Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Newgel.co.uk
Back to the Training Manual
International Clinical Recommendations onScar Management
Thomas A. Mustoe, M.D., Rodney D. Cooter, M.D., Michael H. Gold, M.D., F. D. Richard Hobbs,
F.R.C.G.P., Albert-Adrien Ramelet, M.D., Peter G. Shakespeare, M.D., Maurizio Stella, M.D.,
Luc Téot, M.D., Fiona M. Wood, M.D., and Ulrich E. Ziegler, M.D., for the International Advisory Panel
on Scar Management
Chicago, Ill., Nashville, Tenn., Adelaide, South Australia, and Perth, Western Australia, Australia, Birmingham and Salisbury, United Kingdom, Lau-sanne, Switzerland, Turin, Italy, Montpellier, France, and Wurzburg, Germany
Many techniques for management of hypertrophic
therapies showed early promise in small-scale
scars and keloids have been proven through extensive use,
trials, but these results have not been repeated
but few have been supported by prospective studies withadequate control groups. Several new therapies showed
in larger trials with long-term follow-up. Judg-
good results in small-scale trials, but these have not been
ment of efficacy has further been limited by
repeated in larger trials with long-term follow-up. This
the difficulty in quantifying change in scar ap-
article reports a qualitative overview of the available clin-
pearance, and by the natural tendency for scars
ical literature by an international panel of experts using
to improve over time. Thus, cutaneous scar
standard methods of appraisal. The article provides evi-dence-based recommendations on prevention and treat-
management has relied heavily on the experi-
ment of abnormal scarring and, where studies are insuf-
ence of practitioners rather than on the results
ficient, consensus on best practice. The recommendations
of large-scale randomized, controlled trials and
focus on the management of hypertrophic scars and ke-
loids, and are internationally applicable in a range of
This article reports a qualitative overview of
clinical situations. These recommendations support amove to a more evidence-based approach in scar man-
over 300 published references using standard
agement. This approach highlights a primary role for
methods of appraisal and, where studies are
silicone gel sheeting and intralesional corticosteroids in
insufficient, expert consensus on best practices
the management of a wide variety of abnormal scars. The
from an international group with extensive ex-
authors concluded that these are the only treatments for
perience and interest in the treatment of scar-
which sufficient evidence exists to make evidence-basedrecommendations. A number of other therapies that are
ring. Although focusing primarily on the man-
in common use have achieved acceptance by the authors
agement of hypertrophic scars and keloids, the
as standard practice. However, it is highly desirable that
recommendations are internationally applica-
many standard practices and new emerging therapies un-
ble in a range of clinical situations.
dergo large-scale studies with long-term follow-up beforebeing recommended conclusively as alternative therapiesfor scar management.
(
Plast. Reconstr. Surg. 110: 560,
An initial systematic MEDLINE and EMBASE
search (1996 through 2001) took place using the
The management of hypertrophic scars and
mesh terms "scar treatments," "surgery," "silicone
keloids is characterized by a wide variety of
gel sheeting," "intralesional corticosteroids," "ra-
techniques. Many have been proven through
diotherapy," "cryotherapy," "pressure therapy,"
extensive use over the past two decades, but
and "laser therapy." In addition, a search on scar
few have been supported by prospective studies
evaluation methods took place and all review
with adequate control groups, and in some
articles on the management of hypertrophic
cases even safety data are lacking. Many new
scars and keloids were accessed in these data-
From Northwestern University School of Medicine, Royal Adelaide Hospital and The Queen Elizabeth Hospital, Gold Skin Care Centre,
University of Birmingham, Laing Burn Research Laboratories, Salisbury District Hospital, Burn Centre, CTO, Burns Unit University HospitalLapeyronie, Chirurgische Universitatsklinik, Burns Unit, and Royal Perth Hospital and Princess Margaret Children's Hospitals. Received forpublication March 20, 2001; revised December 6, 2001.
Vol. 110, No. 2 / SCAR MANAGEMENT RECOMMENDATIONS
bases. A secondary hand search of citations in the
forms have been developed to help use this
accessed articles was also conducted.
The authors provided additional review arti-
cles, clinical studies, and recent unpublished
PREVENTION OR TREATMENT
data that revealed further useful cited refer-
It is much more efficient to prevent hyper-
ences in English and other languages. Those
trophic scars than to treat them. Prevention
references providing original data on the effi-
implies using a therapy with the aim of reduc-
cacy of scar management techniques were
ing the risk of a problem scar evolving. The
graded according to "hierarchy of evidence"
transition to a treatment regimen takes place
methods to reflect the reliability of data.1–3 The
when a true hypertrophic scar or keloid, and
drafts of the manuscript were reviewed by the
not an immature scar, is diagnosed. Conceptu-
chairman and panel during a series of telecon-
ally and practically, treatment and prevention
ferences and by e-mail.
regimens can be similar, and the following sec-tion presents the clinical data for both. Early
diagnosis of a problem scar can considerablyimpact the outcome. The consensus of the au-
Scar classification schemes need to be as clin-
thors is that the most successful treatment of a
ically relevant as possible, and the authors have
hypertrophic scar or keloid is achieved when
extended standard terminology for this article
the scar is immature but the overlying epithe-
lium is intact, although this is not as yet con-firmed in current literature.
A number of grading systems have been sug-
gested over recent years.4–7 The most widely
A comprehensive review of the clinical liter-
used system is the Vancouver Scar Scale,8–10
ature published over the past 30 years on scar
which provides an objective measurement of
treatments was undertaken and the evidence
burn scars and assists prognosis and manage-
was graded for quality. An evaluation is pre-
ment. Generic measurement tools and record
sented for each modality. The efficacy of twoscar management techniques, silicone gelsheeting and injected corticosteroids, has been
demonstrated in randomized, controlled trials.
Scar Classification
Comparison between treatment modalities
and between clinical studies is difficult, as de-
Mature scar—A light-colored, flat scar.
fining an adequate response to therapy re-
Immature scar—A red, sometimes itchy or painful, and
slightly elevated scar in the process of remodeling. Many
mains a relatively neglected area. A mild partial
of these will mature normally over time and become flat,
response, which may still leave a cosmetically
and assume a pigmentation that is similar to the
unacceptable scar, is accepted as a therapeutic
surrounding skin, although they can be paler or slightlydarker.
success in most studies. Scars never disappear
Linear hypertrophic (e.g., surgical/traumatic) scar—A red,
and in many cases only partial response is
raised, sometimes itchy scar confined to the border of the
original surgical incision. This usually occurs within weeksafter surgery. These scars may increase in size rapidly for
The variability in efficacy and recurrence
3–6 months and then, after a static phase, begin to
rates between studies is striking and makes sin-
regress. They generally mature to have an elevated, slightly
gle uncontrolled studies impossible to evalu-
rope-like appearance with increased width, which isvariable. The full maturation process may take up to 2
ate. There are some good reasons for this vari-
ability. First, differentiating hypertrophic scars
Widespread hypertrophic (e.g., burn) scar—A widespread
from keloids can be problematic. Second,
red, raised, sometimes itchy scar that remains within theborders of the burn injury.
there is a tremendous range between the scar
Minor keloid—A focally raised, itchy scar extending over
that becomes hypertrophic in the first few
normal tissue. This may develop up to 1 year after injury
months and then completely resolves with little
and does not regress on its own. Simple surgical excisionis often followed by recurrence. There may be a genetic
or no treatment and the more severe hypertro-
abnormality involved in keloid scarring. Typical sites
phic scar that becomes permanently disfigur-
include earlobes.
ing. Length of follow-up, heterogeneity of the
Major keloid—A large, raised (⬎0.5 cm) scar, possibly
painful or pruritic and extending over normal tissue. This
scars, and the lack of controls can either over-
often results from minor trauma and can continue to
estimate or understate the benefit of treat-
spread over years.
ment, but more often the former. Third, ke-
PLASTIC AND RECONSTRUCTIVE SURGERY,
August 2002
loids often do not recur for 6 months to as long
mg/ml), and up to 63 percent of patients ex-
as 2 years, and so length of follow-up is critical.
perience side effects that include skin atrophy,
Very few studies on keloids have adequate fol-
depigmentation, and telangiectasias.29 Topical
low-up. These limitations must be kept in mind
steroid creams have been used with varying
in evaluating any of the therapies below.
success,30 but absorption through an intact ep-ithelium into the deep dermis is limited. A
prospective, randomized study shows that top-
Surgical excision of hypertrophic scars or
ical steroids do not reduce scar formation in
keloids is a common management option
postburn deformities.31
when used in combination with steroidsand/or silicone gel sheeting. However, exci-
Silicone Gel Sheeting
sion alone of keloids results in a high rate of
Silicone gel sheeting has been a widely used
recurrence (45 to 100 percent).11–14
clinical management option for hypertrophic
Combining surgery with steroid injections
scars and keloids since the early 1980s.32–37 De-
reduces the recurrence rate of keloids to less
spite initial skepticism, there is now good evi-
than 50 percent, with the combination of sur-
dence of its efficacy and silicone gel sheeting
gery and perioperative radiation therapy re-
has now become standard care for plastic sur-
ducing recurrence to 10 percent.11,15 However,
geons. Results from at least eight randomized,
this combination approach is usually reserved
controlled trials and a meta-study of 27 trials38
for abnormal scars resistant to other
demonstrate that silicone gel sheeting is a safe
and effective management option for hypertro-
Hypertrophic scarring resulting from exces-
phic scars and keloids.39–48 Totally occlusive
sive tension or wound complications, such as
dressings (e.g., polyethylene films) and semi-
infection or delay in healing, can be treated
occlusive dressings, such as polyurethane films,
effectively with surgical excision combined
have not shown evidence of efficacy, and evi-
with surgical taping and silicone gel sheeting.
dence of the effectiveness of other materials
Scars that are subject to tension require sub-
such as glycerin and other non–silicone-based
stantial physical support. The authors agreed
dressing is mixed.49–51
that the most effective way of splinting scars is
Silicone gel sheeting may be especially useful
by surgical closure with intradermal sutures for
in children and others who cannot tolerate the
at least 6 weeks and, when tension is substan-
pain of other management procedures. Sili-
tial, for up to 6 months. Surgical techniques,
cone products vary considerably in composi-
such as W-plasty and Z-plasty, improve the ap-
tion, durability, and adhesion. To date, most
pearance and mobility of contracted burn scars
conclusive trials have been undertaken on
but are not appropriate for immature hyper-
pure adherent silicone gel sheeting. It is not
known whether these results are transferable toother fabric/polyurethane dressings with sili-
cone adhesive or to nonadherent silicone
Despite relatively few randomized, prospec-
products.52 Some formulations of silicone oil
tive studies, there is a broad consensus that
have been shown to be effective on minor hy-
injected triamcinolone is efficacious and is
pertrophic scars, although these studies have
first-line therapy for the treatment of keloids
limitations in their design.33,53
and second-line therapy for the treatment ofhypertrophic scars if other easier treatments
Pressure Therapy
have not been efficacious.15,17–23 Despite their
Pressure therapy has been used in the man-
use in scar management since the mid-1960s,
agement of hypertrophic scars and keloids
their principal mechanism of action remains
since the 1970s.54 It has been standard therapy
unclear.24,25 Response rates vary from 50 to 100
for hypertrophic burn scars and is still first-line
percent, with a recurrence rate of 9 to 50 per-
therapy in many centers.55–61
cent.18 Results are improved when corticoste-
It is generally recommended that pressure
roids are combined with other therapies such
be maintained between 24 and 30 mmHg for 6
as surgery11,13,26 and cryotherapy.27,28
to 12 months for this therapy to be effective;
Intralesional corticosteroid injection is asso-
however, this advice is largely empiric.18,62
ciated with significant injection pain, even with
There are mixed reports on long-term compli-
standard doses of insoluble triamcinolone (40
ance, but it remains a significant issue, as ef-
Vol. 110, No. 2 / SCAR MANAGEMENT RECOMMENDATIONS
fectiveness seems to be related directly to the
high-energy short-pulsed carbon dioxide lasers
duration of pressure.63–65
and scanned continuous-wave carbon dioxide
The evidence supporting the speed of scar
lasers were effective in postsurgical hypertro-
maturation and enhancement of cosmetic out-
phic/keloidal, traumatic, acne, and varicella
come is variable. For example, in a prospective
scars.75,76 Scanning carbon dioxide lasers have
randomized study in 122 burn patients, pres-
been used to debride burn wounds, but with-
sure garments did not increase the speed of
out clinically improved scar outcome.77 How-
wound maturation or decrease the duration of
ever, these early reports have not been widely
substantiated, and currently carbon dioxide la-ser is not widely accepted for the treatment of
keloids because of the high late recurrence
Radiotherapy has been used as mono-
therapy, and in combination with surgery, for
Argon lasers were first used in the 1970s for
hypertrophic scars and keloids. However,
the management of keloids, but studies failed
monotherapy remains controversial15,67 be-
to show long-term improvements.73,78 They pro-
cause of anecdotal reports of carcinogenesis
duce more nonspecific thermal damage than
following the procedure. Response to radio-
carbon dioxide lasers and are associated with
therapy alone is 10 to 94 percent, with a keloid
higher levels of keloid recurrence.76
recurrence rate of 50 to 100 percent.11,13 Such
More recent wavelength-specific lasers (yttri-
high recurrence rates are understandable,
um-aluminum-garnet and pulsed-dye lasers)
given the resistance of these cases to other
have been used to selectively ablate blood ves-
management options. Best results have been
sels. Neodymium:yttrium-aluminum-garnet la-
achieved with 1500 to 2000 rads over five to six
sers have response rates between 36 and 47
sessions in the early postoperative period.68,69
percent.79 In a recent study of 17 patients with
There have been mixed results from radiother-
keloids, nearly 60 percent of keloids were flat-
apy after surgical excision of keloids, with a
tened following one session of neodymium:
significant objective response reported in 25 to
yttrium-aluminum-garnet laser treatment.
100 percent of patients.18,70,71
These patients remained free of keloid scar-
Radiotherapy is difficult to evaluate, as most
ring at 18-month to 5-year follow-up.80 The re-
studies are retrospective, do not define the
maining seven patients required further laser
term "recurrence," and use a variety of radia-
treatment and intralesional corticosteroids to
tion techniques with varying follow-up (6 to 24
flatten the keloids completely. Recurrence of
months). In addition, there are no random-
keloids occurred in three patients, all of whom
ized, prospective studies with long-term follow-
responded to further laser treatment. A recent
up. Most investigators agree that radiotherapy
study in 36 patients has shown that the pulsed
should be reserved for adults and keloids resis-
erbium:yttrium-aluminum-garnet laser is an ef-
tant to other management modalities. Never-
fective and safe treatment option for hypertro-
theless, radiotherapy with informed consent
phic and depressed scars.81 Further large com-
remains a valuable therapeutic option and is
parative studies with longer follow-up are now
the most efficacious treatment available in se-
vere cases of keloids, provided there is appro-
Flashlamp-pumped pulsed-dye lasers have
priate shielding of nonaffected tissues.
shown promise in elimination of erythema andflattening atrophic and hypertrophic scars.82–85
Laser Therapy
Intense-pulsed-light-source devices are usually
Laser therapy has been used for nonspecific
considered in the same category as pulsed-dye
destruction of tissue to produce less scarring,
lasers. Improvements in appearance of hyper-
but this has been largely discredited following
trophic scars and keloids have been noted in
mixed results in larger long-term trials with
57 to 83 percent of cases,82 with further im-
carbon dioxide and argon lasers. Carbon diox-
provements seen in combination with intrale-
ide lasers showed early promise in the excision
sional corticosteroids.86 A pilot study has sug-
of keloids72 but failed to suppress keloid
gested that laser treatment in combination
growth and recurrence in later studies.73,74
with intralesional corticosteroids is effective in
Two newer types of carbon dioxide laser are
healing previously resistant keloids.87 A recent
in use. Small noncontrolled studies, limited by
study in 106 patients (171 anatomic sites) has
lack of long-term follow-up, suggested that
shown fast resolution of scar stiffness and ery-
PLASTIC AND RECONSTRUCTIVE SURGERY,
August 2002
thema and improvement in quality of scarring
ments that have an absence of randomized
when preventive treatment with flashlamp-
studies or some negative studies suggesting
pumped pulsed-dye lasers is started within 2
lack of efficacy. These include topical vitamin
weeks after surgery.88 However, a recent single-
E,31,97,98 onion extract cream,99 allantoin-
blind, randomized, controlled study in 20 pa-
sulfomucopolysaccharide gel,100,101 glycosami-
tients with hypertrophic scars showed no im-
noglycan gel,102 and creams containing extracts
provements in hypertrophic scars following
from plants such as
Bulbine frutescens and
Cen-
laser therapy.89 Laser therapy remains emerg-
ing technology, with limited follow-up and a
The second category includes classic thera-
lack of controlled studies. Further studies are
pies with anecdotal success but significant side
required to define its role. However, many der-
effects or lack of confirming studies. These
matologists, and some of the authors, have
include topical retinoic acid,104 colchicine,105
seen benefits in erythematous hypertrophic
and systemic antihistamines.106
scars in speeding resolution, and perhaps im-
The third category includes newer therapies
proving long-term outcomes.
with anecdotal reports that do not yet have ahistory. Although these may develop into use-
ful therapies in the future, the authors cannot
Cryotherapy alone results in keloid flatten-
make any recommendations at this time. These
ing in 51 to 74 percent of patients after two or
include skin equivalents that incorporate arti-
more sessions, and it is beneficial for the man-
ficial dermis constructs, cyclosporine,107 and
agement of severe acne scars.90–93 Limitations
include the delay of several weeks required for
Other physical management options include
postoperative healing and the commonly oc-
hydrotherapy, massage, ultrasound, static elec-
curring side effect of permanent hypopigmen-
tricity, and pulsed electrical stimulation. Hy-
tation. Other side effects include hyperpig-
drotherapy is widely used in several European
mentation, moderate skin atrophy, and pain.94
countries for the treatment of hypertrophic
As a result, cryotherapy is generally limited to
burn scars (using high pressure). Massage has
management of very small scars.
been widely used by physical therapists, occu-pational therapists, and other allied health
Adhesive Microporous Hypoallergenic Paper Tape
care professions. However, further long-term
The consensus of the authors was that apply-
studies are required before recommendations
ing paper tape with an appropriate adhesive to
can be made regarding their efficacy.
fresh surgical incisions, and for several weeksafter surgery, was useful. The mechanism of
Emerging Evidence
benefit is unknown, but may in part be me-chanical (analogous to pressure therapy) and
Three therapies provide emerging evidence
occlusive (analogous to silicone gel therapy).
However, only two uncontrolled studies con-firm its efficacy.95,96 The authors also felt that
• Interferon (interferon-␣, interferon-, and
this treatment was less effective than more es-
tablished treatments such as silicone gel, but it
• Intralesional 5-fluorouracil15,116
could be used as preventive treatment in low-
• Bleomycin injections117–120
risk patients, or before silicone gel use in freshincisions. Tape with an elastic component may
Interferon-␣, interferon-, and interferon-␥
be useful for scars over mobile or complex
have been shown to increase collagen break-
surfaces, including joints.
down.109–111 Tredget et al. found that interfer-on-␣2b injections three times weekly resulted
in significant mean rates of improvement of
There are anecdotal reports on a number of
hypertrophic scars versus control and also re-
additional therapies, but there is no adequate
duced serum transforming growth factor- lev-
published information on which the authors
els that continued after treatment.114 Inter-
can evaluate the efficacy and safety of these
feron injections are reported to be significantly
therapies or make recommendations. These
better than triamcinolone acetonide injections
therapies fall into three categories.
in preventing postsurgical recurrence of ke-
The first category includes popular treat-
loids (18.7 percent versus 58.5 percent recur-
Vol. 110, No. 2 / SCAR MANAGEMENT RECOMMENDATIONS
rence).115 However, these painful injections
and adding the transforming growth factor-3
may require regional anesthesia.
isoform. These approaches have shown efficacy
Intralesional 5-fluorouracil has been used
in animal models.125–127 Early human trials are
successfully as monotherapy as well as in com-
in progress for some of these strategies.
bination with intralesional corticosteroids to
Another area of active research is interfer-
treat hypertrophic scars and keloids.15,116 Phy-
ence with collagen synthesis. Historically, pen-
sicians experienced in its use show great enthu-
icillamine and other nonspecific inhibitors of
siasm for 5-fluorouracil. The rationale for its
collagen synthesis were used as inhibitors, but
use is sound, and it shows a lack of side effects.
they showed unacceptable toxicity. In recent
It may warrant further investigation and wider
years, several companies have looked for spe-
use as an alternative to steroid injections in
cific nontoxic inhibitors of collagen synthesis
that could be applied locally. Animal trials have
Bleomycin injections show evidence of effi-
been promising
.128 Overall, there has been a
cacy in managing surgical/traumatic hypertro-
substantial effort in the pharmaceutical and
phic scars.117,118 Patients with older scars resis-
biotechnology industry to develop more effec-
tant to intralesional corticosteroids showed
tive antiscarring therapies, and it seems likely
good response to bleomycin 0.01% injections
that new therapies will be available within the
every 3 to 4 weeks. A recent pilot study in 13
next 5 years.
patients showed complete flattening (six pa-tients) or significant flattening (⬎90 percent;
six patients) of hypertrophic scars and keloids
These recommendations are made primarily
following administration of bleomycin (1.5
on the basis of the clinical evidence reviewed
IU/ml) using a multiple-puncture method on
above and reflect the practice of the authors
the skin surface.119 Although published re-
and have been summarized in simple manage-
search is limited, there is considerable clinical
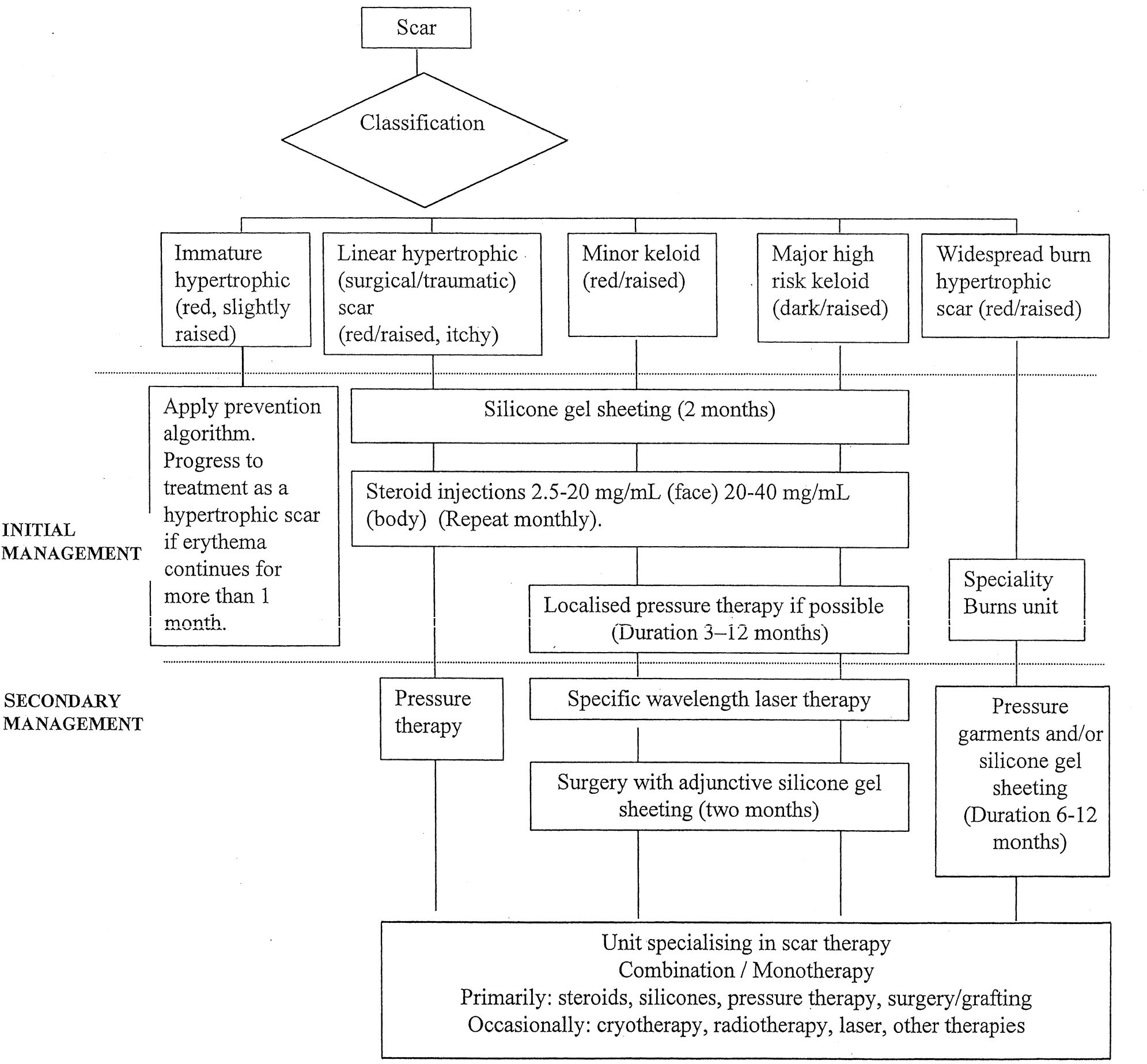
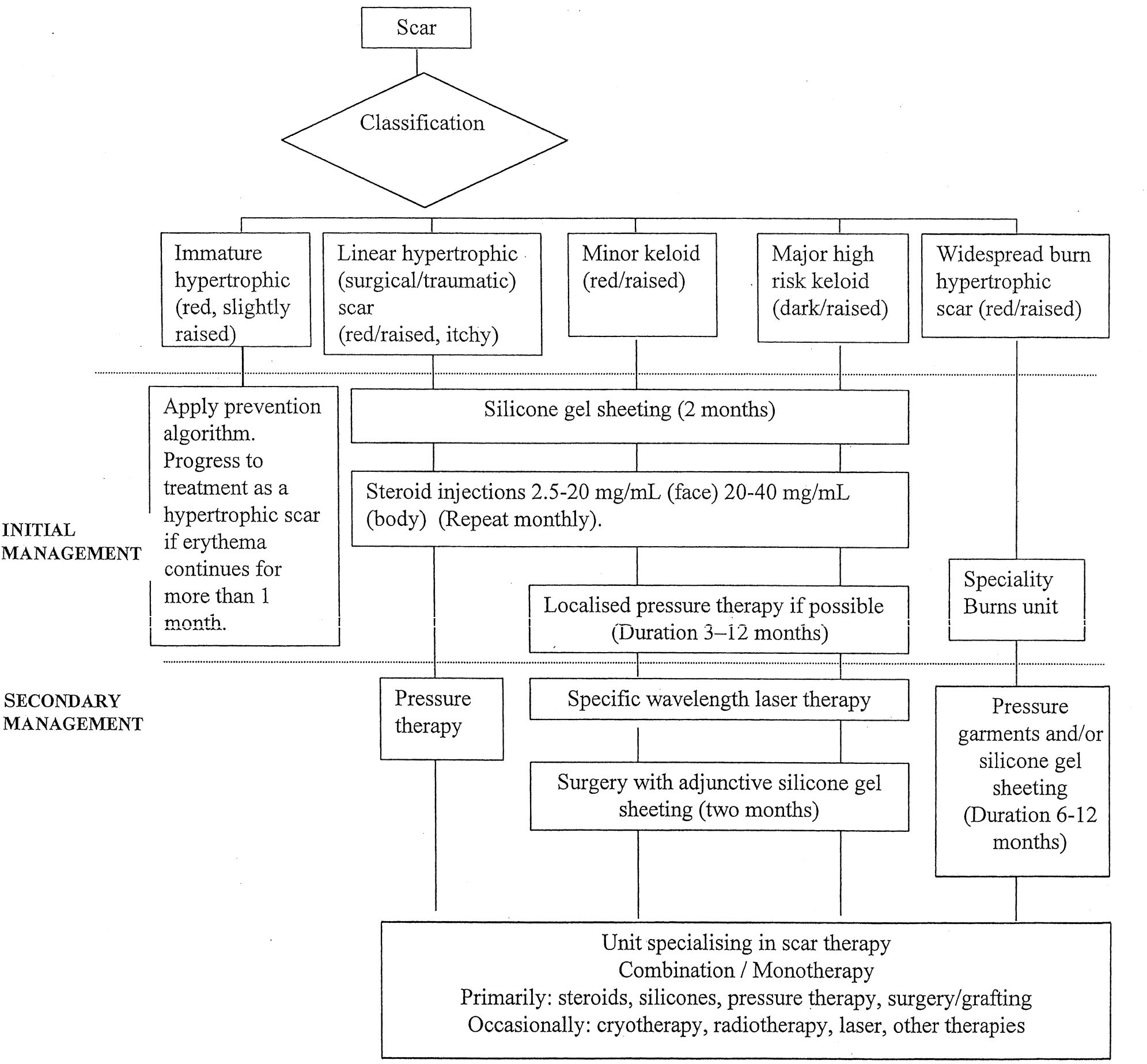
ment algorithms (Figs. 1 and 2). Cost-effective-
experience in using this modality in some Eu-
ness of therapies is not assessed in this article.
ropean countries. The rationale for use ofbleomycin, which is another chemotherapeutic
agent, is similar to that of 5-flourouracil. A
Every effort must be made to prevent the
comparative study of the two agents with ste-
development of hypertrophic scars or keloids
roids is warranted. Adverse effects have not
after surgery or trauma. Excellent surgical
been reported for this indication, although
technique and efforts to prevent postsurgical
side effects in the treatment of warts with bleo-
infection are of prime importance.129 Special
mycin include nail loss and Raynaud's
attention should be given to high-risk patients
(i.e., those who have previously suffered abnor-
Bleomycin and intralesional 5-fluorouracil
mal scarring or are undergoing a procedure
have been used by some of the authors with
with a high incidence of scarring, such as
considerable success. Despite a strong theoret-
breast and thoracic surgery). To our knowl-
ical rationale, larger scale prospective studies
edge, there has been no large-scale assessment
with appropriate follow-up are needed before
of scar outcomes and risk factors. Recom-
these treatments can be considered as standard
mended preventive techniques include the
In addition, experimental animal studies
suggest that there may be a role for transform-
• Hypoallergenic microporous tape with elas-
ing growth factor modulators.122–125 Transform-
tic properties to minimize the risk from
ing growth factor- has been implicated in sev-
shearing. Use of taping for a few weeks after
eral scarring conditions including pulmonary
surgery is standard practice for the majority
fibrosis, glomerulonephritis, and cutaneous
of the authors. Although there are no pro-
scarring. There are three isoforms, and there is
spective controlled studies documenting its
some evidence that the ratio is critical for op-
efficacy, the authors' consensus is that it is
timizing scar outcome. In addition to blocking
transforming growth factor- effects with anti-
• Silicone gel sheeting, which should be con-
bodies, researchers have proposed blocking
sidered as first-line prophylaxis. Use of sili-
transforming growth factor- activation by
cone gel sheeting should begin soon after
means of the mannose 6-phosphate receptor,
surgical closure, when the incision has fully
PLASTIC AND RECONSTRUCTIVE SURGERY,
August 2002
FIG. 1. Prevention of surgical/trauma scarring.
epithelialized, and be continued for at least
1 month. Silicone gel sheets should be worn
Pain and itchiness are commonly reported
for a minimum of 12 hours daily, and if
symptoms associated with scarring. Evidence of
possible for 24 hours per day, with twice-
management methodologies for pruritus re-
daily washing. Use of silicone ointments may
mains anecdotal. Pulsed-dye lasers may have
be appropriate on the face and neck re-
value in reduction of itching, although more
gions, although their efficacy in preventing
cost-effective options are preferred at this
scarring is unsupported by controlled trials.
stage. Other treatments, such as moisturizers,
Concurrent intralesional corticosteroid in-
silicone gel sheeting, systemic antihistamines,
jections as second-line prophylaxis for more
topical corticosteroids, antidepressants, mas-
severe cases.
sage, and hydrotherapy have been shown to
The effectiveness of alternative therapies is
improve symptoms. Care should be taken with
limited to anecdotal evidence. Patients at low
hypersensitivity to moisturizing products such
risk of scarring should maintain normal hy-
giene procedures and be provided with coun-seling and advice if concerned about their scar.
Immature hypertrophic scars (red).
Scar Classification and Patient History
difficult to predict whether this type of scar will
When patients present with a troublesome
resolve or develop into a hypertrophic scar. In
scar, appropriate therapy should be selected
the authors' experience, the techniques de-
on the basis of scar classification and patient
scribed above in the Prevention section should
history. Scar classification is the primary deci-
be followed. If erythema persists for more than
sion criterion for treatment selection. Patient
1 month, the risk of true hypertrophy increases
history, however, provides important informa-
and management should be as for a linear or
tion about the risk of the scar worsening
widespread hypertrophic scar as appropriate
should treatment fail, about previous thera-
(see below). These scars may benefit from a
pies, and about the patient's likely compliance.
course of pulsed-dye laser therapy, although
The degree of erythema has been identified as
this therapy requires further long-term trials.
being of great importance in predicting the
Linear hypertrophic (surgical/traumatic) scars
activity of the scar and response to therapy.
(red, raised).
Silicone gel sheeting should be
Vol. 110, No. 2 / SCAR MANAGEMENT RECOMMENDATIONS
FIG. 2. Complete management algorithm.
used as first-line therapy, in line with results
tonide, long-term placement of intradermal su-
from randomized, controlled trials. If the scar
tures, and subsequent corticosteroids. Specific-
is resistant to silicone therapy, or the scar is
wavelength laser therapy and cryotherapy have
more severe and pruritic, further management
been used by the authors but require further
with corticosteroid injections is indicated. Ad-
controlled studies.
ditional consideration may be given to other
Widespread burn hypertrophic scars (red/raised).
second-line therapies mentioned above for se-
Widespread burn scars should be treated with
first-line therapy of silicone gel sheeting and
If silicone gel sheeting, pressure garments,
pressure garments, although there remains lim-
and intralesional corticosteroid injections are
ited significant evidence for the efficacy of pres-
not successful after 12 months of conservative
sure garments. The treatment of burn scars is
therapy, surgical excision with postoperative
difficult and often requires a combination of
application of silicone gel sheeting should be
techniques including individualized pressure
considered. An option for more severe scars is
therapy; massage and/or physical therapy; sili-
reexcision with layering of triamcinolone ace-
cone gel sheeting; corticosteroids on particu-
PLASTIC AND RECONSTRUCTIVE SURGERY, August 2002
larly difficult areas; and surgical procedures
atic, quantitative reviews of the literature to
such as Z-plasty, excision, and grafting or flap
ensure optimal management of scarring. The
coverage. A variety of adjunctive therapies such
authors' recommendations are made on the
as massage, hydrocolloids, and antihistamines
basis of the best available evidence in the liter-
to relieve pruritus are also used. Pulsed-dye la-
ature, particularly randomized, controlled tri-
ser may have a role.
als, supported by clinical experience. Many
Minor keloids.
The consensus view from the
management techniques have limited data to
literature and the authors is that first-line ther-
support their use, and these recommendations
apy for most minor keloids is a combination of
support a move to a more evidence-based ap-
silicone gel sheeting and intralesional cortico-
proach in scar management.
steroids. If there is no resolution, surgical ex-
Thomas A. Mustoe, M.D.
cision with follow-up intralesional steroids and
Division of Plastic and Reconstructive Surgery
silicone gel sheeting is indicated. Localized
Northwestern University School of Medicine
pressure therapy such as ear clips on earlobe
675 North Saint Clair, 19-250
keloids has been shown to be helpful as second-
Chicago, Ill. 60611
line adjunctive therapy in small trials.
Surgical excision without careful follow-up
or use of other adjunctive measures will result
in a high recurrence rate, and if the surgery is
Editorial assistance has been provided by Jeremy Bray. A
performed without careful attention to pre-
small unrestricted educational grant was provided by Smith
serving normal architecture, the resulting de-
& Nephew Medical, Ltd., and used by the panel for coordi-
formity after recurrence may be worse. It is
nation and communication.
preferable to only partially excise the keloid
rather than produce a deformity. The authors'
1. Guyatt, G. H., Sackett, D. L., Sinclair, J. C., et al.
experience is that excision of difficult recur-
guides to the medical literature: IX. A method for
rent keloids with grafting of skin taken from
grading healthcare recommendations. J.A.M.A. 274:
the excised keloid followed by immediate radi-
ation therapy can be successful, but that the
2. Piantadosi, S.
David Byar as a teacher. Control. Clin.
Trials 16: 202, 1995.
long-term risks of radiation must be carefully
3. Olkin, I.
Statistical and theoretical considerations in
meta-analysis. J. Clin. Epidemiol. 48: 133, 1995.
Major keloids.
Major keloids are a most chal-
4. Davey, R. B., Sprod, R. T., and Neild, T. O.
lenging clinical problem, and many are resis-
erised colour: A technique for the assessment of burn
tant to any treatment. Extensive counseling with
scar hypertrophy. A preliminary report. Burns 25: 207,1999.
the patient is required before embarking on a
5. Powers, P. S., Sarkar, S., Goldgof, D. B., Cruse, C. W., and
surgical solution because the recurrence rate is
Scar assessment: Current problems and
so high. For some patients, symptomatic treat-
future solutions. J. Burn Care Rehabil. 20: 54, 1999.
ment with antihistamines and good hygiene
6. Beausang, E., Floyd, H., Dunn, K. W., Orton, C. I., and
may be all that is possible. Radiation therapy
Ferguson, M. W.
A new quantitative scale for clinical
scar assessment. Plast. Reconstr. Surg. 102: 1954, 1998.
should be considered for treatment failures,
7. Yeong, E. K., Mann, R., Engrav, L. H., et al.
and innovative therapies such as bleomycin and
burn scar assessment with use of a new scar-rating
5-flourouracil may have a future role, in addi-
scale. J. Burn Care Rehabil. 18: 353, 1997.
tion to investigational strategies that interfere
8. Sullivan, T., Smith, J., Kermode, J., et al.
with transforming growth factor- or collagen
burn scar. J. Burn Care Rehabil. 11: 256, 1990.
9. Baryza, M. J., and Baryza, G. A.
The Vancouver Scar
synthesis. These patients are best treated by cli-
Scale: An administration tool and its interrater reli-
nicians with a special interest in keloids. Ongo-
ability. J. Burn Care Rehabil. 16: 535, 1995.
ing patient counseling and advice on preven-
10. Nedelec, B., Shankowsky, A., and Tredgett, E. E.
tion are essential components of this therapy.
ing the resolving hypertrophic scar: Comparison ofthe Vancouver Scar Scale and scar volume. J. Burn CareRehabil. 21: 205, 2000.
11. Berman, B., and Bieley, H. C.
Adjunct therapies to
surgical management of keloids. Dermatol. Surg. 22:
Management choices should depend on the
patient's individual requirements and evi-
12. Darzi, M. A., Chowdri, N. A., Kaul, S. K., et al.
ation of various methods of treating keloids and hy-
dence-based findings. There remains a signifi-
pertrophic scars: A 10-year follow-up study. Br. J. Plast.
cant need for further randomized, controlled
Surg. 45: 374, 1992.
trials of all available scar therapies and system-
13. Lawrence, W. T.
In search of the optimal treatment of
Vol. 110, No. 2 / SCAR MANAGEMENT RECOMMENDATIONS
keloids: Report of a series and a review of the litera-
35. Carney, S. A., Cason, C. G., Gowar, J. P., et al.
ture. Ann. Plast. Surg. 27: 164, 1991.
gel sheeting in the management of hypertrophic scar-
14. Berman, B., and Bieley, H. C.
Keloids. J. Am. Acad.
ring. Burns 20: 163, 1994.
Dermatol. 33: 117, 1995.
36. Branagan, M., Chenery, D. H., and Nicholson, S.
15. Urioste, S. S., Arndt, K. A., and Dover, J. S.
of the infrared attenuated total reflectance spectros-
hypertrophic scars: Review and treatment strategies.
copy for the in vivo measurement of hydration level
Semin. Cutan. Med. Surg. 18: 159, 1999.
and silicone distribution in the stratum corneum fol-
16. Sherris, D. A., Larrabee, W. F., Jr., and Murakami, C. S.
lowing skin coverage by polymeric dressings. Skin Phar-
Management of scar contractures, hypertrophic scars
macol. Appl. Skin Physiol. 13: 157, 2000.
and keloids. Otolaryngol. Clin. North Am. 28: 1057, 1995.
37. Suetake, T., Sasai, S., Zhen, Y.-X., and Tagami, H.
17. Rockwell, W. B., Cohen, I. K., and Ehrlich, H. P.
fects of silicone gel sheet on the stratum corneum
loids and hypertrophic scars: A comprehensive review.
hydration. Br. J. Plast. Surg. 53: 503, 2000.
Plast. Reconstr. Surg. 84: 827, 1989.
38. Poston, J.
The use of silicone gel sheeting in the man-
18. Niessen, F. B., Spauwen, P. H. M., Schalkwijk, J., and
agement of hypertrophic and keloid scars. J. Wound
On the nature of hypertrophic scars and
Care 9: 10, 2000.
keloids: A review. Plast. Reconstr. Surg. 104: 1435, 1999.
39. Su, C. W., Alizadeh, K., Boddie, A., and Lee, R. C.
19. Alster, T. S., and West, T. B.
Treatment of scars: A
problem scar. Clin. Plast. Surg. 25: 451, 1998.
review. Ann. Plast. Surg. 39: 418, 1997.
40. Katz, B. E.
Silicone gel sheeting in scar therapy. Cutis
20. Murray, J. C.
Keloids and hypertrophic scars. Clin. Der-
56: 65, 1995.
matol. 12: 27, 1994.
41. Berman, B., and Flores, F.
Comparison of a silicone
21. Kelly, A. P.
Keloids. Dermatol. Clin. 6: 413, 1988.
gel-filled cushion and silicone gel sheeting for the
22. Murray, J. C.
Scars and keloids. Dermatol. Clin. 11: 697,
treatment of hypertrophic or keloid scars. Dermatol.
Surg. 25: 484, 1999.
23. Griffith, B. H., Monroe, C. W., and McKinney, P.
42. Gold, M. H.
A controlled clinical trial of topical sili-
follow-up study on the treatment of keloids with tri-
cone gel sheeting in the treatment of hypertrophic
amcinolone acetonide. Plast. Reconstr. Surg. 46: 145,
scars and keloids. J. Am. Acad. Dermatol. 30: 506, 1994.
43. Cruz-Korchin, N. I.
Effectiveness of silicone sheets in
24. McCoy, B. J., Diegelmann, R. F., and Cohen, I. K.
the prevention of hypertrophic breast scars. Ann.
vitro inhibition of cell growth, collagen synthesis and
Plast. Surg. 37: 345, 1996.
prolyl hydroxylase activity by triamcinolone ace-
44. Agarwal, U. S., Jain, D., Gulati, R., et al.
tonide. Proc. Soc. Exp. Biol. Med. 163: 216, 1980.
sheet dressings for prevention of post-minigraft cob-
25. Ketchum, L. D., Smith, J., Robinson, D. W., et al.
blestoning in vitiligo. Dermatol. Surg. 25: 102, 1999.
treatment of hypertrophic scar, keloid and scar con-
45. Ahn, S. T., Monafo, W. W., and Mustoe, T. A.
tracture by triamcinolone acetonide. Plast. Reconstr.
silicone gel for the prevention and treatment of hy-
Surg. 38: 209, 1966.
pertrophic scars. Arch. Surg. 126: 499, 1991.
26. Tang, Y. W.
Intra- and postoperative steroid injections
46. Ahn, S. T., Monafo, W. W., and Mustoe, T. A.
for keloids and hypertrophic scars. Br. J. Plast. Surg. 45:
silicone gel: A new treatment for hypertrophic scars.
Surgery 106: 781, 1989.
27. Hirshowitz, B., Lerner, D., and Moscona, A. R.
47. Gold, M. H.
The role of CICA-CARE in preventing
ment of keloid scars by combined cryosurgery and
scars following surgery: A review of hypertrophic and
intralesional corticosteroids. Aesthetic Plast. Surg. 6:
keloid scar treatments. Oral presentation at the An-
nual Meeting of the American Academy of Dermatol-
28. Whang, K. K., Park, H. J., and Myung, K. B.
ogy, San Francisco, Calif., March 10 –15, 2000.
analysis of the combination of cryosurgery and in-
48. Borgognoni, L., Martini, L., Chiarugi, C., Gelli, R., and
tralesional corticosteroid for keloid or hypertrophic
Reali, U. M.
Hypertrophic scars and keloids: Immu-
scars. Korean J. Dermatol. 35: 450, 1997.
nophenotypic features and silicone sheets to prevent
29. Sproat, J. E., Dalcin, A., Weitauer, N., and Roberts, R. S.
recurrences. Ann. Burns Fire Disasters 8: 164, 2000.
Hypertrophic sternal scars: Silicone gel sheeting ver-
49. Quinn, K. J.
Silicone gel in scar treatment. Burns 13:
sus kenalog injection treatment. Plast. Reconstr. Surg.
90: 988, 1992.
50. Morris, D. E., Wu, L., Zhao, L. L., et al.
30. Yii, N. W., and Frame, J. D.
Evaluation of cynthaskin
chronic animal models for excessive dermal scarring:
and topical steroid in the treatment of hypertrophic
Quantitative studies. Plast. Reconstr. Surg. 100: 674,
scars and keloids. Eur. J. Plast. Surg. 19: 162, 1996.
31. Jenkins, M., Alexander, J. W., MacMillan, B. G., et al.
51. Baum, T. M., and Busuito, M. J.
Use of a glycerin-based
Failure of topical steroids and vitamin E to reduce
gel sheeting in scar management. Adv. Wound Care 11:
postoperative scar formation following reconstructive
surgery. J. Burn Care Rehabil. 7: 309, 1986.
52. Phillips, T. J., Gerstein, A. D., Lordan, V., et al.
32. Perkins, K., Davey, R. B., and Wallis, K. A.
randomized controlled trial of hydrocolloid dressing
A new treatment for burn scars and contractures.
in the treatment of hypertrophic scars and keloids.
Burns Incl. Therm. Inj. 9: 201, 1983.
Dermatol. Surg. 22: 775, 1996.
33. Sawada, Y., and Sone, K.
Treatment of scars and ke-
53. Wong, T. W., Chiu, H. C., Chang, C. H., et al.
loids with a cream containing silicone oil. Br. J. Plast.
cream occlusive dressing: A novel non-invasive regi-
Surg. 43: 683, 1990.
men in the treatment of keloid. Dermatology 192: 329,
34. Chang, C. C., Kuo, Y. F., Chiu, H., et al.
silicone, modulates the effects of keratinocytes on fi-
54. Staley, M. J., and Richard, R. L.
Use of pressure to treat
broblasts. J. Surg. Res. 59: 705, 1995.
hypertrophic burn scars. Adv. Wound Care 10: 44, 1997.
PLASTIC AND RECONSTRUCTIVE SURGERY, August 2002
55. Fricke, N. B., Omnell, M. L., Dutcher, K. A., Hollender,
76. Kantor, G. R., Wheeland, R. G., Bailin, P. L., et al.
L. G., and Engrav, L. H.
Skeletal and dental distur-
Treatment of earlobe keloids with carbon dioxide la-
bances in children after facial burns and pressure
ser excision: A report of 16 cases. J. Dermatol. Surg.
garment use: A 4-year follow-up. J. Burn Care Rehabil.
Oncol. 11: 1063, 1985.
20: 239, 1999.
77. Sheridan, R. L., Lydon, M. M., Petras, L. M., et al.
56. Ward, R. S.
Pressure therapy for the control of hyper-
ablation of burns: Initial clinical trial. Surgery 125: 92,
trophic scar formation after burn injury: A history and
review. J. Burn Care Rehabil. 12: 257, 1991.
78. Hulsbergen-Henning, J. P., Roskam, Y., and van Gemert,
57. Tredget, E. E.
Management of the acutely burned up-
Treatment of keloids and hypertrophic scars
per extremity. Hand Clin. 16: 187, 2000.
with an argon laser. Lasers Surg. Med. 6: 72, 1986.
58. Nedelec, B., Ghahary, A., Scott, P., and Tredget, E.
79. Abergel, R. P., Meeker, C. A., Lam, T. S., and Dwyer,
Control of wound contraction: Basic and clinical fea-
Control of connective tissue metabolism by
tures. Hand Clin. 16: 289, 2000.
lasers: Recent developments and future prospects.
59. Agrawal, K., Panda, K. N., and Arumugam, A.
J. Am. Acad. Dermatol. 11: 1142, 1984.
expensive self-fabricated pressure clip for the ear lobe.
80. Kumar, K., Kapoor, B. S., Rai, P., and Shukla, H. S.
Br. J. Plast. Surg. 51: 122, 1998.
situ irradiation of keloid scars with Nd:YAG laser.
60. Linares, H. A.
From wound to scar. Burns 22: 339,
J. Wound Care 9: 213, 2000.
81. Kwon, S. D., and Kye, Y. C.
Treatment of scars with a
61. Rayner, K.
The use of pressure therapy to treat hyper-
pulsed Er:YAG laser. J. Cutan. Laser Ther. 2: 27, 2000.
trophic scarring. J. Wound Care 9: 151, 2000.
82. Alster, T. S.
Improvement of erythematous and hyper-
62. Tilley, W., McMahon, S., and Shukalak, B.
trophic scars by the 585 nm flashlamp pulsed dye laser.
tation of the burned upper extremity. Hand Clin. 16:
Ann. Plast. Surg. 32: 186, 1994.
83. Alster, T. S., Kurban, A. K., Grove, G. L., et al.
63. Johnson, J., Greenspan, B., Gorga, D., et al.
ation of argon induced scars by the pulsed dye laser.
ance with pressure garment use in burn rehabilitation.
Lasers Surg. Med. 13: 368, 1993.
J. Burn Care Rehabil. 15: 180, 1994.
84. Alster, T. S., and Williams, C. M.
Treatment of keloid
64. Kealey, G. P., Jensen, K. L., Laubenthal, K. N., and Lewis,
sternotomy scars with 585 nm flashlamp-pumped
Prospective randomised comparison of two
pulsed-dye laser. Lancet 345: 1198, 1995.
types of pressure therapy garments. J. Burn Care Re-
85. Dierickx, C., Goldman, M. P., and Fitzpatrick, R. E.
habil. 11: 334, 1990.
Laser treatment of erythematous/hypertrophic and
65. Rose, M. P., and Deitch, E. A.
The clinical use of a
pigmented scars in 26 patients. Plast. Reconstr. Surg. 95:
tubular compression bandage, Tubigrip, for burn scar
therapy: A critical analysis. Burns Incl. Therm. Inj. 12:
86. Goldman, M., and Fitzpatrick, R. E.
Laser treatment of
scars. Dermatol. Surg. 21: 685, 1995.
66. Chang, P., Laubenthal, K. N., Lewis, R. W., II, et al.
87. Connell, P. G., and Harland, C. C.
Treatment of keloid
Prospective, randomized study of the efficacy of pres-
scars with pulsed dye lasers and intralesional steroid.
sure garment therapy in patients with burns. J. Burn
J. Cutan. Laser Ther. 2: 147, 2000.
Care Rehabil. 16: 473, 1995.
88. McCraw, J. B., McCraw, J. A., McMellin, A., and Betten-
67. Norris, J. E. C.
Superficial X-ray therapy in keloid man-
Prevention of unfavorable scars using early
agement: A retrospective study of 24 cases and liter-
pulse dye laser treatments: A preliminary report. Ann.
ature review. Plast. Reconstr. Surg. 95: 1051, 1995.
Plast. Surg. 42: 7, 1999.
68. Cosman, B., Crikelair, G. F., Ju, D. M., et al.
89. Wittenberg, G. P., Fabian, B. G., Bogomilsky, J. L., et al.
gical treatment of keloids. Plast. Reconstr. Surg. 27: 335,
Prospective single-blind, randomised controlled study
to assess the efficacy of the 585-nm flashlamp pumped
69. Brown, L. A., Jr., and Pierce, H. E.
Keloids: Scar revi-
pulsed-dye laser and silicone gel sheeting in hyper-
sion. J. Dermatol. Surg. Oncol. 12: 51, 1986.
trophic scar treatment. Arch. Dermatol. 135: 1049, 1999.
70. Levy, D. S., Salter, M. M., and Roth, R. E.
90. Layton, A. M., Yip, J., and Cunliffe, W. J.
irradiation in the prevention of keloids. A.J.R. Am. J.
on intralesional triamcinolone and cryosurgery in the
Roentgenol. 127: 509, 1976.
treatment of acne keloids. Br. J. Dermatol. 130: 498,
71. Edsmyr, F., Larson, L. G., Onyango, J., et al.
therapy in the treatment of keloids in East Africa. East
91. Ciampo, E., and Iurassich, S.
Liquid nitrogen cryosur-
Afr. Med. J. 50: 457, 1973.
gery in the treatment of acne lesions. Ann. Ital. Der-
72. Bailin, P.
Use of the CO2 laser for non-PWS cutaneous
matol. Clin. Sper. 51: 67, 1997.
lesions. In K. A. Arndt, J. M. Noe, and S. Rosen (Eds.),
92. Zouboulis, C., Blume, U., Buttner, P., and Orfanos, C. E.
Cutaneous Laser Therapy: Principles and Methods. New
Outcomes of cryosurgery in keloids and hypertrophic
York: John Wiley, 1983. Pp. 187–200.
scars: A prospective, consecutive trial of case series.
73. Apfelberg, D. B., Maser, M. R., White, D. N., et al.
Arch. Dermatol. 129: 1146, 1993.
ure of carbon dioxide laser excision of keloids. Lasers
93. Ernst, K., and Hundeiker, M.
Results of cryosurgery in
Surg. Med. 9: 382, 1989.
394 patients with hypertrophic scars and keloids. Haut-
74. Norris, J. E.
The effect of carbon dioxide laser surgery
arzt 46: 462, 1995.
on the recurrence of keloids. Plast. Reconstr. Surg. 87:
94. Rusciani, L., Rosse, G., and Bono, R.
apy in the treatment of keloids. J. Dermatol. Surg. Oncol.
75. Bernstein, L. J., Kauvar, A. N., Grossman, M. C., et al.
19: 529, 1993.
Scar resurfacing with high-energy short-pulsed and
95. Reiffel, R. S.
Prevention of hypertrophic scars by long-
flash scanning carbon dioxide lasers. Dermatol. Surg.
term paper tape application. Plast. Reconstr. Surg. 96:
24: 101, 1998.
Vol. 110, No. 2 / SCAR MANAGEMENT RECOMMENDATIONS
96. Davey, R. B., Wallis, K. A., and Bowering, K.
and Ghahary, A.
The antifibrogenic effects of lipo-
contact media: An update on graft fixation and burn
scar management. Burns 17: 313, 1991.
wounds. J. Interferon Cytokine Res. 19: 1413, 1999.
97. Havlik, R. J.
Vitamin E and wound healing: Safety and
114. Tredget, E. E., Shankowsky, H. A., Pannu, R., et al.
efficacy reports. Plast. Reconstr. Surg. 100: 1901, 1997.
Transforming growth factor-beta in thermally injured
98. Baumann, L. S., Spencer, J., and Klein, A. W.
patients with hypertrophic scars: Effects of interferon
effects of topical vitamin E on the cosmetic appear-
alpha-2b. Plast. Reconstr. Surg. 102: 1317, 1998.
ance of scars. Dermatol. Surg. 25: 311, 1999.
115. Berman, B., and Flores, F.
Recurrence rates of excised
99. Jackson, B. A., Shelton, A. J., and McDaniel, D. H.
keloids treated with postoperative triamcinolone ace-
study evaluating topical onion extract as treatment for
tonide injections of interferon alfa-2b injections.
postsurgical scars. Dermatol. Surg. 25: 267, 1999.
J. Am. Acad. Dermatol. 37: 755, 1997.
100. Scalvenzi, M., Delfino, S., and Sammarco, E.
116. Fitzpatrick, R. E.
Treatment of inflamed hypertrophic
matological scars: Improvement after application with
scars using intralesional 5-FU. Dermatol. Surg. 25: 224,
an allantoin and sulphomucopolysaccharide-based
gel. Ann. Ital. Dermatol. Clin. Sper. 52: 132, 1998.
117. Bodokh, I., and Brun, P.
Traitement des chéloïdes par
101. Magliaro, A., Gianfaldoni, R., and Cervadoro, G.
infiltrations de Bléomycine. Ann. Dermatol. Venereol.
Treatment of burn scars with a gel based on allantoin
123: 791, 1996.
and sulfomucopolysaccharides. G. Ital. Dermatol. Vene-
118. Larouy, J. C.
Traitement des chéloïdes: trois méth-
reol. 134: 153, 1999.
odes. Nouv. Dermatol. 19: 295, 2000.
102. Boyce, D. E., Bantick, G., and Murison, M. S.
119. Espana, A., Solano, T., and Quintanilla, E.
of ADCON-T/N glycosaminoglycan gel in the revision
in the treatment of keloids and hypertrophic scars by
of tethered scars. Br. J. Plast. Surg. 53: 403, 2000.
multiple needle punctures. Dermatol. Surg. 27: 23,
103. Widgerow, A. D., Chait, L. A., Stals, R., and Stals, P. J.
New innovations in scar management. Aesthetic Plast.
120. Smith, E. A., Harper, F. E., and LeRoy, E. C.
Surg. 24: 227, 2000.
phenomenon of a single digit following local intra-
104. Janssen de Limpens, A. M. P.
The local treatment of
dermal bleomycin sulfate injection. Arthritis Rheum.
hypertrophic scars and keloids with topical retinoic
28: 459, 1985.
acid. Br. J. Dermatol. 103: 319, 1980.
121. Epstein, E.
Persisting Raynaud's phenomenon follow-
105. Peacock, E. E., Jr.
Pharmacologic control of surface
ing intralesional bleomycin treatment of finger warts.
scarring in human beings. Ann. Surg. 193: 592, 1981.
J. Am. Acad. Dermatol. 13: 468, 1985.
106. Topol, B. M., Lewis, V. L., Jr., and Beneviste, K.
122. O'Kane, S., and Ferguson, M. W.
use of antihistamine to retard the growth of fibroblasts
growth factor beta s and wound healing. Int. J. Biochem.
derived from human skin, scar and keloids. Plast. Re-
Cell Biol. 29: 63, 1997.
constr. Surg. 68: 227, 1981.
123. Yamada, H., Tajima, S., Nishikawa, T., Murad, S., and
107. Duncan, J. L., Thomson, A. W., and Muir, L. F. K.
Pinnell, S. R.
Tranilast, a selective inhibitor of col-
Topical cyclosporin and T-lymphocytes in keloid scars.
Br. J. Dermatol. 124: 109, 1991.
lagen synthesis in human skin fibroblasts. J. Biochem.
108. Lawrence, W. T.
Treatment of earlobe keloids with
(Tokyo) 116: 892, 1994.
surgery plus adjuvant intralesional verapamil and
124. Nakamura, K., Irie, H., Inoue, M., Mitani, H., Sunami,
pressure earrings. Ann. Plast. Surg. 37: 167, 1996.
H., and Sano, S.
Factors affecting hypertrophic scar
109. Tredget, E. E., Wang, R., Shen, Q., Scott P. G., and
development in median sternotomy incisions for con-
genital cardiac surgery. J. Am. Coll. Surg. 185: 218,
mRNA and protein in hypertrophic scar tissues and
fibroblasts: Antagonism by IFN-alpha and IFN-gamma
125. O'Kane, S., and Ferguson, M. W.
in vitro and in vivo. J. Interferon Cytokine Res. 20: 143,
growth factor betas and wound healing. Int. J. Biochem.
Cell Biol. 29: 63, 1997.
110. Granstein, R. D., Rook, A., Flotte, T. J., et al.
126. Cowin, A. J., Holmes, T. M., Brosnan, P., and Ferguson,
trolled trial of intralesional recombinant interferon-␥
Expression of TGF-beta and its receptors in
in the treatment of keloidal scarring. Arch. Dermatol.
murine fetal and adult dermal wounds. Eur. J. Derma-
126: 1295, 1990.
tol. 11: 424, 2001.
111. Pittet, B., Rubbia-Brandt, L., Desmoulieve, A., et al.
127. Tyrone, J. W., Marcus, J. R., Bonomo, S. R., Mogford,
fect of gamma interferon on the clinical and biological
J. E., Xia, Y., and Mustoe, T. A.
Transforming growth
evolution of hypertrophic scars and Dupuytren's dis-
factor beta3 promotes fascial wound healing in a new
ease: An open pilot study. Plast. Reconstr. Surg. 93:
animal model. Arch. Surg. 135: 1154, 2000.
128. Kim, I., Mogford, J. E., Witschi, C., Nafissi, M., and
112. Larrabee, W. F., Jr., East, C. A., Jaffe, H. S., et al.
Mustoe, T. A.
Inhibition of prolyl 4-hydroxylase re-
tralesional interferon gamma treatment for keloids
duces scar elevation in a rabbit model of hypertrophic
and hypertrophic scars. Arch. Otolaryngol. Head Neck
scarring. Wound Repair Regen. 9: 139, 2001.
Surg. 116: 1159, 1990.
129. Harahap, M.
Surgical Techniques for Cutaneous Scar Re-
113. Takeuchi, M., Tredget, E. E., Scott, P. G., Kilani, R. T.,
vision. New York: Marcel Dekker, 1999.
Source: http://www.newgel.co.uk/papers/Mustoe%202002.pdf
CROSS ROADS A Drug Prevention Manual for PSD Teachers • Using the Programme• The Pack & the Curriculum• Notes for Teachers •Expressing Positive Feelings•Dealing with Negative Feelings SEDQA PREVENTION PROGRAMME •Understanding Own Attributes in collaboration with the Education Division •Decision-making - Assertiveness•Smoking and it's Effects
« Bienvenido AL nUevo CUAdeRno AUToinSTRUCTivo PARA eL PPU SECCIÓN DE APTITUD NUMÉRICA Descripción de la prueba Aspectos que evalúa la prueba (matriz)— Números y operaciones— Cambio y relaciones — Geometría LA UNIVERSIDAD PERUANA DE CIENCIAS APLICADAS (UPC) — Estadística y probabilidad TIENE EL AGRADO DE PRESENTARTE EL NUEVO CUADERNO