were significantly older than those
tients were analyzed with regard to the presence of
without functional limitation (p ,0.001 each com-
clinical criteria making them potential candidates for
pared with class 0 –I). The incidence of coronary ar-
bi- or left ventricular pacing at the time of ICD im-
tery disease was also significantly higher in patients
plantation. The criteria were chosen based on the
with CHF than in those without, although there was no
inclusion criteria of the Pacing Therapies for Conges-
difference between patients in NYHA class II or III. In
tive Heart Failure (PATH-CHF) study6 (Table I).
contrast, there was a further increase in the percentage
Some exclusion criteria were not used because they
of patients with nonischemic cardiomyopathy when
were not applicable to ICD patients or were specified
class III patients were compared with those with only
for some of the features of the PATH-CHF study
mild heart failure. Not unexpectedly, left ventricular
design. The same analysis was performed with inclu-
ejection fraction was significantly lower with ad-
sion of patients with NYHA class II heart failure, but
vanced stages of CHF (p ,0.001 for each individualcomparison). Conversely, the incidence of patients
with severely depressed left ventricular ejection frac-
with a QRS .120 msec showed a significant increase
tion (#30%). For group comparison, patients were
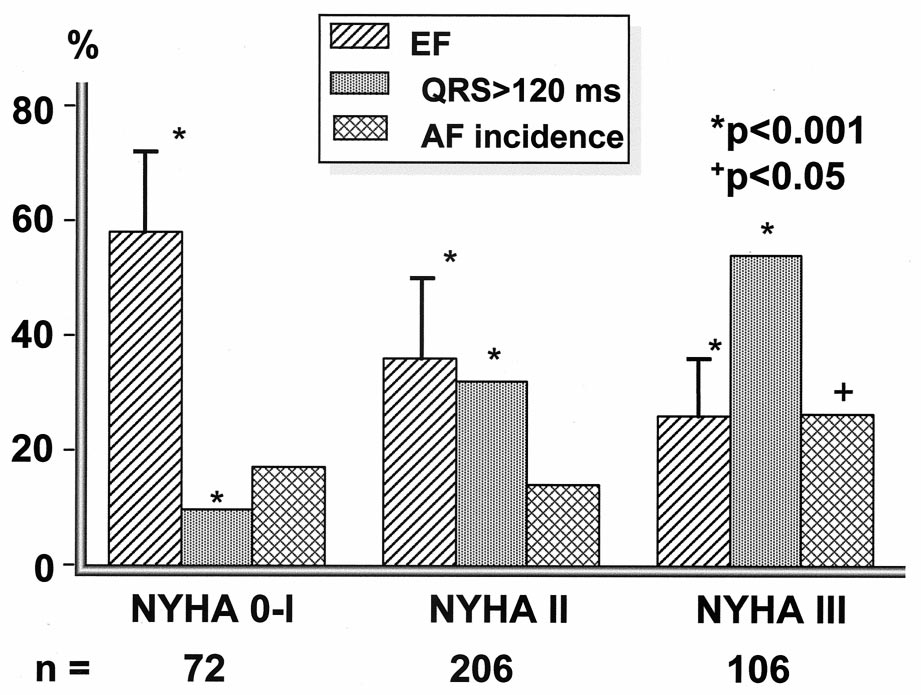
from 9.7% in class 0 –I to 52.8% in class III (Figure
stratified into 3 groups according to their functional
1). Of the patients with intraventricular conduction
class of CHF at the time of implantation as judged by
delay, a QRS width of .150 msec was present in 48
the implanting physician: patients with no signs of
of all 129 patients with QRS prolongation (37%): 3 of
CHF (NYHA class 0 –I), patients with mild CHF
7 patients in NYHA class 0 –I (43%), 26 of 66 in class
(NYHA class II), and patients with moderate-to-se-
II (39%), and 19 of 56 in class III (34%). The inci-
vere heart failure (NYHA class III). All electrocardio-
dence of atrial fibrillation was significantly higher in
grams were reviewed by 2 independent observers.
patients of NYHA class III CHF compared with pa-
Mean age, left ventricular ejection fraction, resting
tients with no or mild heart failure (p ,0.05), but no
heart rate, and PR and QRS interval were compared
significant difference was observed between patients
using analysis of variance. When significant differ-
with class 0 –I or class II (Figure 1). Mean QRS duration
ences were present, individual groups were compared
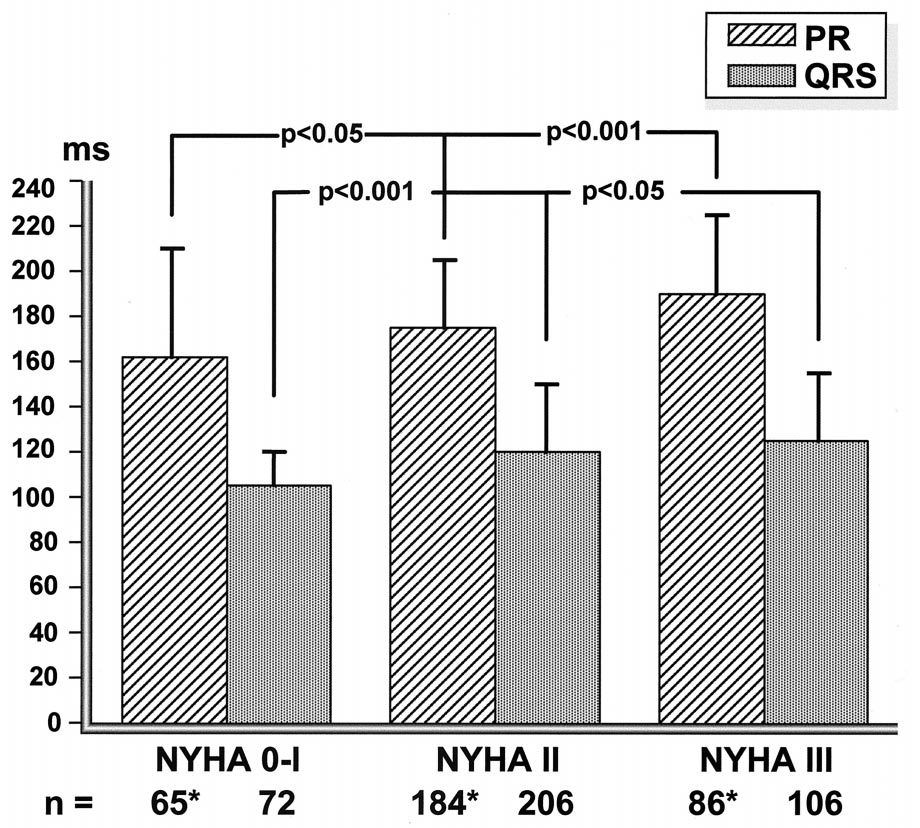
and PR interval also significantly increased with ad-
using a 2-tailed paired
t test. Gender proportion, inci-
vanced functional class of heart failure (Figure 2). In
dence of coronary artery disease and dilated cardio-
class III patients, mean heart rate at rest was significantly
myopathy, incidence of atrial fibrillation, and a QRS
higher compared with class II patients (p 5 0.006) and
width of .120 msec were compared using a chi-
patients in class 0 –I (p 5 0.01, Table II).
square test. Values of p ,0.05 were considered sta-
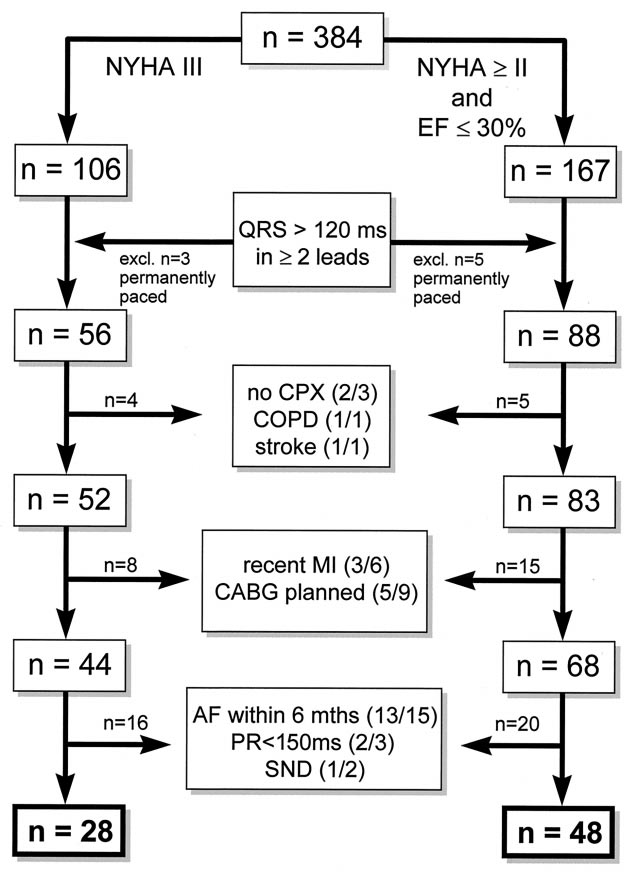
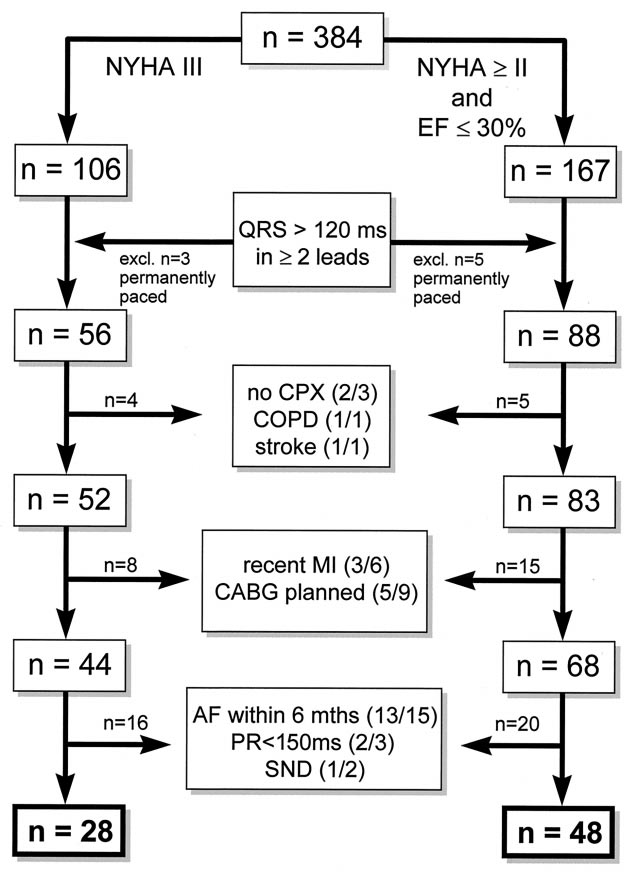
The eligibility analysis for left or biventricular
pacing is outlined in Figure 3. There were 106 patients
144D THE AMERICAN JOURNAL OF CARDIOLOGYT
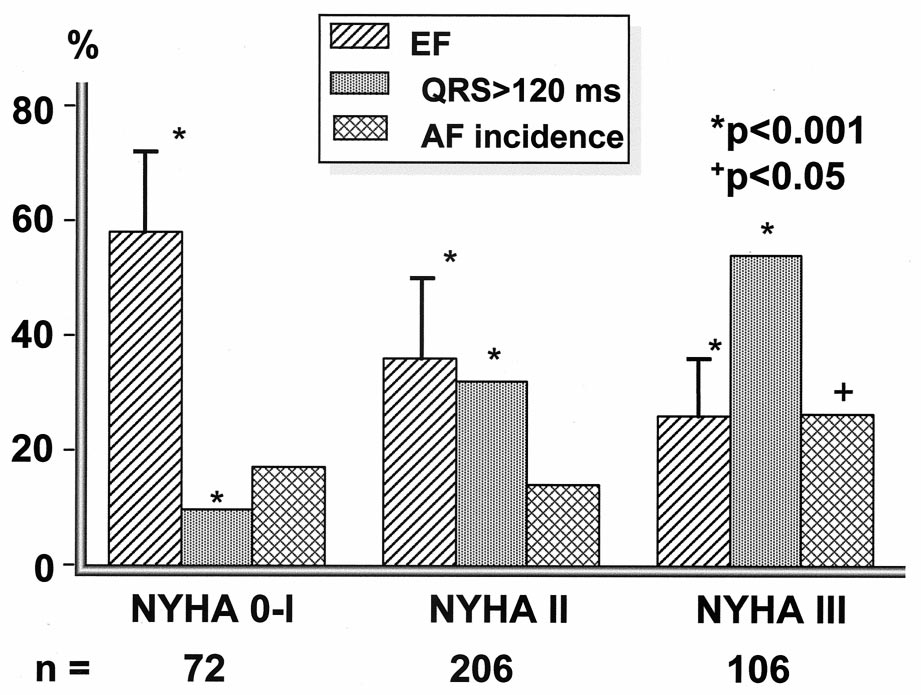
TABLE II Presence of Electrocardiographic Abnormalities in Implantable Cardioverter Defibrillator Patients According to New York
Heart Association (NYHA) Class
Incidence of CAD (%)
Incidence of DCM (%)
Heart rate (beats/min 6 SD)
Incidence of AF (%)‡
PR interval (ms 6 SD)
QRS width (ms 6 SD)
AF 5 atrial fibrillation; CAD 5 coronary artery disease; DCM 5 dilated cardiomyopathy; LVEF 5 left ventricular ejection fraction; NS 5 not significant; SD 5
standard deviation.
*By analysis of variance.
†Chi-square test.
‡Within the last 6 months before implant.
with NYHA class III heart failure. Of these, 56 had a
vere chronic obstructive pulmonary disease that
QRS of .120 msec in at least 2 surface electrocar-
limited his cardiopulmonary performance and 1 pa-
diographic leads. Two patients had to be excluded
tient had a previous disabling stroke. Of the remaining
because they were unable to perform significant exer-
52 patients, 8 were excluded because either they had a
cise due to noncardiac reasons as assessed by cardio-
recent myocardial infarction (n 5 3), or a surgical
pulmonary exercise testing (1 patient after leg ampu-
revascularization was planned in addition to ICD im-
tation, 1 patient with coxarthrosis); 1 patient had se-
plantation (n 5 5). These were excluded because
FIGURE 1. Comparison of mean left ventricular ejection fraction, incidence of QRS prolongation
>120 msec, and atrial fibrillation between different stages of congestive heart failure
(n 5 384). Mean left ventricular ejection fraction (EF), incidence of QRS width >120 msec (in
>2 surface electrocardiographic leads) and incidence of atrial fibrillation (AF) in patients with
no or minimal (New York Heart Association [NYHA] 0 –I), mild-to-moderate (NYHA II), and
severe (NYHA III) heart failure are shown. Mean EF significantly decreased with advanced
stages of heart failure. Conversely, there was a significant increase in QRS duration. The AF
incidence was highest in NYHA III patients, whereas there was no significant difference be-
tween class 0 –I and class II. See text for statistical analysis.
A SYMPOSIUM: ELECTRICAL MANAGEMENT OF CARDIAC DISORDERS
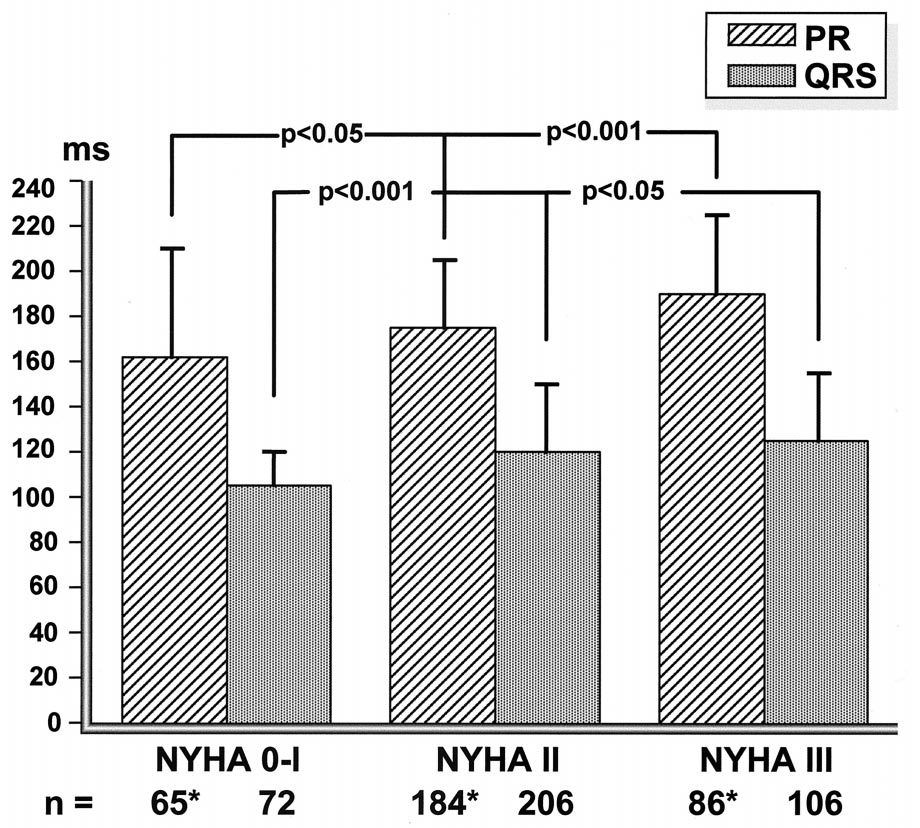
FIGURE 2. Mean PR interval and QRS duration depending on the New York Heart Association
(NYHA) functional class (n 5 384). Mean PR interval and QRS width are shown for the differ-
ent stages of heart failure. Both PR interval and QRS width significantly increased with in-
creasing functional heart failure class. * Denotes the number of patients analyzed after exclu-
sion of patients with atrial fibrillation or permanent pacing in the ventricle. See text for statisti-
cal analysis.
some degree of functional improvement could be ex-
of CHF14 (Table III). Ventricular tachyarrhythmia has
pected due to resolving myocardial stunning after the
been implicated as the underlying mechanism for sud-
recent infarct or due to improvement of cardiac func-
den death in ;80% of ambulatory patients in whom
tion after restoration of blood supply by surgical re-
Holter recordings could be obtained at the time of
vascularization. Finally, 16 patients were excluded
death.15–22 However, in patients with CHF the inci-
because they had had atrial fibrillation within the last
dence of bradyarrhythmia and electromechanical dis-
6 months (n 5 13), had a PR interval of ,150 msec
sociation may be considerably higher.23 Nevertheless,
(n 5 2), or had some indication of sinus node dys-
ventricular arrhythmia is a frequent finding in patients
function (n 5 1). Thus, 28 patients remained as can-
with CHF, and nonsustained ventricular tachycardia
didates for pacing therapy for CHF equaling 7.3% of
observed on ambulatory Holter recordings has been
the total ICD population or 26.4% of all patients in
shown to be an independent predictor both of total
NYHA class III. If patients with NYHA class II heart
mortality9,24–26 and sudden cardiac death.27
failure and severely depressed left ventricular function
Role of medical treatment: Apart from reduction of
were included, the number increased to 48 patients
mortality, the second main goal of medical treatment
(12.5% of the ICD population, Figure 3).
of CHF is functional improvement. Digitalis is com-
monly prescribed in patients with CHF, and it has
Mortality and sudden death in CHF: Mortality from
been shown that withdrawal of digoxin leads to wors-
CHF is mainly caused by progressive pump failure
ening of symptoms.28,29 However, there seems to be
and sudden death and strongly depends on the func-
no positive effect on mortality.30 Similarly, diuretics
tional stage of CHF: patients with mild CHF, i.e.,
may play a role for symptomatic relief only.31 Angio-
NYHA class II, have a 1-year mortality of 5–15%,7,8
tensin-converting enzyme inhibitors not only lead to
which increases to 20 –50% in class III patients.9–11 In
symptomatic improvement in patients with CHF but
class IV patients, which make up approximately 10 –
also decrease mortality, both in patients with left ven-
15% of the heart failure population, the outcome is
tricular dysfunction and CHF 7,13 and in patients with
least favorable, with a 1-year mortality exceeding
postinfarction CHF.32–34 However, it is still unclear
50%.12,13 The proportion of sudden deaths in relation
whether these agents also decrease the sudden cardiac
to total mortality decreases with worsening symptoms
death rate: in nonselected CHF populations, no signif-
146D THE AMERICAN JOURNAL OF CARDIOLOGYT
is general agreement that class I agents should not beused in CHF patients. In contrast, several studies fromthe prethrombolytic era have shown improved overallsurvival and a reduction of sudden death in postin-farction patients receiving b-blocker treatment.38–40In a recent survey of .200,000 patients with myocar-dial infarction, this beneficial effect was also presentin patients who received thrombolytic treatment; pa-tients with left ventricular dysfunction and symptomsof CHF had the same benefit from b-blocker treatmentas patients with well-preserved left ventricular func-tion.41 In fact, some data suggest that b-blocker treat-ment (if tolerated in the run-in phase) may decreasemortality in patients with mild-to-moderate heart fail-ure.42 However, few data are, as yet, available onpatients with severe CHF. Nevertheless, b blockersare being increasingly used as a therapeutic alternativein CHF. The class III agent amiodarone has failed toshow significant improvement in overall survival inhigh-risk postinfarction patients, despite a significantreduction of arrhythmic or sudden death.43,44 A sig-nificant mortality reduction was shown for a popula-tion of patients with predominantly nonischemicCHF,45 whereas there seems to be no significant re-duction of mortality in ischemic cardiomyopathy.46 Ina meta-analysis of 13 postinfarction and CHF trialswith amiodarone, a small, marginally significant re-duction of total mortality could be demonstrated.47However, the investigators stated that confirmation of
FIGURE 3. Analysis of eligibility for pacing therapy in congestive
these results by a single, large-scale trial would be
heart failure (CHF). This graph illustrates the eligibility analysis
desirable. Thus, it may be concluded that amiodarone
process both for patients with New York Heart Association
can be safely administered to patients with CHF at risk
(NYHA) class III CHF (left ) and after inclusion of patients with
for sustained ventricular tachyarrhythmia, although a
NYHA class II CHF and a left ventricular ejection fraction (EF)
clear mortality benefit has not been demonstrated.
<30% (right ). Numbers above arrows refer to the patients ex-
Pooled data from several studies do not show a reduc-
cluded for NYHA class III and NYHA class II—EF <30%.
AF
tion in mortality with the use of calcium antagonists in
5 atrial fibrillation; CABG 5 coronary artery bypass
surgery; COPD 5 chronic obstructive pulmonary disease; CPX 5
patients after myocardial infarction.48 There is, as yet,
cardiopulmonary exercise test; MI 5 myocardial infarction;
only 1 randomized, prospective study that showed an
SND 5 sinus node dysfunction.
improved outcome with the calcium antagonist amlo-dipine49 in patients with advanced CHF. Moreover,there seems to be some functional improvement with
icant decrease of the sudden death incidence with
diltiazem in idiopathic CHF.50
angiotensin-converting enzyme inhibitors was ob-
Role of the ICD in CHF: The Antiarrhythmics Versus
served,7,13 whereas in trials including postinfarction
Implantable Defibrillators (AVID) trial has shown im-
patients who had left ventricular dysfunction with
proved survival with the implantable defibrillator in
predominantly mild CHF, the incidence of sudden
patients who have either survived sudden cardiac
death was significantly lower in the treated group.34,35
death or in patients with sustained, hemodynamically
Class I antiarrhythmic agents have been shown to
compromising ventricular tachycardia and decreased
increase mortality after myocardial infarction,36 and in
left ventricular function51; similar results have been
patients with CHF and atrial fibrillation.37 Thus, there
reported for the Canadian Implantable DefibrillatorStudy (CIDS)52 and Cardiac Arrest Study Hamburg(CASH)53 studies (publication of final results pend-ing). The Multicenter Automatic Defibrillator Implan-
TABLE III Sudden Death Dependent on the Severity of
Congestive Heart Failure
tation Trial (MADIT)54 focused on primary preven-tion of sudden death in patients with decreased left
ventricular function in the chronic state after myocar-
dial infarction, nonsustained VT noted on Holter re-
cording, and inducible but nonsuppressible VT during
invasive electrophysiologic study. This study also
showed a reduction of total mortality in patients
NYHA 5 New York Heart Association.
treated with an ICD compared with medical treatment,
Reproduced with permission from J Am Coll Cardiol.14
consisting mainly of amiodarone. However, total mor-
A SYMPOSIUM: ELECTRICAL MANAGEMENT OF CARDIAC DISORDERS
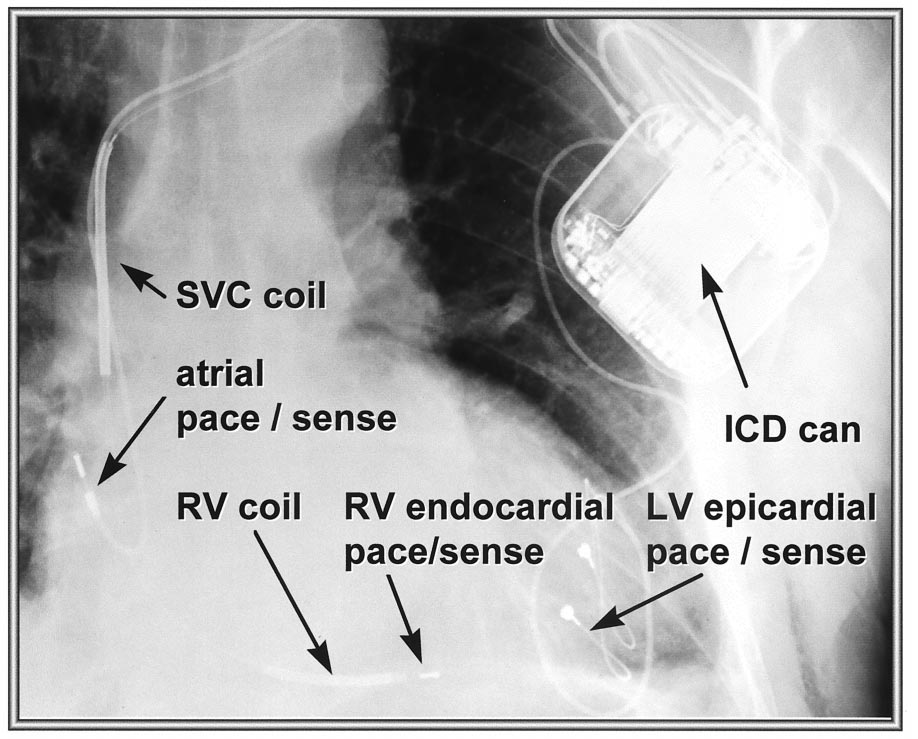
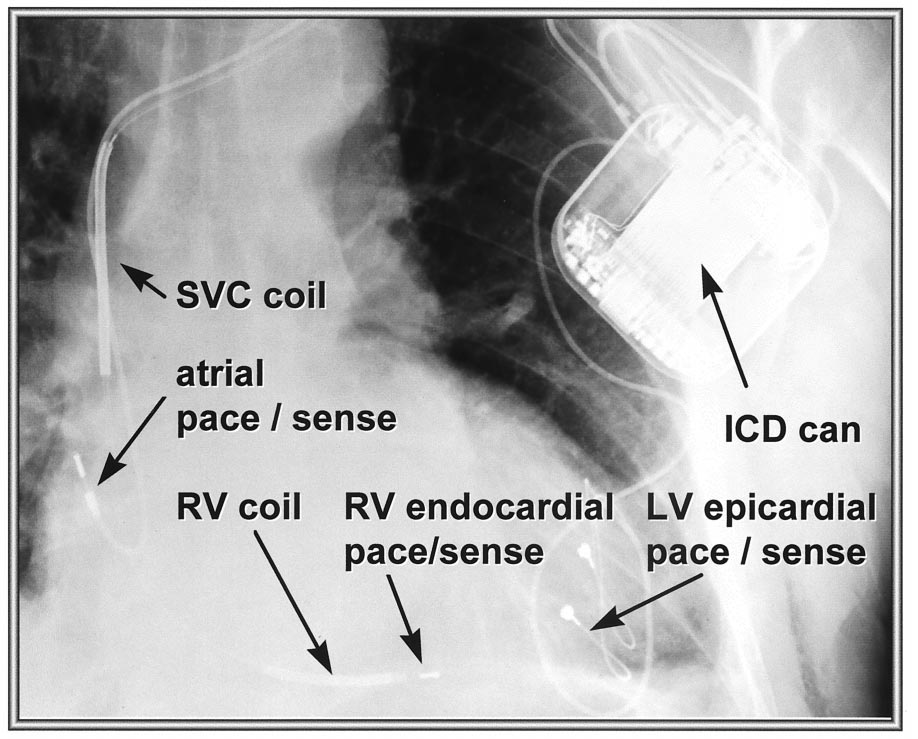
FIGURE 4. Radiograph of biventricular ICD. Anteroposterior view of a pectorally implanted ICD
in a patient with ventricular tachyarrhythmia, congestive heart failure, and a widened QRS
complex. The defibrillation lead and the atrial lead are placed conventionally via the left sub-
clavian vein in the right ventricle and atrium, respectively. An additional bipolar lead is placed
epicardially via a small lateral thoracotomy on the left ventricular free wall. The atrial lead is
used for triggering of biventricular pacing to optimize atrioventricular delay (VDD mode).
ICD 5 implantable cardioverter defibrillator; LV 5 left ventricle; RV 5 right ventricle;
SVC 5 superior vena cava.
tality remains high in patients with CHF and an im-
late into chronic functional improvement is currently
planted ICD.55 Moreover, in a nonrandomized study
being investigated in several studies, such as the
by Sweeney et al,56 the ICD did not improve survival
PATH-CHF,6 the Vigor-CHF,69 and the Multisite
in patients with endstage CHF awaiting heart trans-
Stimulation in Cardiomyopathy (MUSTIC) trial.70
plantation despite a reduction of sudden death. Thus,
Notably, Saxon et al69 demonstrated a reduction of
the concern remains that, in patients with advanced
plasma norepinephrine levels in CHF patients with
CHF, conventional ICD treatment may simply convert
biventricular pacing, a finding that may have impor-
the mode of death from arrhythmic death to pump
tant prognostic implications in this subset of patients,
if it can be confirmed in larger studies. A recent
Pacing for CHF: There are few data available on the
analysis in a CHF clinic population estimated that
effect of pacing therapy on cardiac pump function.
about 6% of all CHF patients fulfill the eligibility
Hochleitner et al59 showed substantial functional im-
criteria of the PATH-CHF study and may, therefore,
provement in patients with CHF treated with conven-
potentially benefit from this therapeutic approach,71 a
tional dual-chamber pacing (using right ventricular
proportion of patients that would increase to 13% if
apical pacing). In an acute study, Auricchio et al60
patients with atrial fibrillation could be included and
demonstrated hemodynamic improvement in CHF pa-
the pacemaker had defibrillation capabilities.
tients when the atrioventricular delay was optimized,
Potential for a biventricular ICD: Figure 4 shows a
2 other studies found similar results.61,62 However,
radiographic image of an implanted ICD with addi-
these data were challenged by other investigators who
tional left ventricular pacing leads for optimization of
did not observe any significant improvement.63–65
left ventricular function in a patient with advanced
More recently, interest in pacing for CHF was re-
CHF and a prolonged QRS complex. Based on the
newed by the idea that optimization of atrioventricular
available data on the potential benefit that left or
delay, as well as resynchronization of ventricular ac-
biventricular pacing may offer for CHF patients, it
tivation, may exert positive hemodynamic effects.
may be speculated that such a combined device may
This may be accomplished by finding the optimal
not only lead to a dramatic reduction in sudden death
pacing site(s) in the right or left ventricle. Both bi- and
but, due to functional improvement in a significant
left ventricular pacing have shown acute hemody-
number of patients with CHF, also decrease the po-
namic improvement in patients with a widened QRS
tential of conversion of the mode of death from sud-
complex at baseline.6,66–68 Whether these data trans-
den to pump failure death. Thus, with additional he-
148D THE AMERICAN JOURNAL OF CARDIOLOGYT
modynamic support, the ICD may eventually become
minor. In addition, ICD treatment seems to be more
an effective bridge to heart transplantation in patients
effective for primary prevention of sudden death in
with end-stage CHF. Moreover, a biventricular ICD
some high-risk subgroups. However, CHF remains the
may offer a new, effective therapy for the desperate
leading cause of death in patients with an implanted
patient with NYHA class IV CHF who is not a can-
ICD. Thus, there is great need for optimized care for
didate for transplantation and who is generally not
pump failure to prevent functional deterioration in
considered an ICD candidate because of his or her
ICD patients with CHF. Biventricular or left ventric-
extremely poor prognosis due to potential death from
ular pacing with optimized atrioventricular delay is a
pump failure. It seems reasonable to assume that a
new treatment modality that may improve functional
proportion of NYHA class IV patients may fulfill the
capacity and, thus, quality of life in a subgroup of
eligibility criteria comparable to the 26% of class III
CHF patients with intraventricular conduction delay.
patients in our series (most likely, there will be more
It may be speculated that pacing for heart failure
patients with QRS prolongation, but on the other hand,
combined with antitachycardia options may decrease
more patients with atrial fibrillation). Thus, there may
mortality in these patients with moderate-to-severe
be a significant number of class IV patients who may
CHF. Future studies will address the use of pacing in
benefit from additional pacing therapy for CHF. Pa-
patients with mild-to-moderate (NYHA class II) or
tients with severely depressed left ventricular function
more advanced (NYHA class IV) heart failure and
and yet only mild symptoms of CHF are currently
atrial fibrillation and may renew interest in the use of
being investigated in 2 trials: the Ventak-CHF trial in
the ICD as an electronic bridge to transplant.
the United States and the PATH-CHF II trial in Eu-
1. Eriksson H. Heart failure: a growing public health problem. J Intern Med
rope. Our data indicate that the percentage of patients
1995;237:135–141.
2. Ho KKL, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure:
who may benefit from pacing may almost double if
the Framingham study. J Am Coll Cardiol 1993;22(suppl A):6A–13A.
these patients are included. This number may even
3. Kannel WB, Belanger AJ. Epidemiology of heart failure. Am Heart J 1991;
121:951–957.
further increase if patients with atrial fibrillation can
4. Cowie MR, Mosterd A, Wood DA, Deckers JW, Poole-Wilson PA, Sutton GC,
be treated. In our series, including patients with atrial
Grobbee DE. The epidemiology of heart failure. Eur Heart J 1997;18:208 –225.
fibrillation would increase the number of eligible pa-
5. O'Connell JB, Bristow MR. Economic impact of heart failure in the United
States: time for a different approach. J Heart Lung Transplant 1993;13:S107–
tients to 10.7% (NYHA class III) and 16.4% (NYHA
class $II and an ejection fraction #30%), respec-
6. Auricchio A, Stellbrink C, Block M, Mortensen P, on behalf of the PATH-CHF
tively. Furthermore, patients with permanent need for
investigators. Clinical and objective improvements in severe congestive heartfailure patients using univentricular or biventricular pacing: preliminary results of
pacing were excluded in our series, and these may also
a randomized prospective study. (Abstr.) J Am Coll Cardiol 1998;31(2 suppl
be treated. However, there were only 5 patients ex-
A):31A.
7. The SOLVD Investigators. Effect of enalapril on survival in patients with
cluded for this reason. Thus, the group of patients with
reduced left ventricular ejection fractions and congestive heart failure. N Engl
additional need for antibradycardia pacing do not
J Med 1991;325:293–302.
seem to have an important impact on the ICD popu-
8. Gradman A, Deedwania P, Cody R, Massie B, Pitt B, Goldstein S. Predictors
of total mortality and sudden death in mild to moderate heart failure. J Am Coll
lation amenable to bi- or left ventricular pacing.
Cardiol 1989;14:564 –570.
9. Wilson JR, Schwartz JS, Sutton MS, Ferraro N, Horowitz LN, Reichek N,
Josephson ME. Prognosis in heart failure: relation to hemodynamic measure-ments and ventricular ectopic activity. J Am Coll Cardiol 1983;2:403– 410.
The analysis presented is retrospective and can
10. Kjekshus J. Arrhythmias and mortality in congestive heart failure. Am J
therefore only provide an idea of the percentage of
Cardiol 1990;65(suppl):42I– 48I.
11. Franciosa JA, Wilen M, Ziesche S, Cohn JN. Survival in men with severe
patients who may be candidates for pacing therapy in
chronic left ventricular failure due to either coronary heart disease or idiopathic
CHF. Patients who were denied ICD implantation for
dilated cardiomyopathy. Am J Cardiol 1983;51:831– 836.
clinical reasons were not analyzed. Moreover, most
12. Smith WM. Epidemiology of congestive heart failure. Am J Cardiol 1985;
55(suppl A):3A– 8A.
published data on pacing in CHF patients are limited
13. The CONSENSUS Trial Study Group. Effects of enalapril on mortality in
by small patient numbers and provide only data on
severe congestive heart failure: results of the Cooperative North Scandinavian
acute hemodynamic or short-term functional effects.
Enalapril Survival Study. N Engl J Med 1987;316:1429 –1435.
14. Uretsky BF, Sheahan RG. Primary prevention of sudden cardiac death in
Virtually no data are available for a biventricular ICD.
heart failure: will the solution be shocking? J Am Coll Cardiol 1997;30:1589 –
Therefore, prospective data in large patient cohorts
1597.
15. Nikolic G, Bishop RL, Singh JB. Sudden death recorded during Holter
with sufficient follow-up duration are necessary to
monitoring. Circulation 1982;66:218 –225.
determine the true role of pacing for CHF with regard
16. Savage DD, Castelli WP, Anderson SJ, Kannel WB. Sudden unexpected
to long-term functional improvement, the number of
death during ambulatory electrocardiographic monitoring. Am J Med 1983;74:148 –152.
patients that may need additional defibrillation
17. Lewis BH, Antman EM, Graboys TB. Detailed analysis of 24 hour ambula-
backup, and the effect of pacing on mortality in CHF.
tory electrocardiographic recordings during ventricular fibrillation or torsade des
pointes. J Am Coll Cardiol 1983;2:426 – 436.
18. Pratt CM, Francis MJ, Luck JC, Wyndham CR, Miller RR, Quinones MA.
Analysis of ambulatory electrocardiograms in 15 patients during spontaneous
Despite significant advances in the diagnosis and
ventricular fibrillation. J Am Coll Cardiol 1983;2:789 –797.
19. Panidis IP, Morganroth J. Sudden death in hospitalized patients. Cardiac
management of heart failure, mortality remains high.
rhythm disturbances detected by ambulatory electrocardiographic monitoring.
Medical treatment includes angiotensin-converting
J Am Coll Cardiol 1983;2:798 – 805.
enzyme inhibitors, diuretics, and b blockers as first-
20. Milner PG, Platia EV, Reid PR, Griffith LS. Ambulatory electrocardiographic
recordings at the time of fatal cardiac arrest. Am J Cardiol 1985;56:588 –592.
line drugs. Digitalis and some calcium antagonists
21. Bayes de Luna A, Coumel P, Leclercq JF. Ambulatory sudden cardiac death:
may offer additional benefit with regard to symptom-
mechanisms of production of fatal arrhythmia on the basis of data from 157 cases.
atic relief. Amiodarone is effective in decreasing sud-
Am Heart J 1989;117:151–159.
22. Olshausen KV, Witt T, Pop T, Treese N, Bethge KP, Meyer J. Sudden cardiac
den death, but its effect on total mortality may be
death while wearing a Holter monitor. Am J Cardiol 1991;67:381–386.
A SYMPOSIUM: ELECTRICAL MANAGEMENT OF CARDIAC DISORDERS
23. Luu M, Stevenson LW, Brunken RC, Drinkwater DC, Schelbert HR, Tillisch
48. Teo KK, Yusuf S, Furberg CD. Effects of prophylactic antiarrhythmic drug
JH. Diverse mechanisms of unexpected cardiac arrest in advanced heart failure.
therapy in acute myocardial infarction. JAMA 1993;270:1589 –1595.
49. Packer M, O'Connor CM, Ghali JK, Pressler ML, Carson PE, Belkin RN,
24. Birgersdotter-Green U, Rosenqvist M, Ryden L. Effect of congestive heart
Miller AB, Neuberg GW, Frid D, Wertheimer JH, Cropp AB, DeMets DL, for the
failure treatment on incidence and prognosis of ventricular tachyarrhythmias.
PRAISE Study Group. Effect of amlodipine on morbidity and mortality in severe
J Cardiovasc Pharmacol 1991;17(suppl)6:S53–S58.
chronic heart failure. N Engl J Med 1996;335:1107–1114.
25. Bigger JT, Flesiss JL, Kleiger R, Miller JP, Rolnitzky LM. The relationships
50. Figulla HR, Gietzen F, Zeymer U, Raiber M, Hegselmann J, Soballa R,
among ventricular arrhythmias, left ventricular dysfunction and mortality in the
Hilgers R, for the DiDi Study Group. Diltiazem improves cardiac function and
2 years after myocardial infarction. Circulation 1984;69:250 –258.
exercise capacity in patients with idiopathic dilated cardiomyopathy: results of
26. Hofmann T, Meinertz T, Kasper W, Geibel A, Zehender M, Hohnloser S,
the diltiazem in dilated cardiomyopathy trial. Circulation 1996;94;346 –352.
Stienen U, Treese N, Just H. Mode of death in idiopathic dilated cardiomyopathy:
51. The Antiarrhythmic Versus Implantable Defibrillator (AVID) Investigators.
a multivariate analyis of prognostic determinants. Am Heart J 1988;116:1455–1461.
A comparison of antiarrhythmic-drug therapy with implantable defibrillators in
27. Doval HC, Nul DR, Grancelli HO, Varini SD, Soifer S, Corrado G, Dubner
patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med
S, Scapin O, Perrone SV, for the GESICA Investigators. Nonsustained ventricular
tachycardia in severe heart failure. Independent marker of increased mortality due
52. Connolly SJ, Gent M, Roberts RS, Dorian P, Green MS, Klein GJ, Mitchell
to sudden death. Circulation 1996;94:3198 –3203.
LB, Sheldon RS, Roy D. Canadian Implantable Defibrillator Study (CIDS): study
28. Uretsky BF, Young JB, Shahidi E, Yellen LG, Harrison MC, Jolly K, on
design and organization. Am J Cardiol 1993;72(suppl):103F–108F.
behalf of the PROVED investigator group. Randomized study assessing the effect
53. Siebels J, Kuck KH, and the CASH Investigators. Implantable cardioverter
of digoxin withdrawal in patients with mild to moderate chronic congestive heart
defibrillator compared with antiarrhythmic drug treatment in cardiac arrest sur-
failure: results from the PROVED trial. J Am Coll Cardiol 1993;22:955–962.
vivors (the Cardiac Arrest Study Hamburg). Am Heart J 1994;127:1139 –1144.
29. Packer M, Gheorgiade M, Young JB, Constantini PJ, Adams KF, Cody RJ,
54. Moss AJ, Hall J, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH,
Smith LK, Van Voorhees L, Gourley LA, Jolly MK. Withdrawal of digoxin from
Saksena S, Waldo AL, Wilber D, Brown MW, Heo M. Improved survival with an
patients with chronic heart failure treated with angiotensin-converting-enzyme
implanted defibrillator in patients with coronary disease at high risk for ventric-
inhibitors. N Engl J Med 1993;329:1–7.
30.
ular arrhythmia. N Engl J Med 1996;335:1933–1940.
The Digitalis Investigative Group. The effect of digoxin on mortality and
morbidity in patients with heart failure. N Engl J Med 1997;336:525–533.
Kim SG, Maloney JD, Pinski SL, Choue CW, Ferrick KJ, Roth JA, Gross J,
31. Patterson JH, Adams KF Jr, Applefield MM, Corder CN, Masse BR. Oral
Brodman R, Furman S, Fisher JD. Influence of left ventricular function on
torasemide in patients with chronic congestive heart failure: effects on body
survival and mode of death after implantable defibrillator therapy (Cleveland
weight, edema and electrolyte excretion. Pharmacotherapy 1994;14:514 –521.
Clinic Foundation and Montefiore Medical Center experience). Am J Cardiol
32. Pfeffer MA, Braunwald E, Moye LA, Basta L, Brown EJ Jr, Cuddy TE, Davis
BR, Geltman EM, Goldman S, Flaker GC. Effect of captopril on mortality and
56. Sweeney MO, Ruskin JN, Garan H, McGovern BA, Guy ML, Torchiana DF,
morbidity in patients with left ventricular dysfunction after myocardial infarc-
Vlahakes GJ, Newell JB, Semigran MJ, Dee W. Influence of the implantable
tion—results of the survival and ventricular enlargement study. N Engl J Med
cardioverter/defibrillator on sudden death and total mortality in patients evaluated
1992;327:669 – 677.
for cardiac transplantation. Circulation 1995;92:3273–3281.
33. The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effect of
57. Kim SG. Implantable defibrillator therapy: does it really prolong life? How
ramipril on mortality and morbidity of survivors of acute myocardial infarction
can we prove it? Am J Cardiol 1993;71:1213–1218.
with clinical evidence of heart failure. Lancet 1993;2:821– 827.
58. Guarnieri T, Levine JH, Griffith LSC, Veltri EP. When sudden cardiac death
34. Kober L, Torp Pedersen C, Carlsen JE, Bagger H, Eliasen P, Lyngborg K,
is not so sudden: lessons learned from the automatic implantable defibrillator. Am
Videbaek J, Cole DS, Auclert L, Pauly NC. A clinical trial of the angiotensin-
Heart J 1988;115:205–207.
converting enzyme inhibitor trandolapril in patients with severe left ventricular
59. Hochleitner M, Hortnagl H, Ng C, Hortnagl H, Gschnitzer F, Zechmann W.
dysfunction after myocardial infarction. N Engl J Med 1995;333:1670 –1676.
Usefulness of physiologic dual-chamber pacing in drug resistant idiopathic di-
35. Ambrosioni E, Borghi C, Magnani B. The effect of the angiotensin-convert-
lated cardiomyopathy. Am J Cardiol 1990,66:198 –202.
ing enzyme inhibitor zofenopril on mortality and morbidity after prior myocardial
60. Auricchio A, Sommariva L, Salo RW, Scafuri A, Chiariello L. Improvement
infarction. N Engl J Med 1995;332:80 – 85.
of cardiac function in patients with severe congestive heart failure and coronary artery
36. Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, Barker AH,
disease with shortened AV delay. Pacing Clin Electrophysiol 1993;16:2034 –2043.
Arensberg D, Baker A, Friedman L, Greene HL. Mortality and morbidity in
61. Brecker SJD, Xiao HB, Sparrow J, Gibson DG. Effects of dual-chamber
patients receiving encainide, flecainide, or placebo: the Cardiac Arrhythmia
pacing with short atrioventricular delay in dilated cardiomyopathy. Lancet 1992;
Suppression Trial. N Engl J Med 1991;324:781–788.
340:1308 –1312.
37. Flaker GC, Blackshear JL, McBride R, Kronmal RA, Halperin JL, Hart RG,
62. Nishimura RA, Hayes DL, Holmes DR Jr, Tajik AJ. Mechanism of hemo-
on behalf of the Stroke Prevention in Atrial Fibrillation Investigators. Antiar-
dynamic improvement by dual-chamber pacing for severe left ventricular dys-
rhythmic drug therapy and cardiac mortality in atrial fibrillation. J Am Coll
function: an acute Doppler and catheterization hemodynamic study. J Am Coll
38. Norwegian Multicenter Study Group. Timolol-induced reduction in mortality
63. Linde C, Gadler F, Edner M, Nordlander R, Rosenqvist M, Ryden L. Results
and reinfarction in patients surviving acute myocardial infarction. N Engl J Med
of atrioventricular synchronous pacing with optimized delay in patients with
severe congestive heart failure. Am J Cardiol 1995;75:919 –923.
39. Betablocker Heart Attack Trial Research Group. A randomized trial of
64. Gold MR, Feliciano Z, Gottlieb SS, Fisher ML. Dual-chamber pacing with a
propanolol in patients with acute myocardial infarction: I. Mortality results.
short atrioventricular delay in congestive heart failure: a randomized study. J Am
Coll Cardiol 1995;26:967–973.
40. Gundersen T. Influence of heart size on mortality and reinfarction in patients
65. Shinbane JS, Chu E, DeMarco T, Sobol Y, Fitzpatrick AP, Lau DM, Klinski
treated with timolol after myocardial infarction. Br Heart J 1983;50:135–139.
C, Schiller NB, Griffin JC, Chatterjee K. Evaluation of acute dual-chamber
41. Gottlieb SS, McCarter RJ, Vogel RA. Effect of beta-blockade on mortality
pacing with a range of atrioventricular delays on cardiac performance in refrac-
among high-risk and low-risk patients after myocardial infarction. N Engl J Med
tory heart failure. J Am Coll Cardiol 1997;30:1295–1300.
1998;339:489 – 497.
Kerwin WF, Botvinick EH, O'Connell MS, Merrick SH, DeMarco T,
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM,
Chatterjee K, Saxon LA. Biventricular pacing in dilated cardiomyopathy: acute
Shusterman NH. The effect of carvedilol on morbidity and mortality in patients
improvements in biventricular ejection fraction correspond with measures of im-
with chronic heart failure. N Engl J Med 1996;334:1349 –1355.
43.
proved RV/LV synchrony. (Abstr.) PACE Pacing Clin Electrophysiol 1998;21:189.
Julian DG, Camm AJ, Frangin G, Janse MJ, Munoz A, A, Schwartz PJ,
Simon P. Randomised trial of effect of amiodarone on mortality in patients with
Blanc JJ, Etienne Y, Gilard M, Mansourati J, Munier S, Boschat J, Benditt
left-ventricular dysfunction after recent myocardial infarction: EMIAT. Lancet
DG, Lurie-KG. Evaluation of different ventricular pacing sites in patients with
severe heart failure: results of an acute hemodynamic study. Circulation 1997;
44. Cairns JA, Connolly SJ, Roberts R, Gent M. Randomised trial of outcome
after myocardial infarction in patients with frequent or repetitive ventricular
68. Cazeau S, Ritter P, Lazarus A, Gras D, Backdach H, Mundler O, Mugica J.
premature depolarisations: CAMIAT. Lancet 1997;349:675– 682.
Multisite pacing for end-stage heart failure: early experience. PACE Pacing Clin
45. Doval HC, Nul DR, Grancelli HO, Perrone SV, Bortman GR, Curiel R.
Electrophysiol 1996;19:1748 –1757.
Randomised trial of low-dose amiodarone in severe congestive heart failure.
69. Saxon LA, DeMarco T, Chatterjee K, Boehmer J, for the Vigor-CHF
Lancet 1994;344:493– 498.
Investigators. The magnitude of sympathoneural activation in advanced heart
46. Singh SN, Fletcher RD, Fisher SG, Singh BN Lewis HD, Deedwania PC,
failure is altered with chronic biventricular pacing. (Abstr.) PACE Pacing Clin
Massie BM, Colling C, Lazzeri D, for the Survival Trial of Antiarrhythmic
Therapy in Congestive Heart Failure. Amiodarone in patients with congestive heart
70. Daubert C, Linde C, Cazeau S, Sutton R, Kappenberger L, Bailleul C, on
failure and asymptomatic ventricular arrhythmia. N Engl J Med 1995;333:77– 82.
behalf of the MUSTIC study group. Protocol design of the MUSTIC (Multisite
47. Amiodarone Trials Meta-Analysis Investigators: Effect of prophylactic ami-
Stimulation in Cardiomyopathy) study. (Abstr.) Arch Mal Coeur Vaiss 1998;91:154.
odarone on mortality after acute myocardial infarction and in congestive heart
71. Lamp B, Hammel D, Kerber S, Deng M, Breithardt G, Block M. Multisite
failure: meta-analysis of individual data from 6500 patients in randomised trials.
pacing in severe heart failure— how many patients are eligible? (Abstr.) PACE
Pacing Clin Electrophysiol 1998;21:736.
150D THE AMERICAN JOURNAL OF CARDIOLOGYT
Source: http://home.arcor-online.de/nordman/Publikationen/Potential%20benefit%20of%20BV%20pacing_AJC1999_83_143D-150D_Stellbrink.pdf
Treatment Options for Parkinson's Disease Medication is the primary treatment for symptoms of Parkinson's disease (PD). In a few cases, surgery may also be an option. It is very important for you, your family and/or caregivers to develop a solid understanding of the treatment options that may be available. Focusing on exercise, stress management, proper nutrition and other available complimentary
Catania - anno XXXII - n. 28 - 24 luglio 2016 - Euro 0,60 - www.prospettiveonline.it "Poste Italiane s.p.a." - Spedizione in abbonamento postale - D.L. 353/2003 (conv. in L. 27/02/ 2004 no 46) art. 1, c. 1, DCB - Fil. di CT - Taxe perçue - Tassa riscossa - ISSN: 1720-0881 settimanale regionale di attualità "In caso di mancato recapito rinviare al CMP/CPO di Catania, per la restituzione al mittente previo addebito. Il mittente si impegna a pagare la tariffa vigente"