Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Neurospinegp.com.mx
OPEN ACCESS
James I. Ausman, MD, PhD
For entire Editorial Board visit :
University of California, Los
Review Article
Microvascular decompression for glossopharyngeal neuralgia
through a microasterional approach: A case series
Rogelio Revuelta‑Gutiérrez, Andres Humberto Morales‑Martínez, Carolina Mejías‑Soto1,
Jaime Jesús Martínez‑Anda, Luis Alberto Ortega‑Porcayo
Departments of Neurosurgery and 1Neuroradiology, National Institute of Neurology and Neurosurgery "Manuel Velasco Suárez", Mexico City, Mexico
E‑mail: Rogelio Revuelta‑Gutiérrez ‑
[email protected]; *Andres Humberto Morales‑Martínez ‑
[email protected];
Carolina Mejías‑Soto ‑
[email protected]; Jaime Jesús Martínez‑Anda ‑
[email protected]; Luis Alberto Ortega‑Porcayo ‑
[email protected]
*Corresponding author
Received: 17 January 16 Accepted: 07 March 16 Published: 05 May 16
Abstract
Background: Glossopharyngeal neuralgia (GPN) is an uncommon craniofacial pain
syndrome. It is characterized by a sudden onset lancinating pain usually localized
in the sensory distribution of the IX cranial nerve associated with excessive vagal
outflow, which leads to bradycardia, hypotension, syncope, or cardiac arrest.
This study aims to review our surgical experience performing microvascular
decompression (MVD) in patients with GPN.
Methods: Over the last 20 years, 14 consecutive cases were diagnosed with GPN.
MVD using a microasterional approach was performed in all patients. Demographic
data, clinical presentation, surgical findings, clinical outcome, complications, and
long‑term follow‑up were reviewed.
Results: The median age of onset was 58.7 years. The mean time from onset
of symptoms to treatment was 8.8 years. Glossopharyngeal and vagus nerve
compression was from the posterior inferior cerebellar artery in eleven cases
(78.5%), vertebral artery in two cases (14.2%), and choroid plexus in one case
Video Available on:
(7.1%). Postoperative mean follow‑up was 26 months (3–180 months). Pain
analysis demonstrated long‑term pain improvement of 114 ± 27.1 months and pain
Access this article online
remission in 13 patients (92.9%) (
P = 0.0001) two complications were documented,
one patient had a cerebrospinal fluid leak, and another had bacterial meningitis.
There was no surgical mortality.
Conclusions: GPN is a rare entity, and secondary causes should be discarded.
Quick Response Code:
MVD through a retractorless microasterional approach is a safe and effective
technique. Our series demonstrated an excellent clinical outcome with pain
remission in 92.9%.
Key Words: Glossopharyngeal nerve, microvascular decompression, neuralgia,
neurovascular compression, vagus nerve
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
For reprints contact: [email protected]
How to cite this article: Revuelta-Gutiérrez R, Morales-Martínez AH, Mejías-Soto C, Martínez-Anda JJ, Ortega.Porcayo LA. Microvascular decompression for
glossopharyngeal neuralgia through a microasterional approach: A case series. Surg Neurol Int 2016;7:51.
http://surgicalneurologyint.com/Microvascular-decompression-for-glossopharyngeal-neuralgia-through-a-microasterional-approach:-A-case-series/
2016 Surgical Neurology International Published by Wolters Kluwer - Medknow
Surgical Neurology International 2016, 7:51 http://www.surgicalneurologyint.com/content/7/1/51
management; (3) pain not controlled with medication.
All patients were previously managed with conservative
Glossopharyngeal neuralgia (GPN) is an uncommon treatment including carbamazepine, gabapentin, and
craniofacial pain syndrome, representing 0.2–1.3%[3,8]
pregabalin. No pain improvement for at least 6 months
of facial pain syndromes, with an annual incidence of
before surgical procedure was documented. Diagnosis
0.7 cases per 100,000 habitants per year according to work‑up included a 3T magnetic resonance imaging
a population‑based study.[14] It is characterized by a (MRI). T1, T2, gadolinium‑enhanced and FIESTA
sudden onset of lancinating acute pain, lasting seconds
sequences were assessed to discard a secondary cause of
to minutes, usually in the sensory distribution of the
the symptoms and identify vascular compression.
auricular and pharyngeal branches of the of the IX and
X cranial nerve. The pain is felt in the pharynx, tongue,
A statistical analysis was performed using SPSS Version
tonsillar fossa, internal ear, and mandible angle. In some
20 (IBM SPSS Statistics, New York, USA). Categorical
cases, it is associated with excessive vagal outflow; which
variables were expressed as proportions and continuous
leads to bradycardia, hypotension, syncope,
variables were expressed using means and standard
deviations. Clinical outcome was evaluated according
to the surgical management, use of medications, pain
The first GPN description is attributed to recurrence, and postoperative complications. Descriptive
Theodore H. Weisenburg in 1910.[24] Dandy elucidated
statistics was performed for the patient data and the
the pathophysiology of trigeminal neuralgia and proposed
grade of pain preoperatively and postoperatively was
vascular compression as the main etiology, causing analyzed using Wilcoxon signed‑rank test. P < 0.05 was
demyelization, and ephaptic transmission;[4,24] which is considered statistically significant.
the same pathophysiology of GPN. First line medical
treatment, including carbamazepine and gabapentin, may
sometimes improve pain paroxysms.[28] However, in cases
Under general anesthesia patients were placed in park
with refractory GPN various surgical approaches have been
bench position with the head fixed in a Mayfield skull
attempted. In 1920, Sicard and Robineau[31] proposed clamp. The upper shoulder was retracted, and the head
sectioning the glossopharyngeal nerve through the neck
was rotated 60° to the opposite side of the exposure
as a definitive treatment; which evolved to intracranial
with slight cervical lateral tilting (10°) toward the floor.
rhizotomy of the glossopharyngeal nerve performed by
A 5 cm retrosigmoid incision centered over the asterion
Dandy.[8] Later on, Sweet,[35] introduced percutaneous was performed and a keyhole (2.5–3 cm) asterional
compression at the middle fossa and finally Jannetta, craniectomy exposed the angle of the transverse and
popularized microvascular decompression (MVD) as a sigmoid sinuses [Figures 1 and 2a]. Curvilinear durotomy
definitive surgical treatment for this pathology.[12,17,32]
was performed under microscope magnification and
MVD series have reported good outcomes in 90–98%,
intradural dissection started toward the dural angle
long‑term pain improvement have been observed in 64%
between the tentorium and petrous surface [Figure
with a low mortality ranging from 0% to 5.8%.[13]
2b]. Cerebrospinal fluid (CSF) was released through
arachnoid dissection without using cerebellar retractors.
This study aims to review our surgical experience The dissection was directed caudally, and the lower
performing MVD using a microasterional approach in vascular nervous complex involving the glossopharyngeal
patients with GPN.
This study is a consecutive case series of 14 patients, who
underwent MVD for the treatment of idiopathic GPN
at the National Institute of Neurology and Neurosurgery
"Manuel Velasco Suárez", in Mexico City, between 1994
and 2014. The senior author (Rogelio Revuelta‑Gutiérrez)
performed all the surgeries. A retrospective analysis of
the clinical charts was performed. Patient data including
gender, the age of onset, symptoms, previous medical
management, operative findings, complications, and
clinical outcome were collected. Pain intensity was
graded according a three‑grade scale: (1) No pain, no
need for medication; (2) pain controlled with medical
Figure 1: Craniotomy size and reference
Surgical Neurology International 2016, 7:51 http://www.surgicalneurologyint.com/content/7/1/51
nerve was exposed, identifying its exit through the jugular
The pain was more common on the left side (78.6%)
foramen. Once the identification of the vascular element
compared to the right (21.4%). The primary location
compressing the glossopharyngeal nerve was observed of the pain was pharyngeal in 13 cases (92.9%) and
[Figure 2c], blunt dissection was done, and a small preauricular in one case (7.1%). Pain irradiation
piece or multiple pieces of Teflon were placed between
was referred in 6 cases (42.9%), 5 of them to the
the glossopharyngeal nerve and the compressing vessels
preauricular area and one to the pharynx. One patient
(arterial or venous) [Figure 2d, Video 1].
(7.1%) presented with syncope and another one had an
intraoperative vasovagal reflex during decompression.
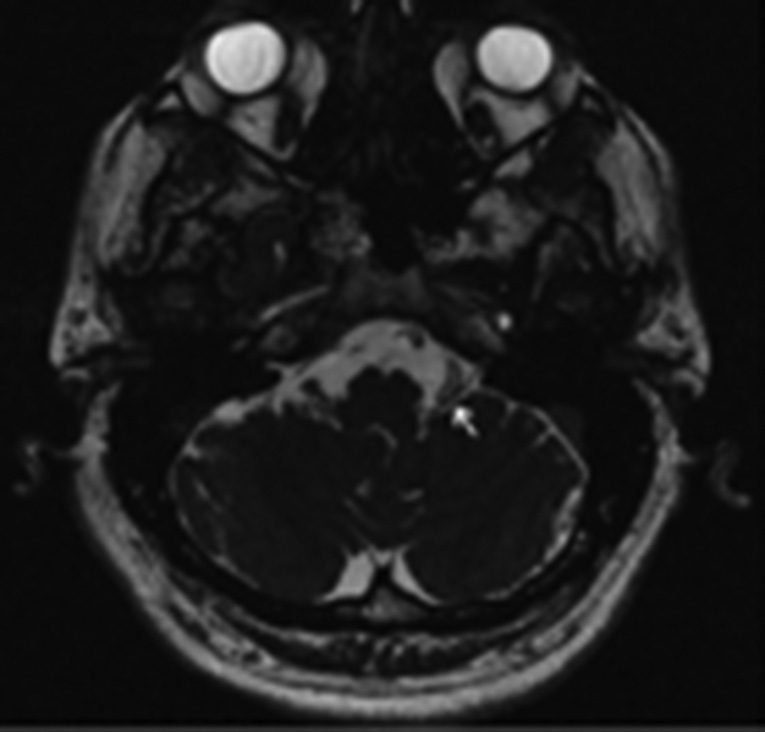
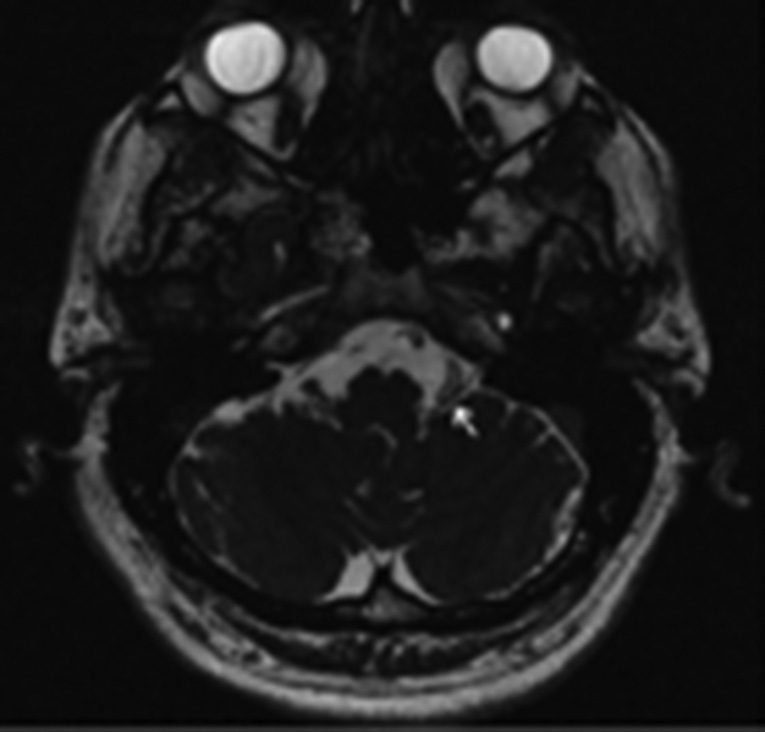
Neuroradiological and operative findings
MRI showed vascular compression from the posterior
inferior cerebellar artery (PICA) [Figure 3] in three
A total of 14 patients were diagnosed with GPN and were
patients (21.4%), vertebral‑basilar arteries in three
surgically treated [Table 1]. The median age of onset was
patients (21.4%), and an inflammatory process in one
58.7 ± 11 years, with a male to female ratio of (1:1.8).
The mean time duration from symptom onset to surgery
patient (7.1%). Seven patients were reported as normal
was 8.8 years. Pain trigger was described when swallowing
on MRI scan (49.7%). At the time of the surgery, all 14
in seven cases, talking in four cases and without previous
patients were found to have compression of the vagal and
stimuli in three cases. Carbamazepine was the most used
glossopharyngeal nerve roots. Vascular compression was
medication (78%), followed by gabapentin and pregabalin;
from PICA in 11 cases (78.5%), vertebral artery in two
64.2% patients were on more than one drug. All patients
cases (14.2%), and compression from the choroid plexus
from this study had no clinical improvement with full in one case (7.1%).
dose carbamazepine, gabapentin, pregabalin, and daily
Clinical outcome
analgesic medication. Three patients were misdiagnosed
All 14 patients were contacted for long‑term follow‑up.
before they were referred to our institution; stiloidectomy
Postoperative mean follow‑up of was 26 months
was performed in two patients (14.3%) and previous dental
(3–180 months). All patients referred initial pain relief,
surgery in one patient (7.1%). Mean time from diagnosis
and 13 were pain‑free with no need of medication in
to surgery was 106.3 ± 95.7 months (males 86.4 ± 78.4
the long‑term follow‑up. Only one patient referred pain
months and females 117.3 ± 106.9 months; P = 0.58).
1 month after surgery and was treated with carbamazepine
with complete relief of the pain and no further surgery
Table 1: Clinical data and outcome of patients with
was required. Pain analysis demonstrated long‑term pain
improvement of 114 ± 27.1 months and pain remission
in 13 patients (92.9%) (P = 0.0001) [Table 1].
Pain localization
Two patients presented complications related to surgical
treatment. One patient presented with CSF leak, which
resolved with lumbar drainage and acetazolamide 500 mg
TID for 5 days without any complications. The second
patient presented with meningitis and was treated with
intravenous vancomycin 1 g. BID for 5 days recovering
completely without clinical sequelae [Table 1]. There was
no surgical mortality in this case series.
Wilfred Harris applied the term GPN when he described
an entity similar to trigeminal neuralgia. At his initial
Preoperative pain
report in 1937, Harris described two types of pathologies:
Primary or idiopathic and secondary to carcinoma.
Long‑term follow‑up postoperative pain
Idiopathic GPN is explained due to nerve compression by
a vessel, as it exits the medulla oblongata.[24] This theory
is supported by the success of MVD in the treatment
of this pathology.[32] The main symptom of the GPN is
a lancinating pain lasting seconds to minutes. However,
Cerebrospinal fluid leak
some cases have reported the presence of pain associated
to syncope.[7] In this regard, Gardner associated the
Surgical Neurology International 2016, 7:51 http://www.surgicalneurologyint.com/content/7/1/51
Figure 2: Glossopharyngeal microvascular decompression through
Figure 3: Preoperative axial magnetic resonance FIESTA image
a minimal invasive asterional approach. (a) Right microasterional
demonstrates glossopharyngeal nerve compression from the left
approach (2.5–3 cm). (b) Durotomy exposing right cerebellar
hemisphere, the base of the dural opening is reflected at the
junction of the sigmoid and transverse sinus. (c) Cerebrospinal
can be performed. For lower cranial nerve exposure;
fluid drainage after arachnoid dissection allows proper visualization
of the vertebral artery compressing the glossopharyngeal nerve.
McLaughlin et al.,[20] recommended a triangular
(d) A piece of Teflon is interposed between the affected nerve and
craniectomy with the apex at the edge of the jugular
the offending vessel
bulb. In our experience, our circular microasterional
craniectomy [Figure 2a] at the edge of the transverse and
proximity of the glossopharyngeal nucleus to the sigmoid sinuses gives enough bone exposure to access the
vagal nucleus. The activation of the nucleus produces
trigeminal, facial, and glossopharyngeal nerves.
activation of the vagal nerve, which results in bradycardia
and hypotension secondary to a decrease of the peripheral
In the MVD series, the overall surgical mortality is 1.1%.
vascular resistance. Another theory explains the vascular
The rate of long‑term pain remission is 84.7% with
resistance impairment secondary to inhibition of recurrence in 7%. Transient X cranial nerve dysfunction
vasomotor centers.[16]
occurred in 13.2% and permanent deficits in 5.5%.[27] In
our case series, we did not have any mortality, and no
Traditionally, a lateral suboccipital approach provides permanent deficits occurred after the surgery. We did
adequate exposure to the trigeminal, facial, and not have cerebellar lesions or hearing the loss in this case
lower cranial nerves. Kawashima et al.[15] proposed series; it is explained because we do not use retractors
a transcondylar fossa approach advocating the wide over the cerebellum, the surgical route place minimal
operative view of the cerebellomedullary cistern, smaller
traction on the VII–VIII nerve complex and we perform
retraction of the cerebellum, less risk of cranial nerve
a careful microsurgical vascular dissection with minimal
injury, and enough space to perform the sling retraction
bipolar coagulation. However, we had two complications;
technique. However, we believed that a minimally a CSF leak and a case of meningitis that was successfully
invasive technique as an asterional approach described
previously by the senior author[25] is enough for adequate
exposure of PICA, vertebral artery, and the relationship
Rey‑Dios and Cohen‑Gadol demonstrated in his analyses
with the glossopharyngeal nerve and the upper roots of
that the most effective surgical procedure to treat GPN
the vagus nerve. There is no need of retractors, and after
is the MVD.[27] Several studies used rhizotomy[2,9,13,17,29,36]
the CSF is released with adequate and careful arachnoid
as the preferred procedure, but a 3‑fold increase in the
dissection, the cerebellum is out of the way, and there
risk of permanent postoperative vagus dysfunction[27]
is enough space for working without the necessity of is objectionable in comparison to MVD. It is also well
removing the jugular tubercle.
demonstrated that the rate of pain control is slightly
better with rhizotomy (95%) than with MVD (86%).[27]
Jannetta,[12] popularized the MVD using a suboccipital
However, in our series we had 92.9% pain remission with
craniotomy. After years of experience, the approach 3–180 months (mean 26 months) of follow‑up; only
was modified according to the surgical goal. Initially, it
one case had pain recurrence that was treated with
is important to focus bone exposure to the junction of
carbamazepine. GPN is a rare condition in which the
the transverse and sigmoid sinuses. A smaller tailored clinical findings are not always typical. The mean duration
craniectomy according to the cranial nerve approach from symptom onset to surgery is 5–8 years.[13,23,30] In our
Surgical Neurology International 2016, 7:51 http://www.surgicalneurologyint.com/content/7/1/51
case series, we had a mean time for diagnosis of 8.8 years,
Conflicts of interest
however, despite the time for diagnosing GPN the clinical
There are no conflicts of interest.
outcome of our patients is similar to the reported in the
It is important to rule out secondary causes such 1. Arbit E, Krol G. Percutaneous radiofrequency neurolysis guided by computed
as neoplasm,[11] infections,[39] trauma,[39,40] vascular
tomography for the treatment of glossopharyngeal neuralgia. Neurosurgery
malformations,[10] Chiari malformation,[41] choroid plexus
overgrowth,[22] Tornwaldt's cyst,[33] Eagle syndrome,[6]
Ceylan S, Karakus A, Duru S, Baykal S, Koca O. Glossopharyngeal neuralgia:
pontine lesions,[19] multiple sclerosis,[21] and previous
A study of 6 cases. Neurosurg Rev 1997;20:196-200.
surgical interventions (vagal nerve stimulator).[5] It is 3. Chawla JC, Falconer MA. Glossopharyngeal and vagal neuralgia. Br Med J
essential to have a careful selection and an accurate 4. Dandy W. Glossopharyngeal neuralgia (tic doloreaux). Its diagnosis and
diagnosis of idiopathic GPN to avoid negative exploratory
treatment. Arch Surg 1927;15:198-214.
operations. Two of our patients were previously diagnosed
5. Duhaime AC, Melamed S, Clancy RR. Tonsillar pain mimicking
as Eagle syndrome, in both of them stiloidectomy was
glossopharyngeal neuralgia as a complication of vagus nerve stimulation:
performed without pain improvement, and one of them
Case report. Epilepsia 2000;41:903-5.
Eagle WW. Symptomatic elongated styloid process; report of two cases of
had a tooth extraction before referral to our Institution.
styloid process-carotid artery syndrome with operation. Arch Otolaryngol
During the diagnosis workup, we ruled out secondary
causes and confirmed an idiopathic GPN in all patients
Esaki T, Osada H, Nakao Y, Yamamoto T, Maeda M, Miyazaki T, et al. Surgical
and MVD was performed.
management for glossopharyngeal neuralgia associated with cardiac syncope: Two case reports. Br J Neurosurg 2007;21:599-602.
As Lister et al.[18] previously described in a microsurgical
8. Fraioli B, Esposito V, Ferrante L, Trubiani L, Lunardi P. Microsurgical
anatomic study, PICA has the most variable course of
treatment of glossopharyngeal neuralgia: Case reports. Neurosurgery 1989;25:630-2.
the cerebellar arteries, but most of the time it passes
9. Fraioli B, Esposito V, Guidetti B, Cruccu G, Manfredi M. Treatment of
under the glossopharyngeal nerve. In most of the recent
trigeminal neuralgia by thermocoagulation, glycerolization, and percutaneous
clinical series[13,15,30] PICA is the most common vessel
compression of the gasserian ganglion and/or retrogasserian rootlets:
compressing the glossopharyngeal nerve. In our series,
Long-term results and therapeutic protocol. Neurosurgery 1989;24:239-45.
10. Galetta SL, Raps EC, Hurst RW, Flamm ES. Glossopharyngeal neuralgia
during dissection we found PICA compression in eleven
from a posterior fossa arteriovenous malformation: Resolution following
cases (78.1%), in all of them we did the transposition of
embolization. Neurology 1993;43:1854-5.
the vessel and apply Teflon in between the nerve and the
11. Greene KA, Karahalios DG, Spetzler RF. Glossopharyngeal neuralgia
associated with vascular compression and choroid plexus papilloma. Br J Neurosurg 1995;9:809-14.
In refractory cases to MVD, we believe that sectioning
12. Jannetta PJ. Observations on the etiology of trigeminal neuralgia, hemifacial
the glossopharyngeal nerve and the upper roots of
spasm, acoustic nerve dysfunction and glossopharyngeal neuralgia. Definitive
vagus nerve involved an unaccepted high morbidity. We
microsurgical treatment and results in 117 patients. Neurochirurgia (Stuttg) 1977;20:145-54.
advocate for compression of the glossopharyngeal and 13. Kandan SR, Khan S, Jeyaretna DS, Lhatoo S, Patel NK, Coakham HB.
upper roots of the vagus nerve as a last option for pain
Neuralgia of the glossopharyngeal and vagal nerves: Long-term outcome
recurrence as previously demonstrated for trigeminal
following surgical treatment and literature review. Br J Neurosurg
neuralgia.[26] Other noninvasive treatment options have
14. Katusic S, Williams DB, Beard CM, Bergstralh EJ, Kurland LT. Epidemiology
been described: Percutaneous radiofrequency neurolysis[1]
and clinical features of idiopathic trigeminal neuralgia and glossopharyngeal
is an alternative in cases who failed medical treatment
neuralgia: Similarities and differences, Rochester, Minnesota, 1945-1984.
or in which they cannot undergo intracranial surgery.
Gamma Knife radiosurgery is also a potential option to
15. Kawashima M, Matsushima T, Inoue T, Mineta T, Masuoka J,
relieve the pain without reported side effects but a high
Hirakawa N. Microvascular decompression for glossopharyngeal neuralgia through the transcondylar fossa (supracondylar transjugular tubercle)
early recurrence risk.[34,42]
approach. Neurosurgery 2010;66:275-80.
16. Korkes H, de Oliveira EM, Brollo L, Hachul DT, Andrade JC, Peres MF,
et al. Cardiac syncope induced by glossopharyngeal "neuralgia": A rare presentation. Arq Bras Cardiol 2006;87:e189-91.
17. Laha RK, Jannetta PJ. Glossopharyngeal neuralgia. J Neurosurg 1977;47:316-20.
Glossopharyngeal MVD through a retractorless 18. Lister JR, Rhoton AL Jr., Matsushima T, Peace DA. Microsurgical anatomy
microasterional approach is a safe technique in which
of the posterior inferior cerebellar artery. Neurosurgery 1982;10:170-99.
surgical anatomical knowledge is essential to obtain good
19. McCarron MO, Bone I. Glossopharyngeal neuralgia referred from a pontine
results with minimal morbidity. Our series demonstrate
lesion. Cephalalgia 1999;19:115-7.
an excellent clinical outcome (pain remission ‑ 92.9%)
20. McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK.
Microvascular decompression of cranial nerves: Lessons learned after 4400
following MVD for GPN.
operations. J Neurosurg 1999;90:1-8.
Financial support and sponsorship
21. Minagar A, Sheremata WA. Glossopharyngeal neuralgia and MS. Neurology
22. Occhiogrosso M, De Tommasi A, Vailati G. Choroid plexus compression
Surgical Neurology International 2016, 7:51 http://www.surgicalneurologyint.com/content/7/1/51
of glossopharyngeal nerve in patients with glossopharyngeal neuralgia. J
33. Stern LZ, Hall SW. Tornwaldt's disease. Onset as symptomatic (secondary)
Neurosurg Sci 1996;40:37-41.
glossopharyngeal neuralgia. Neurology 1972;22:1182-5.
23. Patel A, Kassam A, Horowitz M, Chang YF. Microvascular decompression
34. Stieber VW, Bourland JD, Ellis TL. Glossopharyngeal neuralgia treated with
in the management of glossopharyngeal neuralgia: Analysis of 217 cases.
gamma knife surgery: Treatment outcome and failure analysis. Case report. J
Neurosurg 2005;102 Suppl:155-7.
24. Pearce JM. Glossopharyngeal neuralgia. Eur Neurol 2006;55:49-52.
35. Sweet WH. Percutaneous methods for the treatment of trigeminal neuralgia
25. Revuelta-Gutierrez R, Beltrán-Rochín J, Escobedo-Ríos F, Flores-Orozco J.
and other faciocephalic pain; comparison with microvascular decompression.
Microcraniectomía asterional: Una opción quirúrgica para la patología del
Semin Neurol 1988;8:272-9.
ángulo ponto-cerebeloso. Rev Ecuat Neurol1999;8:6-10.
36. Taha JM, Tew JM Jr. Long-term results of surgical treatment of idiopathic
26. Revuelta-Gutierrez R, Martinez-Anda JJ, Coll JB, Campos-Romo A,
neuralgias of the glossopharyngeal and vagal nerves. Neurosurgery
Perez‑Peña N. Efficacy and safety of root compression of trigeminal nerve
for trigeminal neuralgia without evidence of vascular compression. World
37. Teixeira MJ, de Siqueira SR, Bor-Seng-Shu E. Glossopharyngeal neuralgia:
Neurosurgical treatment and differential diagnosis. Acta Neurochir (Wien)
27. Rey-Dios R, Cohen-Gadol AA. Current neurosurgical management
of glossopharyngeal neuralgia and technical nuances for microvascular
decompression surgery. Neurosurg Focus 2013;34:E8.
38. Thomson JL. Glossopharyngeal neuralgia accompanied by unconsciousness.
28. Rozen TD. Trigeminal neuralgia and glossopharyngeal neuralgia. Neurol Clin
J Neurosurg 1954;11:511-4.
39. Waga S, Kojima T. Glossopharyngeal neuralgia of traumatic origin. Surg
29. Rushton JG, Stevens JC, Miller RH. Glossopharyngeal (vagoglossopharyngeal)
neuralgia: A study of 217 cases. Arch Neurol 1981;38:201-5.
40. Webb CJ, Makura ZG, McCormick MS. Glossopharyngeal neuralgia following
30. Sampson JH, Grossi PM, Asaoka K, Fukushima T. Microvascular
foreign body impaction in the neck. J Laryngol Otol 2000;114:70-2.
decompression for glossopharyngeal neuralgia: Long-term effectiveness and
41. Yglesias A, Narbona J, Vanaclocha V, Artieda J. Chiari type I malformation,
complication avoidance. Neurosurgery 2004;54:884-9.
glossopharyngeal neuralgia and central sleep apnoea in a child. Dev Med
31. Sicard R, Robineau J. Algie vélo-pharyngée-es-sentielle. Traitement chirurgical.
Child Neurol 1996;38:1126-30.
Rev Neurol 1920;36:256-7.
42. Yomo S, Arkha Y, Donnet A, Régis J. Gamma knife surgery for
32. Slavin KV. Glossopharyngeal neuralgia. Semin Neurosurg 2004;15:71-9.
glossopharyngeal neuralgia. J Neurosurg 2009;110:559-63.
Source: http://neurospinegp.com.mx/wp-content/uploads/2016/07/Surg-Neurol-Int-2016-Revuelta-Gutierrez.pdf
Aspiration in Juvenile Squirrels: Etiologies, Treatments, Prevention Shirley CaSey1 and MaCkenzie Goldthwait, dVM2 1wildaGain wildlife rehabilitation inC., eVerGreen, Colorado 2annie'S aniMal hoSpital, hiGhlandS ranCh, Colorado Abstract: Respiratory problems are, unfortunately, rather common in What is Aspiration? juvenile squirrels in rehabilitation. Such problems often result from
INCREASING ACCESS TO THE REPRODUCTIVE INFORMATION AND SERVICES, SRHR EDUCATION FOR YOUTH AND LEGAL ABORTION (2009) Reproductive Rights Advocacy Alliance Malaysia (RRAAM); Federation of Reproductive Health Associations Malaysia (FRHAM). Edited by Rashidah Abdullah