Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Nirth.res.in
Prospects of Malaria Control in Northeastern India with
Particular Reference to Assam
V.P. Sharma, Vas Dev
Malaria is endemic in the entire northeastern region comprising of 7 states.
P. falciparumis the most predominant species.
P. falciparum has become resistant to chloroquine(CQ) and sulphadoxine pyremethamine (SP) drugs. The principal vectors viz.
An. baimaii(formerly species D of
An. dirus complex),
An. minimus and
An. fluviatilis are highlyefficient in malaria transmission with exophilic and exophagic behavior, and maintainstable malaria in the region. Problems in malaria control and way forward in achievingsustainable malaria control are described.
The present situation of malaria in India is best described as malaria endemic countrywith >95% of her population at risk of malaria. Reported cases of malaria vary from 1.8to 2.0 million (1.2 million in 2006) and 1, 000 deaths per year. WHO SEARO estimates 15million cases and 19,500 deaths, whereas WHO HQs estimates 70 million malaria cases(Sharma, 2005). The proportion of
P. vivax and
P. falciparum is almost equal but itvaries greatly from place to place and seasonally.
P. falciparum is a killer parasite and ithas become resistant to chloroquine with reports of resistance to other antimalarialdrugs.
P. vivax is sensitive to chloroquine but in the last decade resistance to chloroquinehas been reported from a few places in the country (Dua et. al. 1996). The totalnumber of cases and the percentage of
P. falciparum are rising as a result of fall in
P.
vivax. Furthermore clinical profile of
P. falciparum patients is becoming more severewith increasing trend of renal and respiratory complications and multi-organ failure (B.S.
Das, Personal Communication, formerly at the Ispat Hosptial Rourkela). The major vectorof malaria
An. culicifacies responsible for generating 65% malaria cases has developedresistance to DDT and Malathion (Sharma, 1996). Synthetic pyrethroids are beingsprayed to control the emerging epidemics. Multiple insecticide resistant mosquito strainshave emerged so that malaria control is attainable partially, if at all. Malaria returns yearafter year requiring spraying, but due to limited resources spraying is carried out in 10%endemic population. National Anti Malaria Programme (NAMP) has been renamed as theNational Vector Borne Disease Control Programme (NVBDCP) making it accountable forthe control of all vector borne diseases. Malaria epidemics have become commonplaceand more devastating. Emergency measures are adopted to suppress the epidemics.
This produces transient relief, but the over all picture remains unchanged. New diseasesare emerging and spreading e.g. Dengue and Dengue Hemorrhagic Fever (DHF) andChikungunya virus fever (CHIKV). NVBDCP is spending its limited resources in fightingthe re-emerging arboviral diseases (Lahariya and Pradhan, 2006; Bhargava and Chatterjee,2007; NVBDCP Website). Malaria control in the tribal settlements is to be seen in theabove background of rapidly deteriorating situation of vector borne diseases and resourcecrunch.
Proceeding of National Symposium on Tribal Health
India has 635 tribes and constitutes 7.8 % of the country's population. The tribalpopulation is 87.7 million. Bulk of this population is scattered in 8 states. Almost allpopulation of northeastern states belong to tribal group which has a separate fundingmechanism i.e. malaria control in NE states is a centrally sponsored activity sinceDecember 1994. Therefore central government contribution has no restriction of 50%matching grant from the states. That makes malaria control more sustainable in as faras the resources are concerned. Tribal malaria control generally refers to the EnhancedMalaria Control Project (EMCP) launched with World Bank (WB) financing to cover 1,045Primary Health Centre (PHCs) in 100 predominantly tribal and malaria endemic districtsin 8 states namely, Andhra Pradesh, Bihar, Chhatisgarh, Gujarat, Jharkhand, MadhyaPradesh, Maharashtra and Orissa. Enhanced Malaria Control Project (EMCP) was launchedwith World Bank funds in September 1997 with the objective to strengthen malariacontrol by additional inputs through a mix of interventions. While malaria control in theEMCP areas of 8 states is being presented by other investigators (Sharma, 1999). Iwish to briefly describe the tribal malaria situation in the northeastern states, in particularthe state of Assam.
The population of northeastern (NE) states is 39 million i.e. 3.96% of the country'spopulation. Of the total burden of malaria in India, NE states contribute 10% malariaand 11%
P. falciparum cases and 20% malaria deaths. Malaria control depends oneffective vector control. In the NE region malaria vectors are viz.,
Anopheles minimus(perennial species),
An. baimaii (monsoon species), and
An. fluviatilis (winter species).
All these mosquitoes are highly efficient in the transmission of malaria (Dev, 1996; Devet. al. 2001). Malaria vectors are susceptible to DDT, HCH, Malathion and SyntheticPyrethroids but because of the exophilic and or exophagic vector behavior they avoidresting on the sprayed walls, and thus avoid the killing action of insecticides. Thesituation is further complicated by high proportion of
P. falciparum >60%), a killerparasite that has become multi-drug resistant (Dua et. al. 2003; Dev et al, 2003). Table1 gives the areas and population involved in cross-border malaria.
P. falciparum is thedominant parasite all along the international borders which is widely disseminated bythe population movement on both sides of the international borders.
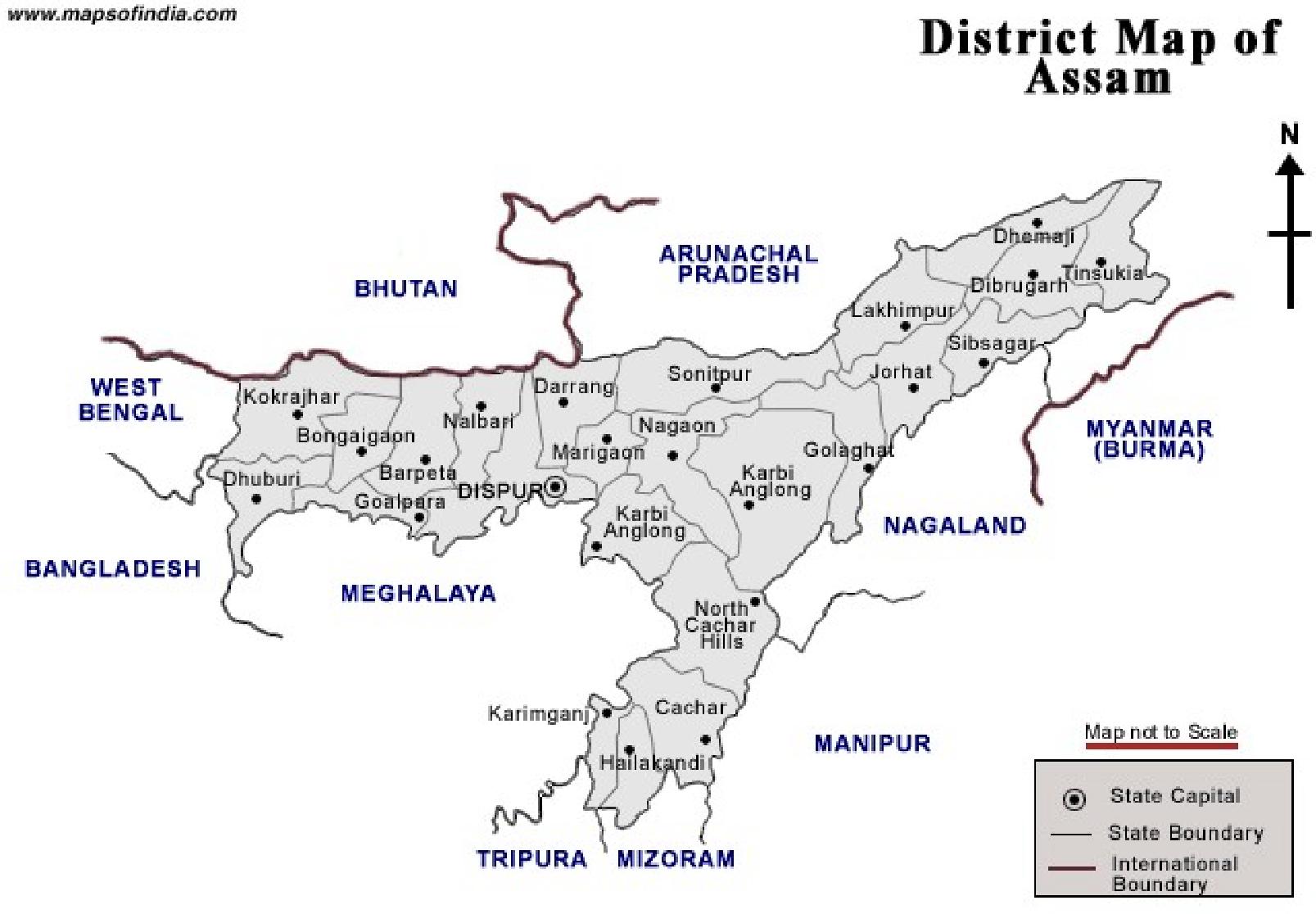
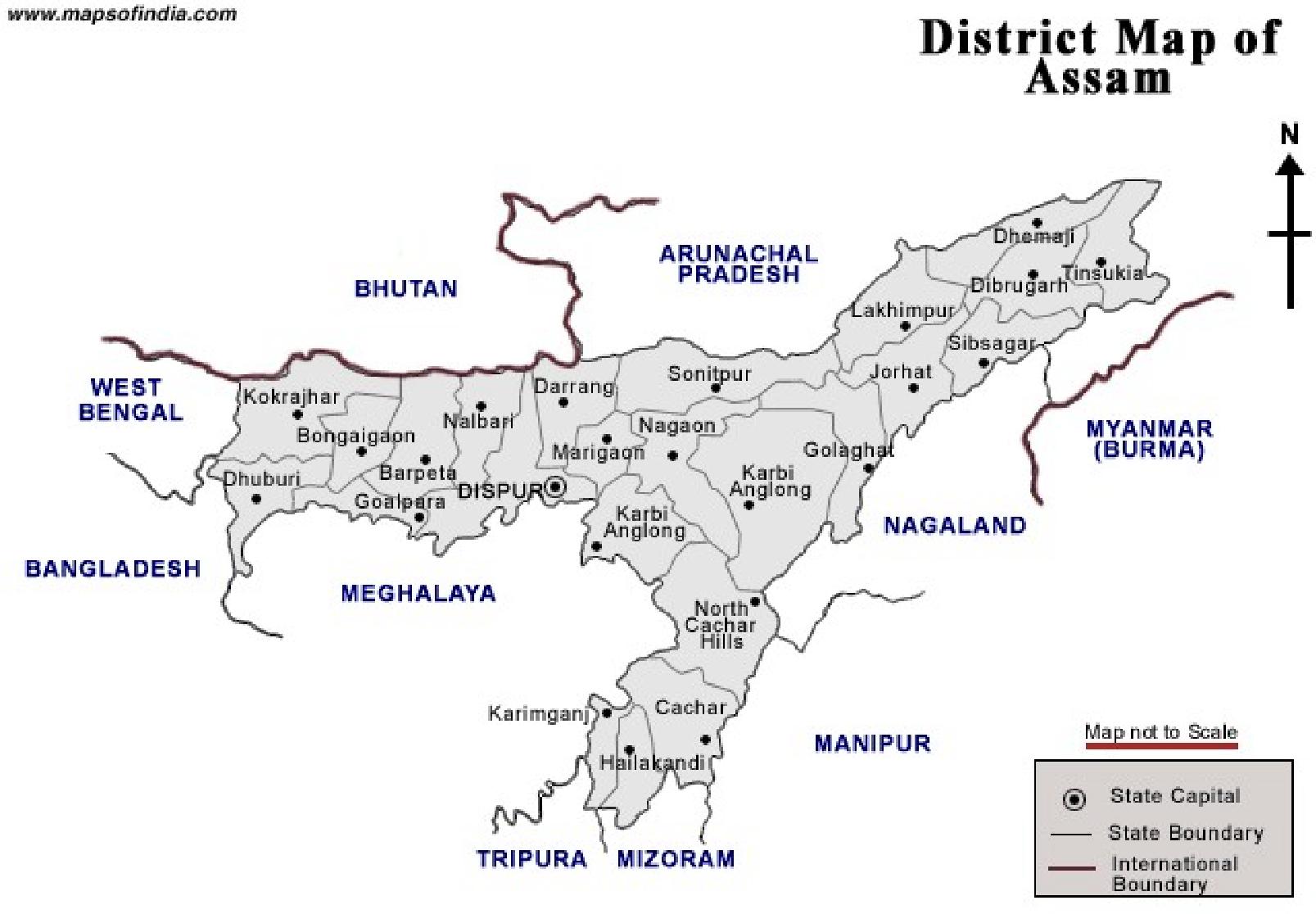
Fig. 1 gives the location of districts in Assam. Fig. 2 gives the An. minimus man hourdensities in Sonapur PHC villages. High densities are encountered from March-April tillthe end of August and these are related to rainfall. Fig 3. gives the malaria incidence(Pv and Pf) over a three year period. Malaria peaks during the rainy season. It isnotable to mention that environmental determinants favor malaria transmission almostthroughout the year except a brief period of interruption due to cold weather (Dev et.
al. 2006a). Table 2 gives the epidemiological situation of malaria in Assam. NVBDCPreports declining trend of malaria each year and in 2006 1.2 million cases were reported(lowest since resurgence in 1976). It is notable to mention that malaria situation inAssam is grim as is evident by the fact that in 2006, malaria cases have doubled, and300 malaria deaths were reported from 23 districts. An estimated one million populationof 66 PHCs and 1,720 villages were severely affected in the outbreaks. Malaria is alsoaffecting the economic zones of the state e.g. tea gardens and industrial belts of thestate.
Sharma, Dev
Table 1: Malaria profile of inter-border populations of Assam*
International bordering
14634 (7.5) 5008 (2.6)
19536 (7.9) 4661 (1.9)
*Data based on the year 2001 (Source, State Health Directorate)
Table 2: Malaria incidence in Assam
Source: State VBDCP
Proceeding of National Symposium on Tribal Health
Fig. 1: District map of Assam
Fig. 2: Trend of Anopheles minimus densities (measured as man hour density)
in Sonapur PHC, Kamrup district, Assam
Sharma, Dev
Fig 3: Trend of malaria in relation to environmental conditions in Sonapur PHC,
Kamrup district, Assam.
Note the perennial malaria transmission with peaks during the rainy season
High densities are encountered from March-April till the end of August and these arerelated to rainfall.
In Assam malaria cases were detected in all months of the year and peaks during
May–June, which coincides with rainy months. These were also the months with highestincidence of infection with P. falciparum. Malaria cases were detected in all age groupsof both sexes, and there was clustering of cases in villages near the vector-breedinghabitat (perennial seepage streams), and foothill villages. However, malaria cases wereconsistently low in villages within 5-km of the nearest health care facility, which were intown areas (Dev et. al. 2004). Another study (Dev et. al. 2006) revealed that the maintransmission season of malaria in Sonapur PHC, Kamrup district in Assam was the wetseason from April to September and malaria cases were low during the dry season fromOctober to March. Indian Tea Association has reported >66%. P. falciparum was theprevalent infection in almost all tea gardens on the north bank of Brahmaputra riveroften causing epidemics. Anopheles minimus was positive with sporozoites almostthroughout the year. The EIRs per person/night were 0.46–0.71 in P. falciparum-predominant areas and 0.12 in the district where P. vivax predominated (Dev et. al.
2004).
Malaria control in Assam required innovative approaches. Therefore for the first
time insecticide treated mosquito nets (ITMN) were introduced in endemic villages(Jana-Kara et. al. 1995). Based on this experience in Assam and to promote the nationalpolicy of the insecticide treated bed nets as the main strategy of malaria control,transfer of technology workshops were organized in all the NE states as shown in Table3.
Proceeding of National Symposium on Tribal Health
Table 3: Technology transfer of the insecticide treated bed nets in the North-
Deltamethrin 2.5%
Table 4: Impact assessment of insecticide treated bed nets on malaria trans-
mission in the northeastern states
Jan '95 –Dec ‘95
Jan '96 –Dec ‘96
Jan '95 –Dec ‘95
Jan '96 –Dec ‘96
Jan '95 –Dec ‘95
Jan '96 –Dec ‘96
* Jan 1995 –Dec 1995 is the base line year data. Mosquito Nets Treated with Deltamethrine (2.5%flow) were introduced in January 1996.
Source: Data collected by the respective State Health Dte through primary health care system (for theremaining northeastern states, the distribution of nets was irregular and patchy, thus data could not beevaluated). The re-treatment of nets was not conducted as scheduled, thus data of the subsequent
Sharma, Dev
years could not be considered.
Simultaneously ITMN were distributed in the endemic villages by the trained
staff, who also monitored the impact of ITMN. Table 4 gives the results of ITMN on themalaria incidence. There was remarkable improvement in malaria situation compared tothe malaria situation in the neighboring villages held as control.
Table 5 gives the people's response to the ITMN programme. A very high per-
centage of people reported the benefits from sleeping under the ITMN, and ITMN userspreferred nets over the spraying. Over a period of time additional demand of ITMN wasgenerated, although poverty prevented people from opting for the ITMN, if not providedfree by the government.
Table 5: Response surveys among ITMN users
% Positive Response
Reporting discomfort
(headache, itching)
Reporting benefits
Would like to continue using
Would like to buy own nets
Problems in Malaria Control
Malaria control in the NE faces many challenges. Inter alia these challenges are:
Tropical rain-forest rich in wild life including reserve forests and sanctuaries,interspersed with valleys, hills and settlements making the region highly receptivefor maintaining perennial malaria transmission;
Schedule tribes and scheduled castes comprise of 12.8% and 7.4% respectivelyand suffer from neglect and high levels of poverty, and about 30-40% populationof Assam lives below the poverty line which is a big driver for maintaining perennialtransmission (Sharma, 2003);
Vast areas inundated with floods annually;
Inaccessible settlements that remain cut off during the rainy season which happensto be the peak transmission season;
Unrest in some areas hampering work ;
Weak to non-existent health infrastructure;
P. falciparum predominant in most areas of the state resulting in high morbidityand mortality and unaffordable treatment cost;
Proceeding of National Symposium on Tribal Health
High proportion of carriers;
Presence of mono and multi-drug resistance;
10. Stable malaria except small pockets with unstable malaria;
11. International borders encouraging cross-border malaria;
12. Presence of highly efficient vectors viz., An. minimus, An. baimaii (formerly species
D of An. dirus complex) and An. fluviatilis;
13. Poor and scattered houses mostly made of mud and bamboos;
14. Tribal rely on traditional methods of treatment and healers;
15. Population migration and nomadic behavior;
16. Deforestation and man made changes in the ecology etc;
17. Gross under-reporting of cases gives a false sense of good performance. Burden of
malaria is high and available data does not reflect true malaria incidence;
18. Malaria control based on DDT spraying to control exophilic and exophagic vector
populations, whereas most transmission is extra-domiciliary;
19. Environment of the NE states is highly receptive for malaria transmission;
20. There is almost round the year transmission with peaks following rains. Vast areas
are inaccessible, remain cut off during the rainy season;
21. There are vacancies at all levels and shortage of essential medicines.
There are many more administrative and socio-economic problems hampering
successful malaria control in the NE states. All the above factors work in unison tomaintain perennial malaria transmission.
Way Forward
1. Health Infrastructure: De-centralize malaria control to district level, eliminating all
controls from the Centre. The responsibility should be shifted to Zila Parishad. Initially
some problems may arise but gradually experienced and trained cadre would rise to the
occasion, and successfully tackle the specific problems at the micro-level. Training and
re-training should be an in-built component of the district health infrastructure. Training
courses should be prepared for each category of staff keeping in mind the local
requirement of malaria planning and control. A regular system of laboratory checks and
counter checks should be maintained so that staff is in place, and supplies are available
at the lowest level of health system. The region should have norms of the primary
health care system considering the terrain and ecology of the region to ensure adequate
coverage. Furthermore planning and implementation of malaria control should be based
on more realistic assessment of the disease burden in the NE. Accelerated economic
and infrastructure development is urgently needed to improve this situation.
2. Stratification: Each district should take up malariogenic stratification based on
DALYs, malaria risk maps should be prepared and updated periodically, hot spots of
malaria should be highlighted for preventive action, prioritize economically important
areas (e.g. tea gardens, industrial areas, defence establishments, R & D organizations
Sharma, Dev
etc.) for interventions. Based on the above information a calendar of activities shouldbe prepared and all supplies arranged before time. Community participation must beensured and they should be made aware of their rights, privileges and responsibilities.
There should be complete transparency in the planning and implementation of themalaria control activities and communities should be taken into confidence, and madepartner from the very beginning.
3. Vector Control: Malaria control in NE is based on the indoor residual spraying of DDT.
In the last 30 years, since the resurgence started malaria picture in Assam has remained
more or less static, although DDT was being sprayed. DDT spraying should stop forthwith
(Sharma, 2003a). Malaria control should rely on the use of insecticide treated mosquito
nets; preferable long lasting insecticide bed nets (LLINs). Wherever it is feasible
bioenvironmental methods of vector control must be introduced for long-term sustainable
malaria control. Drainage should be organized to channelise streams and stagnant water
bodies to control mosquito breeding. Care should be taken to maintain the ecological
integrity of the region. Removal of streams/water bodies from the vicinity of human
settlements up to 1 -1.5 km (the flight range) should be practiced. This strategy will
protect from the bites of vector species viz., An. minimus and An. fluviatilis. Wherever
feasible, bioenvironmental methods of vector control should be applied to control the
mosquitoes. All efforts should be made to maximize preventive vector control coverage.
It may be noted that malaria control in NE requires sustained and multi-pronged attack
on the disease.
4. Parasite Control: In areas where laboratory services are deficient or not available,
dipstick method of diagnosis should be introduced. WHO guidelines for the treatment of
malaria should be followed. Quinine is currently used in the treatment of severe malaria
cases. Quinine should be replaced with the artemisinin as the later provides early
recovery and saves more lives (Woodrow et. al. 2005). Monitoring of drug resistance
should be a continuing process for updating drug policy. Equipping hospitals and training
of para-medicals and medical staff should be given priority for correct and efficient
treatment of patients. There is high prevalence of multi-drug resistant malaria in the NE
states. The existing malaria drugs such as chloroquine, sulphadoxine-pyremethamine,
mefloquine etc. are inefficient and pose the danger of accelerated resistance. WHO
now recommends that the treatment of P. vivax may continue with chloroquine but for
the treatment of P. falciparum fixed dose artemisinin based combination therapy (ACT)
should be adopted as the national drug policy (Sharma, 2006). This policy is being
adopted widely throughout the world and there is no scientific basis or rationale to
continue with the outdated drug policy.
5. Epidemic Malaria: Malaria epidemics visit the state of Assam with increasing fre-
quency leading to high morbidity and mortality. Early warning system should be devel-
oped for early preventive action. Each district should have well trained staff that can
be drafted to fight the epidemics. Epidemic malaria control may require spraying with an
efficient insecticide like the synthetic pyrethroids supported by the intensive surveil-
lance to detect all parasite positive cases. In some areas mass drug administration or
mass radical treatment may be required. Standard techniques and norms should be
followed in the control of malaria epidemics. Patient care in the hospital must be strength-
ened. Medical and para-medical staff should be trained in the management of severe
malaria. Malaria audit must be carried out to pin down the causes of deaths due to
Proceeding of National Symposium on Tribal Health
malaria, and areas of weakness must be strengthened. A recent finding is that inmalaria cases iron supplementation to treat anemia may enhance severity of the dis-ease.
6. Border Malaria: Malaria control along the international borders should receive spe-
cial attention. WHO should be requested to organize border meetings on regular basis
so as to implement an agreed strategy on both sides of the international border. Check-
points should be set up to test migrant population for the presence of malaria parasites.
Carriers can spread malaria, particularly new strains that are more lethal. Blood test
should be made an essential requirement for labor hired by the contractors, engineering
departments, and labor-intensive development agencies.
7. Malaria Awareness: Information, Education and Communication (IEC) should become
a continuing activity to help strengthen early case detection and prompt treatment
(EDPT), use and care of bed nets (LLINs/treated nets), eliciting people's participation in
vector control, and encouraging inter and intra sectoral coordination.
Bhargava, Anurag, Biswaroop Chatterjee. 2007. Chikungunya fever, falciparum malaria,dengue fever, Japanese encephalitis are we listening to the warning signs for publichealth in India? Ind. J. Med. Ethics,.Vol.3(1).pp18-23.
Dev V. 1996. Anopheles minimus: its bionomics and role in the transmission in malaria inAssam, India. Bull. World Health Organ.Vol.74.pp61-66.
Dev VC, Hira R, Rajkhowa MK. 2001. Malaria - attributable morbidly in Assam, northeasternIndia. Ann. Trop. Med. Parasitol. Vol.95.pp789 -796.
Dev VS. Phookan, Barman K. 2003. Therapeutic efficacies of antimalarial drugs in thetreatment of uncomplicated Plasmodium falciparum malaria in Assam, north-easternIndia. Ann. Trop. Med. Parasitol. Vol.97.pp783-791.
Dev VS. Phookan, Sharma VP, Anand SP. 2004. Physiographic and entomologic riskfactors of malaria in Assam, India. Am. J. Trop. Med. Hyg. Vol.71(4).pp451-456Dev VS, Phookan, Sharma VP,. Dash AP and. Anand SP. 2006. Malaria parasite burdenand treatment seeking behavior in ethnic communities of Assam, Northeastern India. J.
Infection. Vol.52.pp131-139.
Dev V., Sharma VP, Dash AP. 2006a. Seasonal prevalence of Plasmodium vivax andPlasmodium falciparum malaria in Assam. In Vector Biology. Eds. V.P. Sharma and JagbirSingh, The National Academy of Sciences, India. pp70-80.
Dua VK, Kar PK, Sharma VP. 1996. Chloroquine resistant Plasmodium vivax malaria inIndia. Trop. Med. Intenl. Hlth.. Vol.1.pp816-819.
Dua VK, Dev V, Phookan S, Gupta NC,. Sharma VP, Subbarao SK. 2003. Multi-drugresistant Plasmodium falciparum malaria in Assam, India: Timing of recurrence andantimalarial drug concentrations in whole blood. Am. J. Trop. Med. Hyg. Vol.69.pp555 –557.
Jana-Kara BR, Wajihullah WA, Shahi B, Dev V, Curtis CF, Sharma VP.1995. Deltamethrin
Sharma, Dev
impregnated bed nets against
Anopheles minimus transmitted malaria in Assam,
India. J. Trop. Med. Hyg.Vol.98.pp73-83.
Lahariya C, Pradhan SK. 2006. Emergence of Chikungunya virus in Indian subcontinentafter 32 years: a review. J. Vector Borne Dis. Vol.43.pp151-160.
Sharma VP. 1996. Re-emergence of malaria in India. Indian J. Med. Res.Vol.103. pp26-45.
Sharma VP. 1999. Current scenario of malaria in India. Parassitologia. Vol.41.pp349-353.
Sharma VP. 2003. Malaria and poverty in India. Curr. Sci. Vol.84 (4).pp513-515.
Sharma VP. 2003a. DDT: The fallen angel. Curr. Sci, Vol.85 (11).pp1532-1537.
Sharma VP. 2005. Getting to grips with malaria: a view from India. SciDev.net
Sharma VP. 2006. Artemisinin drugs in the treatment of Plasmodium falciparum malariain India. Curr. Sci. Vol.90(10).pp1323-1324.
Woodrow CT. Planche and Krishna S .2005. Artesunate versus quinine for severe falciparummalaria. Lancet. Vol.367 (9505).pp110-111.
Source: http://www.nirth.res.in/publications/nsth/4.VP.Sharma.pdf
TROUBLE DE L'ATTENTION AVEC OU SANS Dr Olivier REVOL, Neuropsychiatre – Hôpital neurologique - LYON Conférence APEDYS – VOIRON - Mars 2006 Notes : M. JACQUEMET. Le Dr REVOL dirige le service de Neuropsychologie de l'enfant à l'Hôpital neurologique de LYON.Ce service reçoit des enfants en difficultés générales : des anorexiques, des dépressifs, des phobies scolaires. Il comprend 22 lits dont la moitié est consacrée au Centre de référence des troubles de l'apprentissage. En 2001 un rapport a été déposé au Ministère de la Santé et au Ministère de l'Education Nationale, à la demande de Ségolène ROYAL, pour alerter sur la situation en France : on est en retard par rapport aux autres pays européens sur l'évaluation et la prise en charge des enfants en difficulté scolaire. A la suite, une quinzaine de Centres de référence ont été créés, à GRENOBLE, St ETIENNE, LYON. Ce dernier se divise en quatre services, dont celui dirigé par le Dr REVOL. Ces centres ont pour mission d'évaluer les enfants en difficultés scolaires, de comprendre l'origine, et ensuite proposer une prise en charge, mettre en place des réseaux, informer, comme au biais de cette conférence, les professionnels, les parents, les enseignants et les médecins.A l'Hôpital neurologique, parmi les spécificités, figure le travail sur les enfants instables et les enfants précoces.10 enfants entrent chaque semaine dans ce service, adressés par des professionnels, médecins scolaires, orthophonistes, médecins, psychiatres. Ils restent du lundi au vendredi pour un bilan.
Addressing the Challenges in particular, is referred to as the *1 or wild-type allele. The (TA)7 and (TA)8 of the Clinical Application repeats are associated with low UGT enzymatic activity.3 For the purposes of of Pharmacogenetic Testing this article, we focus on the variant (TA)7, or *28, allele because it has received the