Pr040001542p
Cosmetic Special Topic
Textured-Surface Saline-Filled Silicone BreastImplants for Augmentation Mammaplasty
Scott L. Spear, M.D., Mohamed Elmaraghy, M.D., and Christopher Hess, M.D.
Washington, D.C.
The earliest silicone breast implants were smooth-sur-
sues include but are not necessarily limited to
face, silicone rubber devices filled with either silicone gel
toxicity, immunogenicity, teratogenicity, carci-
or saline. Because of persistent problems with capsular
nogenicity, and potential interference with
contracture, polyurethane-covered silicone implants weredeveloped as an alternative. Particularly in the short run,
mammography. Efficacy issues include but are
these alternatives proved highly successful at reducing the
not necessarily limited to risks of capsular con-
incidence of capsular contracture. By 1990, polyurethane-
tracture, deflation, palpability, and rippling.
covered implants were rapidly becoming the preferred
The distinction between textured and smooth
implant choice of many plastic surgeons, but for legal,
saline devices is largely one of efficacy, al-
regulatory, financial, and safety reasons they were with-drawn from the market by Bristol-Myers in 1991. Mean-
though there is some evidence that there may
while, during the late 1980s, surface texturing and im-
be more particulate silicone shed from the
proved materials became available on other silicone breast
surface of textured implants than smooth
implants and expanders. Most studies suggest that tex-
ones.39 The medical significance of such shed-
tured-surface silicone gel–filled implants, saline-filled im-
ding is unclear.
plants, and tissue expanders have less frequent capsularcontracture than their smooth-surface counterparts.
The early history of silicone breast implants
(
Plast. Reconstr. Surg. 105: 1542, 2000.)
involved the use of saline-filled or silicone gel–filled devices with smooth silicone surfaces. Al-though both of those implant types were sub-
Textured-surface, saline-filled silicone im-
stantial improvements over earlier options
plants are one of several options available to-
such as Ivalon sponges, they too ultimately suf-
day for breast augmentation. Understanding
fered from a significant risk of capsular con-
their appropriate use requires a review of the
tracture.1–4,13–16 For reasons of efficacy, silicone
history of breast implant development, includ-
gel implants were more popular than saline-
ing the development of textured surfaces.1–40
filled implants from the beginning. Thus,
The literature on this subject can be confusing;
much of the early literature and clinical energy
thus, it is important to make certain distinc-
surrounding silicone implants dealt with sili-
tions clear from the outset. Tissue expanders
cone gel implants and potential for their cap-
are different devices than implants and behave
sular contracture, including its cause and
differently than implants. Data relevant to tis-
avoidance. Factors implicated in the develop-
sue expanders are not necessarily true for im-
ment of capsular contracture included surgical
plants and vice versa.18 Similarly, silicone gel–
technique, bleeding, subclinical infection, pa-
filled breast implants are different devices than
tient sensitivity, soft-tissue environment, and
saline-filled implants.3,4 The evidence regard-
even silicone itself. Some of the most common
ing textured, silicone gel–filled implants is not
strategies used in an attempt to defeat capsular
necessarily relevant to saline-filled devices. Fi-
contracture included systemic antibiotics, local
nally, for reasons that are not well understood,
antibiotics, steroid solution irrigations, intralu-
animal research of breast implants has been a
minal steroids, submuscular placement, low-
poor predictor of clinical outcomes.12,18,26
bleed silicone elastomer shells, underfilled im-
The evaluation of breast implants necessarily
plants, double-lumen implants, and saline-
covers two areas: safety and efficacy. Safety is-
filled implants.
From the Division of Plastic Surgery, Georgetown University Medical Center. Received for publication February 25, 1999; revised May 18, 1999.
Vol. 105, No. 4 / AUGMENTATION MAMMAPLASTY
The nearly universal experience by plastic
about the fate and toxicity of the polyurethane,
surgeons that early-generation, smooth, sili-
the evidence is substantial that these implants
cone gel–filled breast implants placed in the
were impressively resistant to capsular contrac-
subglandular plane had a significant risk
ture, particularly for the first decade or so after
of developing capsular contracture led, in part,
their implantation.9–11,16,40 The increasing pop-
to the development of the polyurethane-
ularity of polyurethane-covered implants
covered silicone gel–filled breast implant
through the 1980s coupled with their favorable
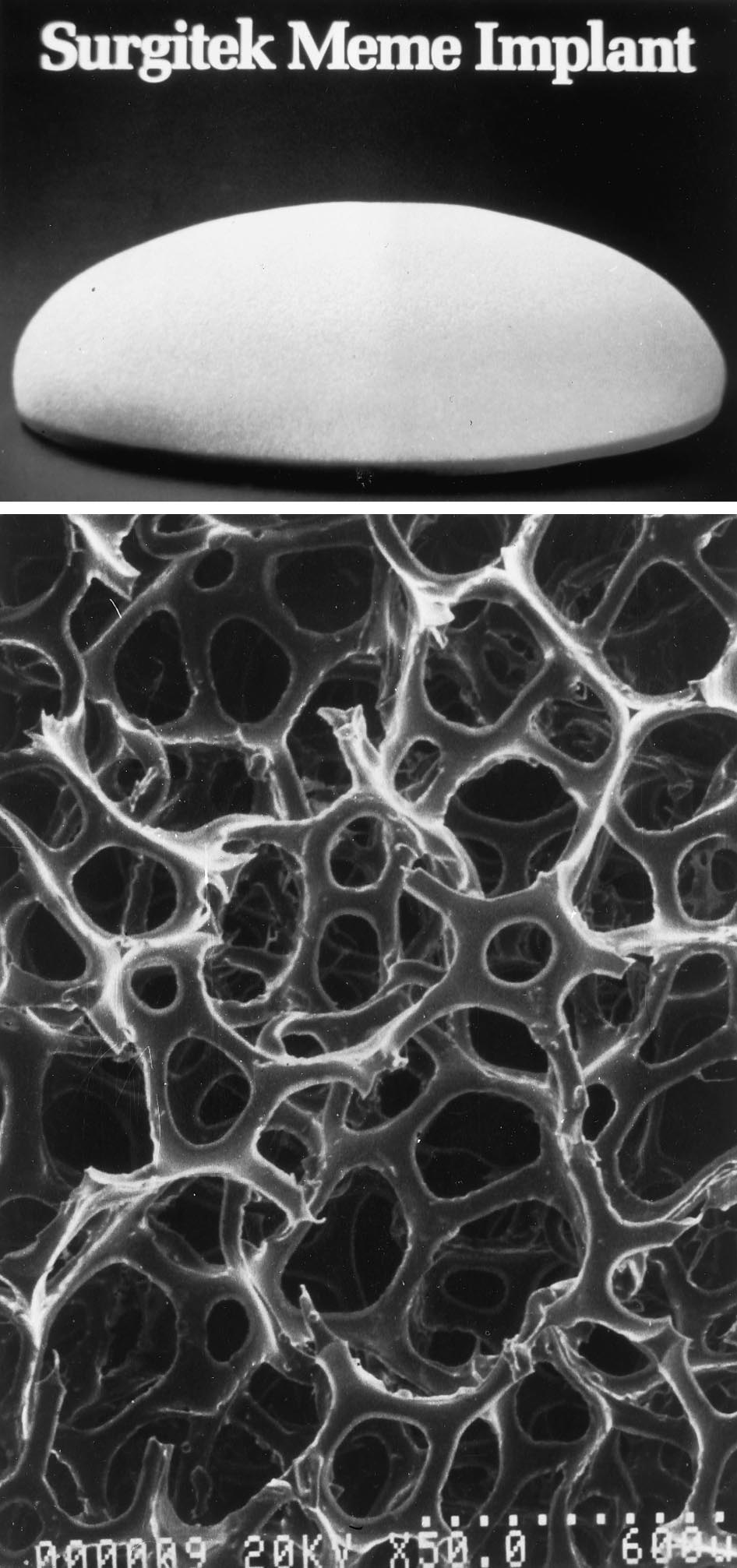
(Fig. 1).1,5–7,9–11 Although there were more than
record of infrequent capsular contracture nat-
one type and manufacturer of polyurethane-
urally led to a search for other options in tex-
covered implants and although they have al-
tured surfaces that would avoid the long-term
ways been associated with nagging questions
doubts about polyurethane. In particular,there was the need of avoiding the possiblebreakdown products of polyurethane andavoiding the separation or delamination of thetextured surface from the implant. This wastrue because the generally favorable reportsregarding the use of polyurethane were tem-pered by some reports of late capsular contrac-ture after the textured surface had delami-nated from the implant, thus, effectivelyconverting it to a smooth-surface device.
During the same time period of the 1970s
and 1980s, other steps had also proven some-what effective in dealing with the frequency ofcapsular contracture, particularly the use oflow-bleed elastomer shells and saline-fill solu-tions, both of which effectively reduced theamount of silicone gel to which the tissues wereexposed.3,4,13,21,22,24,28,36
Thus, textured-surface, silicone implants
were developed in the late 1980s as an obviousalternative to the attached textured surface ofpolyurethane. Because of earlier work to im-prove the performance and decrease the sili-cone permeability of the elastomer shells, thetextured-surface, silicone elastomer shells weredeveloped at a time when all silicone breastimplants were becoming available as strongerand less permeable versions of earlier materi-als. Four different types of textured surfaceswere available more or less simultaneously:polyurethane, Biocell, MSI, and Siltex.
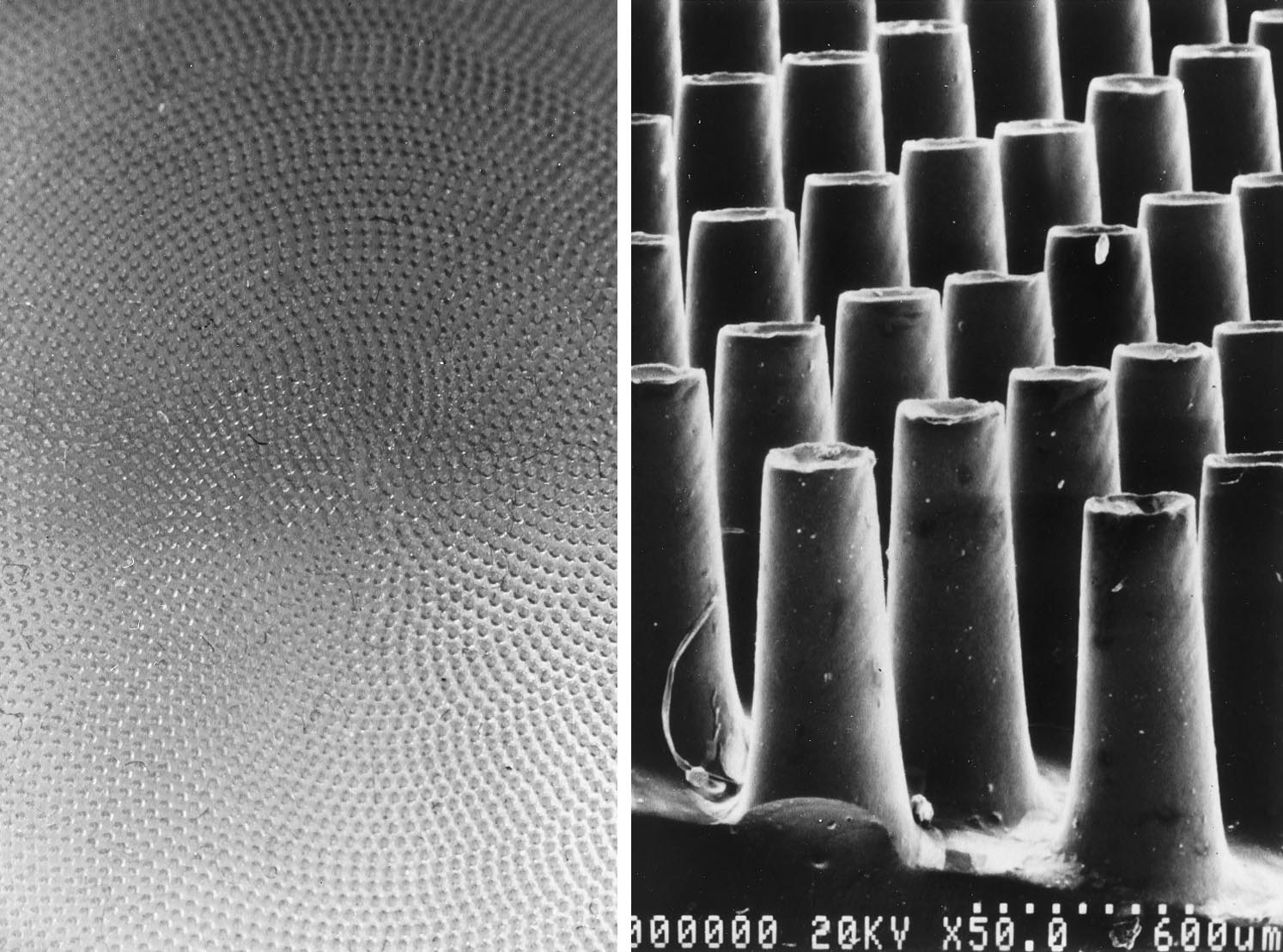
Dow Corning developed and manufactured
the MSI surface, which is an extremely regularsurface of projecting, minute silicone rubberpapillae created with laser technology (Fig. 2).
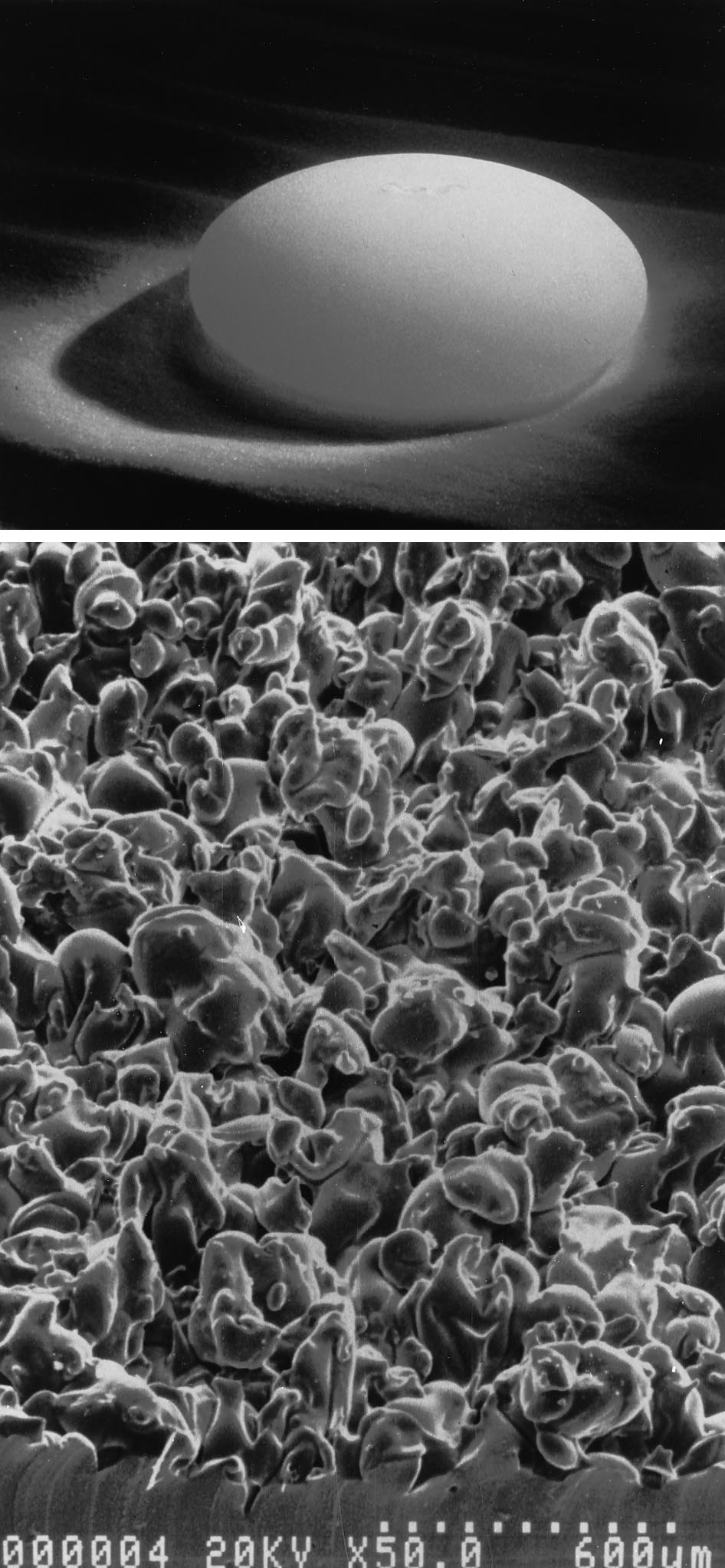
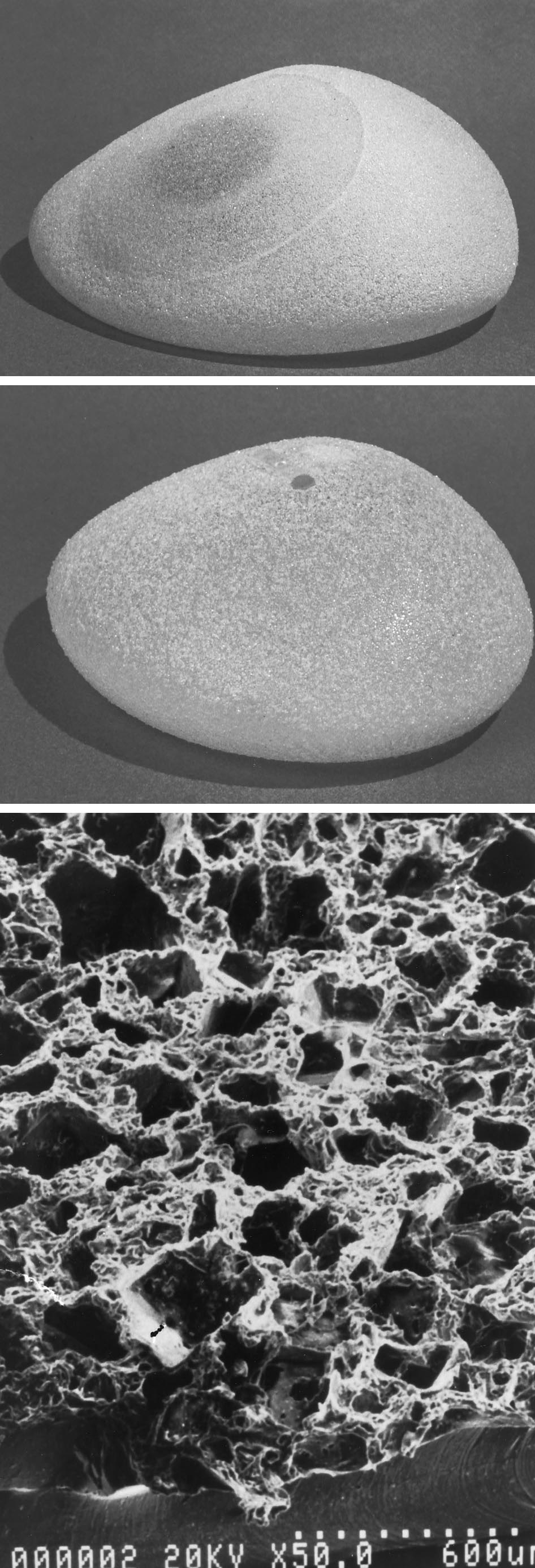
Mentor Corporation developed the Siltex sur-face, which is a patterned surface created as anegative contact imprint off of a texturingfoam (Fig. 3). The McGhan Medical Corpora-tion developed the Biocell surface, which is anaggressive open-pore textured surface createdwith a lost-salt technique and that seems, at
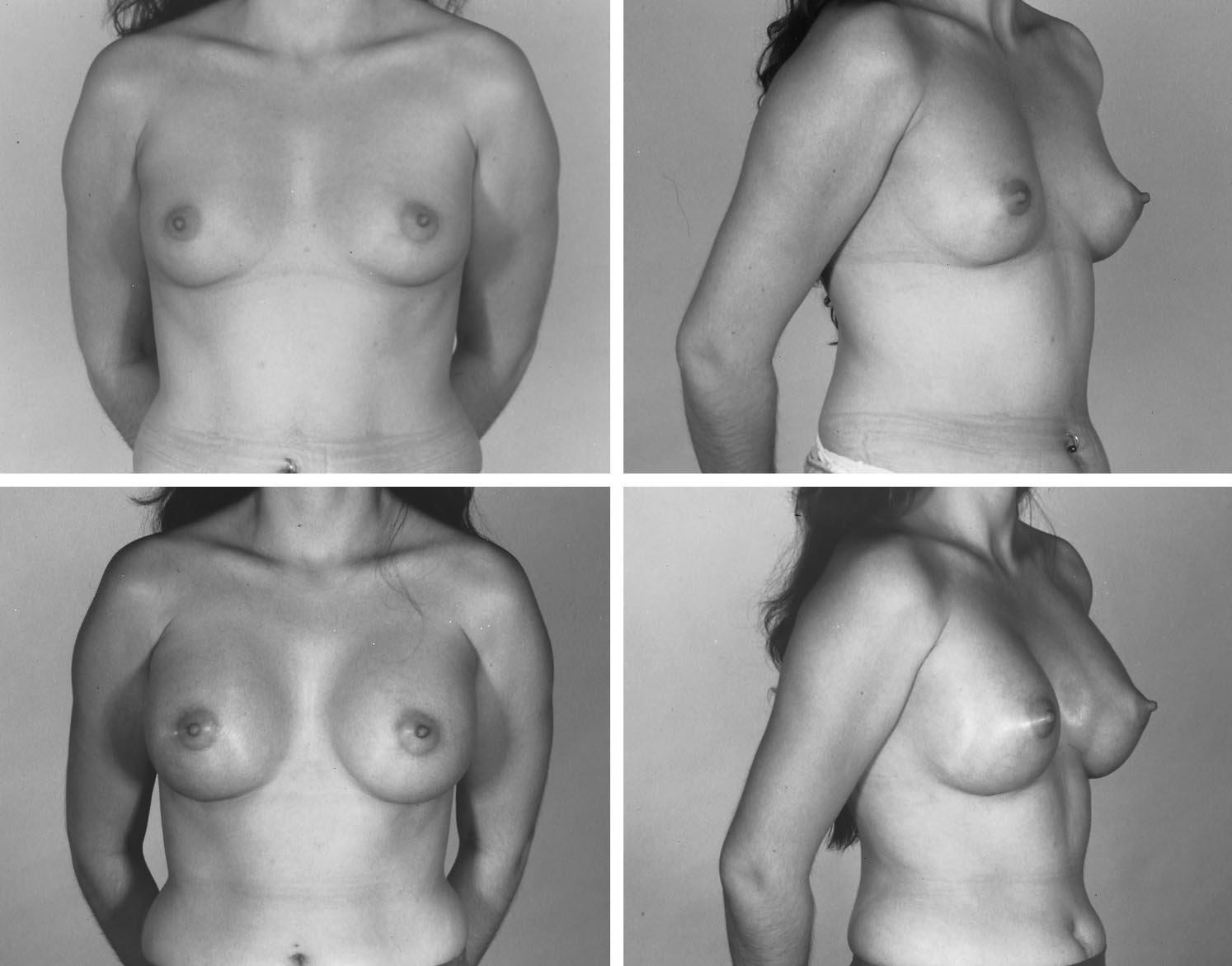
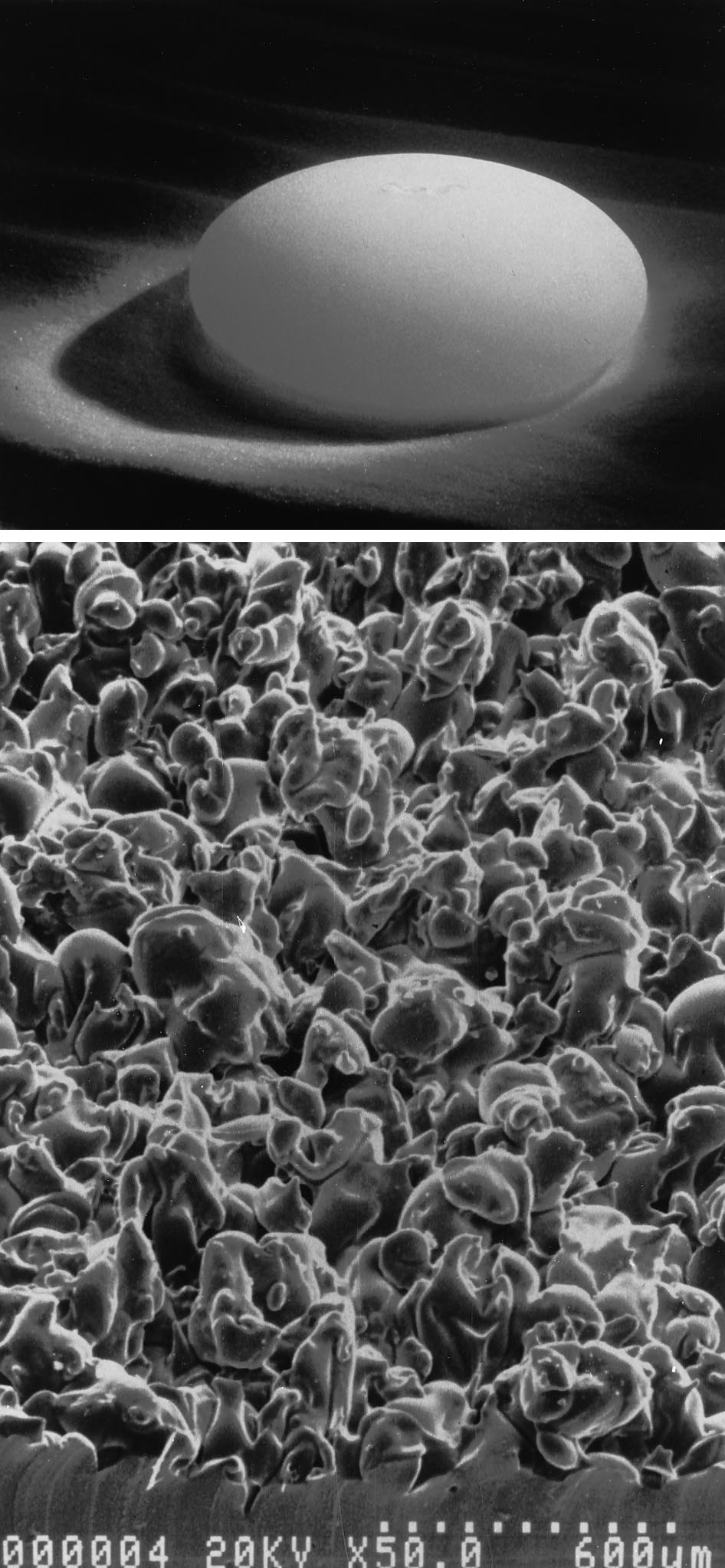
FIG. 1. (Above) Polyurethane-covered silicone gel-filled
breast implant. (Below) The appearance of the polyurethane
least in many ways, similar to polyurethane
as seen by electron microscopy.
PLASTIC AND RECONSTRUCTIVE SURGERY, April 2000
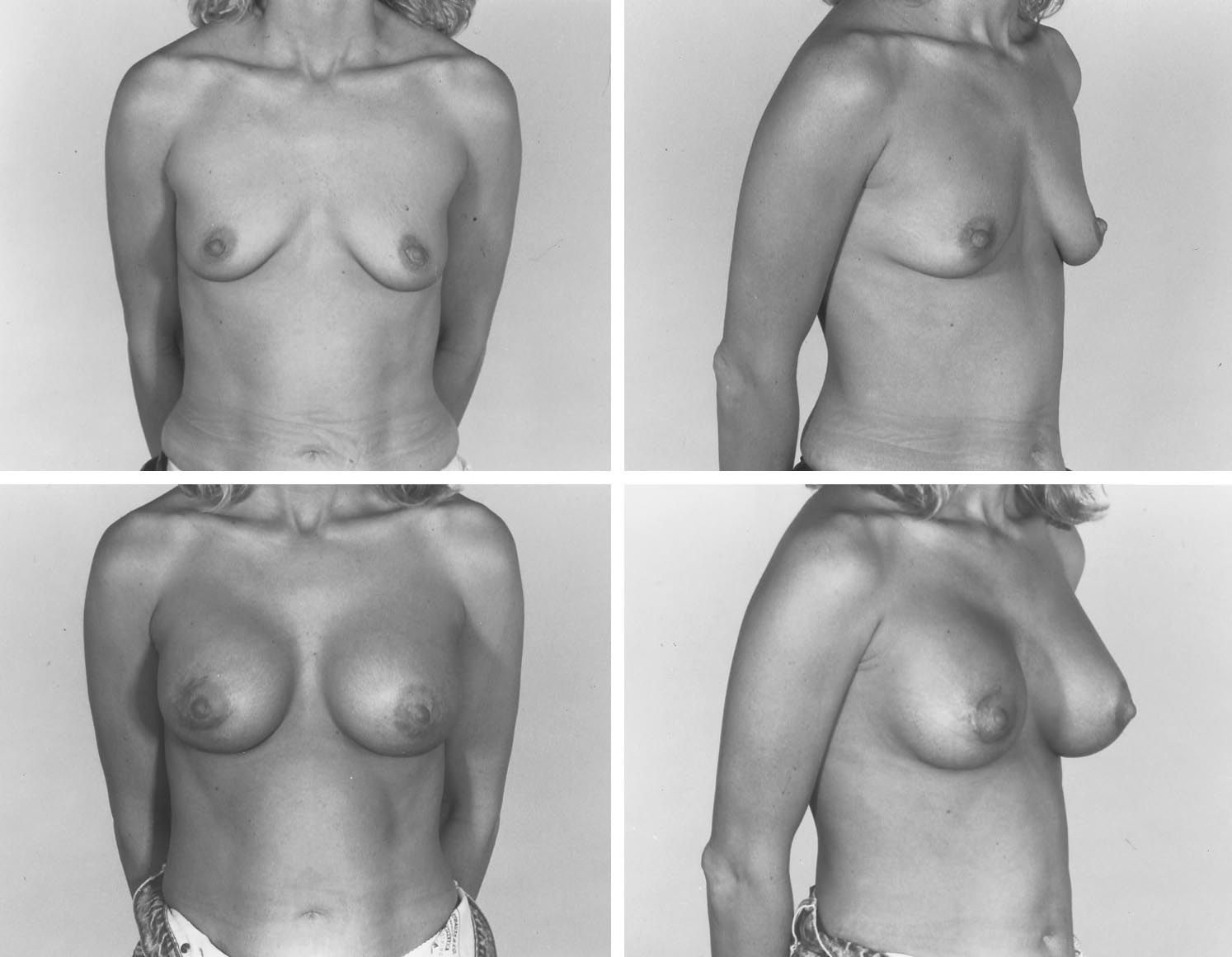
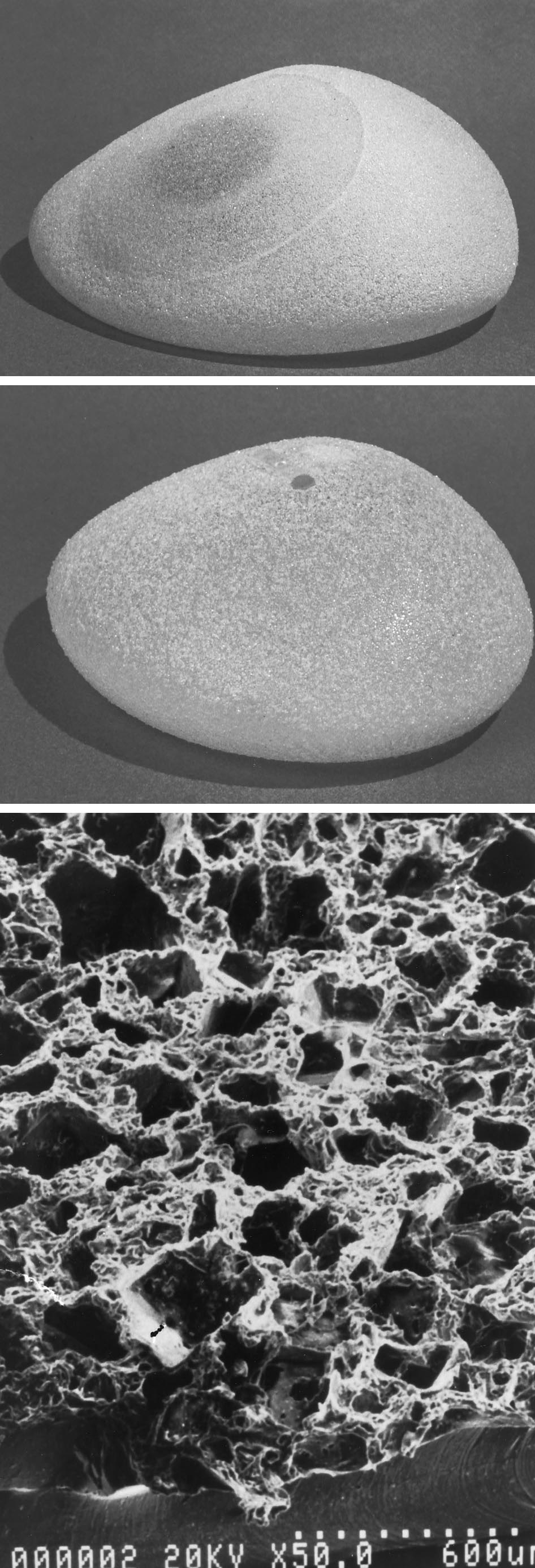
FIG. 2. (Left) The MSI textured surface. (Right) A close-up view of its surface as seen by
The various textured surfaces became avail-
urethane-covered implant from the U.S. mar-
able at approximately the same time and could
ket in 1991 by Bristol Myers, the demand for
be found on silicone gel–filled implants, saline-
other textured-surface breast implants was im-
filled implants, and tissue expanders. Because
mediate. As a result of the FDA hearings of
much of this innovation occurred just before
1991 and 1992 and the contemporaneously ex-
and during the FDA hearings on silicone im-
tremely hostile litigation environment, Dow
plants, there has been only a modest amount of
Corning ceased its breast implant business and
information available regarding how, and how
the MSI surface was simultaneously withdrawn,
well, these textured surfaces work. However,
despite early, quite favorable anecdotal experi-
certain things did become clear. First, each of
ence with it.
the available textured surfaces was manufac-
In the United States, by early 1992, two types
tured differently, looked different, and be-
of textured surfaces were available on tissue
haved differently in the clinical environment.
expanders and saline-filled implants: the Bio-
Second, textured surfaces behaved differently,
cell surface and the Siltex surface. Mentor at
depending on whether they were used on sili-
that time was the only manufacturer approved
cone gel implants, saline implants, or expand-
to market textured-surface, silicone gel–filled
ers. The evidence is convincing that neither
implants in an FDA-approved "adjunct study."
the MSI nor the Siltex textured expanders or
More recently, McGhan has won approval by
implants induced the type of tissue ingrowth as
the FDA for its own adjunct study, which in-
seen with polyurethane. The Biocell expand-
cludes its Biocell textured-surface, silicone gel–
ers, on the other hand, usually incited tissue
filled implants. For practical purposes, we have
ingrowth, whereas the Biocell implants did so
had nearly 10 years of clinical experience with
only occasionally.41 Whereas the MSI and Siltex
two types of textured-surface breast implants.
surfaces were resistant to tissue ingrowth, the
Many surgeons have had their own individual
Biocell surface promoted ingrowth, particu-
experiences with these various devices, and we
larly when native tissues were placed in inti-
now have a handful of reasonable studies on
mate contact with the Biocell surface such as
which to make some judgment.
was seen with tissue expansion or a tight pocket
The stage was initially set in 1981 with re-
around an implant.
ports first by Capozzi and Pennisi, and eventu-
With the voluntary withdrawal of the poly-
ally by many others, that polyurethane-covered,
Vol. 105, No. 4 / AUGMENTATION MAMMAPLASTY
ture rate around those early-design smooth,silicone gel–filled implants and a 20 percentrate around smooth, saline-filled implants.
Some of these patients were radiated, whichhelps explain the high frequency of capsularcontracture in both groups. On a follow-up ofthis same study published 6 years later in 1990,the incidence of capsular contracture at 6 yearsremained stable and was 50 percent in thesilicone gel group and 16 percent in the saline-filled group. The report by Lavine in 1993reviewed 1091 women who had undergonemostly subpectoral breast augmentation by us-ing smooth, saline-filled implants over a 10-year period with an overall capsular contrac-ture rate of 6.1 percent. Thus, even without thebenefit of textured surfacing in these studies,saline-filled implants placed subpectorally hadfairly well proven to have a lower incidence ofcapsular contracture than the early versions ofsmooth-surface, silicone gel–filled implants.
The problems with saline-filled devices, on theother hand, have had more to do with defla-tion, visibility, and palpability.
Much of the impetus for developing a tex-
tured surface, thus, was focused primarily onthe silicone gel–filled implant, for which therewas more of a history of a problem with capsu-lar contracture. Publications by Hakelius andOhlse´n in 1992 and Pollock in 1993 gave earlysupport to a lower capsular contracture ratewith textured-surface, gel implants.19,20 Hake-lius and Ohlse´n performed a 1-year, randomlyassigned, double-blinded study of subglandularbreast augmentations in 25 women by using amore modern design McGhan smooth, siliconegel implant on one side and a McGhan, Bio-cell, textured silicone gel implant on the otherside. The textured silicone gel device per-formed dramatically better, and 12 of the 25women ultimately asked to replace the smoothimplant on one side. Forty-four percent of the
FIG. 3. (Above) The Siltex textured-surface, saline-filled
breast implant. (Below) A close-up of its surface as seen by
smooth, silicone gel–filled implants had capsu-
lar contracture, whereas none of the texturedimplants did.
silicone gel–filled implants produced a dra-
In the publication by Harlan-Pollock in 1993
matic lowering of the capsular contracture rate
reviewing 197 subglandular breast augmenta-
compared with the smooth silicone gel–filled
tions (98 Mentor, smooth, double-lumen sili-
implants available at that time.1,5–7,9–11 During
cone gel and 99 Mentor, Siltex surface, silicone
the same time period, several studies demon-
gel), the smooth implants had a 21 percent
strated that saline-filled implants had a signifi-
incidence of capsular contracture, whereas the
cantly lower rate of capsular contracture than
textured-surface implants had a 4 percent inci-
silicone gel–filled devices.3,4,13,21 Asplund, in a
dence. Coleman's two reviews of his experi-
1984 report on submuscular breast reconstruc-
ence, the first at 1 year and the other after 3
tion, described a 54 percent capsular contrac-
years, confirmed that after subglandular breast
PLASTIC AND RECONSTRUCTIVE SURGERY, April 2000
augmentation, the Mentor Siltex textured sur-face was dramatically effective in reducing cap-sular contracture to 11 percent of patientscompared with 59 percent for smooth Mentorgel-filled implants.
Multicenter data presented on behalf of
both Mentor and McGhan Corporations wouldseem to be in general agreement with theabove studies. The Mentor multicenter "ad-junct" study, composed of more than 1500 in-vestigators and more than 15,000 Siltex tex-tured-surface, silicone gel–filled implants in avariety of clinical situations, has produced acapsular contracture incidence per breast ofroughly 5 percent. The McGhan prospectiveclinical study of silicone gel–filled implantsyielded a similar 5.5 percent textured-surface,implant capsular contracture incidence per im-plant at 4 years. During the same time period,smooth-surface, McGhan gel implants used inbreast augmentation had a 10.6 percent inci-dence per implant of capsular contracture.42 Inboth the McGhan and Mentor studies, the datafor subglandular and submuscular implantshave so far been lumped together, so that noconclusion can be drawn yet from those studieson subpectoral positioning. The above data forMcGhan was reported per implant, and in thecase of breast augmentation, with mostly uni-lateral capsular contracture, the per-patient in-cidence of contracture was 15.8 percent forsmooth gel implants and 9.2 percent for tex-tured gel implants.
The data we have reviewed strongly support
certain conclusions. Polyurethane-covered im-plants were effective at reducing capsular con-tracture compared with a wide variety of earlyversions of smooth, silicone gel–filled devicesavailable in the 1970s and early 1980s. Saline-filled, smooth implants were also somewhateffective at reducing the incidence of capsularcontracture compared with smooth, gel-filleddevices, particularly when placed subpec-torally. And, both the McGhan Biocell texturedsurface and the Mentor Siltex textured surfaceare generally effective in reducing the inci-dence of capsular contracture. Interestingly, todate, there have been no published reportsdirectly comparing the efficacy of the mildlyaggressive Siltex textured surface with themore aggressively textured McGhan Biocellsurface. Several studies have looked at the ben-
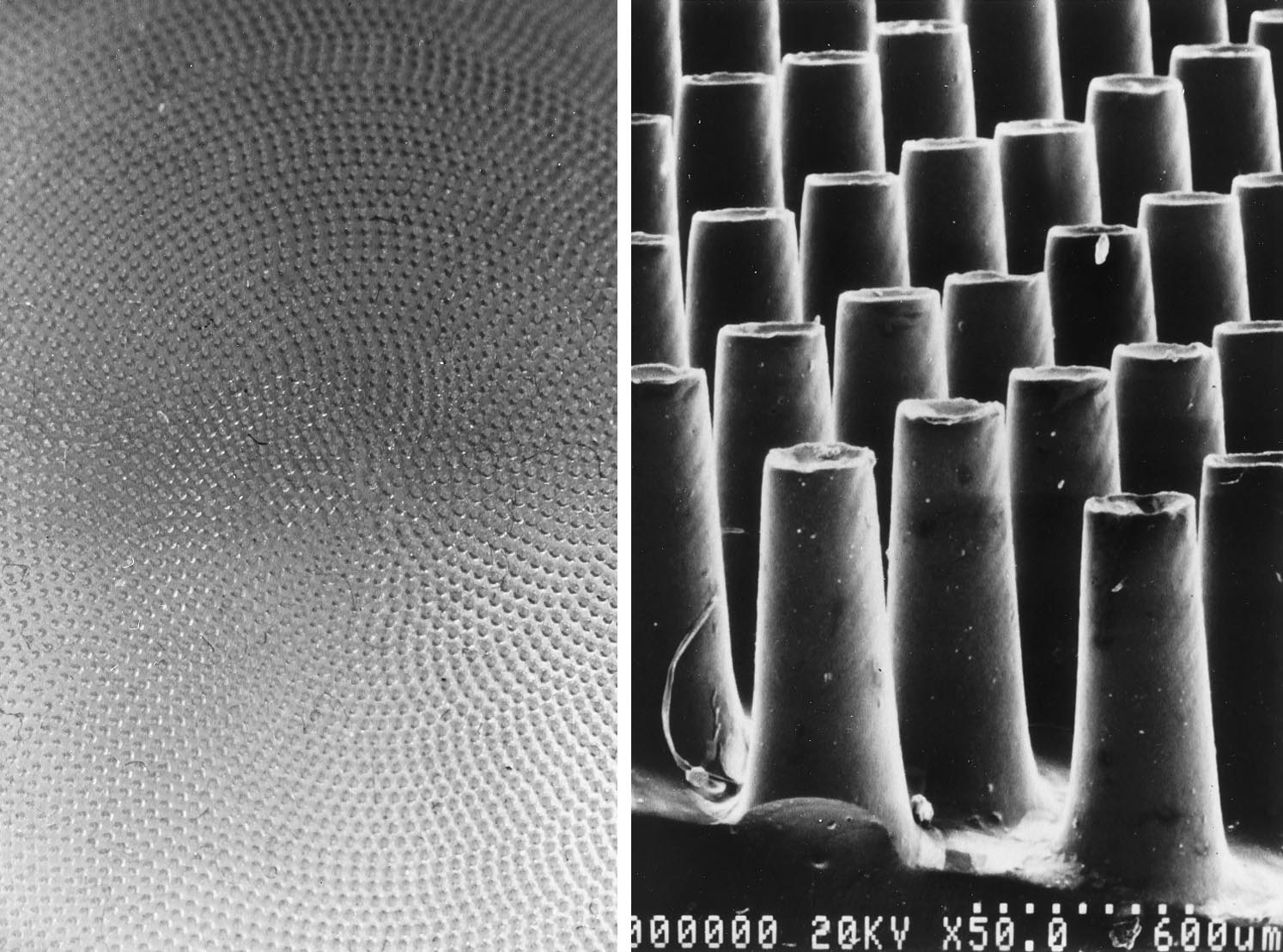
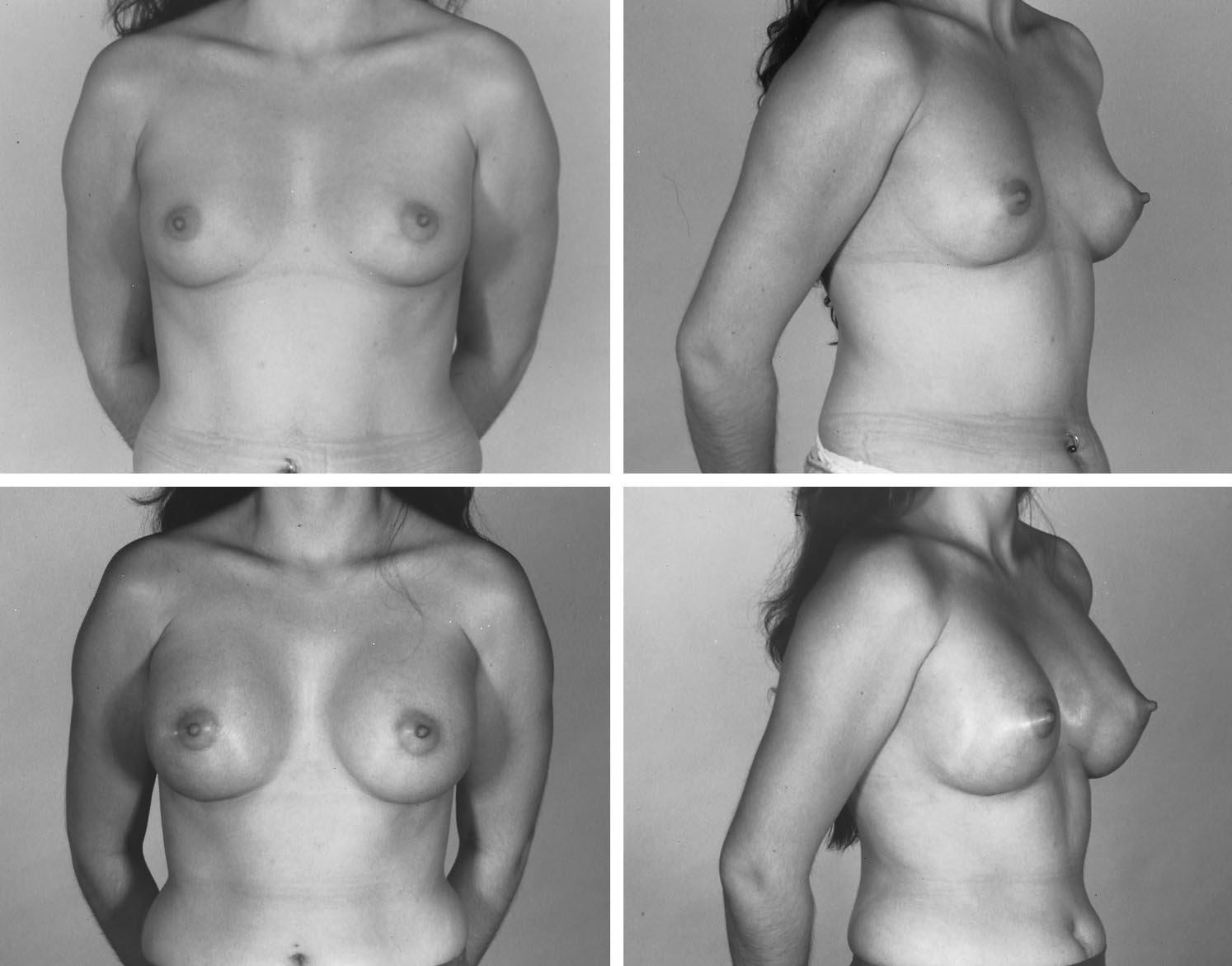
FIG. 4. (Above) The Biocell textured-surface, tissue ex-
efits of submuscular or subpectoral positioning
pander. (Center) The Biocell textured-surface, saline-filledbreast implant. (Below) A close-up of the implant's textured
over subglandular placement, with the evi-
surface as seen by electron microscopy.
dence supporting a reduction in capsular con-
Vol. 105, No. 4 / AUGMENTATION MAMMAPLASTY
tracture with implants under some muscle par-
surgeons could distinguish clinically between
the smooth and textured implants.
Information on the combined benefits of sub-
Tarpila et al. from Sweden performed a sim-
muscular positioning and surface texturing
ilar study in subglandular augmentation in 21
awaits further studies and their publication.
women by using McGhan Biocell and smooth,
The initial work on textured surfaces and
saline-filled implants randomly on opposite
saline-filled devices was in expanders. Max-
sides.35 The implants were overfilled 10 cc, and
well's landmark study on breast reconstruction
antibiotics or antibacterials were not used lo-
with Biocell textured surface, integrated-valve,
cally or systemically. At 1 year, 29 percent of
anatomic tissue expanders dramatically dem-
textured and 38 percent of smooth implants
onstrated the effectiveness of these devices not
exhibited Baker III capsular contractures, a
only in avoiding capsular contracture but in
difference that did not reach statistical signifi-
achieving a satisfactory breast shape.43 How-
ever, there was contradictory information in
Of special interest is the McGhan multi-
both animal models and clinical experience,
center study combining subglandular and sub-
with some authors finding no advantage in
pectoral breast augmentation. At 4 years, the
reducing capsular contracture by using tex-
capsular contracture incidence per patient for
tured surfacing in inflatable devices. Neverthe-
smooth saline-filled implants was 7.4 percent,
less, at least in breast reconstruction, textured-
and 8 percent for textured-surface, saline-filled
surface, integrated valve, inflatable tissue
implants; no significant difference. The inci-
expanders have been accepted by many as pref-
dence of capsular contracture per breast would
erable to smooth devices.42,44
have been roughly half of that, i.e., 3.7 percent
Against this background of information first
and 4 percent, respectively.
on textured surfaces and then on saline-filled
Both Truppmann and Mladick have sepa-
devices, we have additional information specif-
rately reported an incidence of capsular con-
ically on textured-surface, saline-filled im-
tracture near 1 percent in subpectoral aug-
plants. However, before looking at these data,
it is critical to remember that even smooth-
implants.22,28,42 On the basis of these studies
surface, saline-filled implants placed subpec-
and earlier studies on breast reconstruction
torally have a favorable record in terms of cap-
with saline-filled implants, it seems clear, par-
sular contracture.21,22,28 Also, there are two
ticularly for saline-filled devices, that subpec-
benefits of subpectoral positioning with saline-
toral positioning is very protective against cap-
filled implant: decreased capsular contracture
sular contracture. With an incidence of near 1
and decreased implant visibility and palpabil-
percent as reported by Mladick22 and others
ity. In 1994, Burkhardt and Demas reported
around smooth, saline-filled implants for
their experience with Mentor's Siltex textured,
breast augmentation placed subpectorally, it is
saline-filled implant used randomly on one
not clear that surface texturing has much ad-
side of subglandular breast augmentation.23
ditional to offer in avoiding capsular contrac-
The Siltex side had a 2 percent incidence of
ture when submuscular placement is being
capsular contracture compared with 40 per-
considered. Thus, although the benefit of sub-
cent on the opposite side with a smooth im-
muscular positioning of saline-filled implants
plant. Of interest in this study is the preference
in avoiding capsular contracture seems un-
of some of the patients for their firmer smooth
equivocal, the information on surface textur-
inflatable implant over the opposite side's
ing for saline devices is more complicated.
softer textured implant, because the smooth
The published data we have reviewed from
device was less palpable or visible. In 1995,
several different studies suggest then that sub-
Burkhardt and Eades reported on a similar
glandular breast augmentation with smooth,
study comparing McGhan's Biocell textured-
saline-filled implants may yield a capsular con-
surface, saline-filled implant to its smooth
tracture incidence per implant of between 23
counterpart again in subglandular breast aug-
and 40 percent. Surface texturing has the po-
mentation.29 Thirteen percent of textured de-
tential to reduce that incidence to somewhere
vices exhibited Baker class III or IV capsular
between 2 and 29 percent. However, the Siltex
contracture compared with 23 percent of
textured saline-filled implant may have the dis-
smooth devices. Unlike the Mentor textured-
advantage of being more palpable and visible
surface implants, neither the patients or the
than its smooth counterpart, to some extent
PLASTIC AND RECONSTRUCTIVE SURGERY, April 2000
possibly negating its advantage of less capsular
plants in subpectoral breast augmentation. In
contracture in the subglandular position. The
most patients, they did fine in terms of capsular
McGhan Biocell textured surface also seems
contracture (Fig. 5). Although we initially used
effective at reducing the incidence of subglan-
them with a dilute intraluminal solution of
dular capsular contracture, but the McGhan
Solu-medrol, we stopped that practice because
Biocell saline-filled implant also may be more
of the evidence and our own experience that
visible and palpable, than a smooth implant.
submuscular saline-filled implants do not need
Although there is no evidence that the Mentor
the help of steroids. Our experience with sub-
Siltex textured, saline-filled implants experi-
glandular, saline-filled implants has not been
ence tissue ingrowth, the McGhan Biocell sa-
quite as favorable. Both in primary and second-
line implant will achieve ingrowth in some pa-
ary cases of subglandular breast augmentation,
tients. The tighter the pocket and the more
some smooth and some textured saline-filled
pressure exerted by the implant against sur-
implants have been more palpable and more
rounding native tissues, the more likely in-
visible than subpectoral implants. And, it is our
growth will occur. However, it is not clear that
impression that there have been more capsular
tissue ingrowth around implants is necessarily
contractures, although we have not studied
desirable, although many if not most surgeons
these patients carefully enough yet to quanti-
prefer tissue ingrowth around expanders.
tate the difference. And when the implants are
Of course, there is more to breast surgery
placed subpectorally, there is the important
than just capsular contracture. What about
added advantage of improved mammography.
shape, appearance, feel, and mammography?
Based on the published studies and our own
My personal experience with saline-filled im-
clinical experience, we make these recommen-
plants began in the late 1980s when I substi-
dations. For reasons of softness, shape, feel,
tuted smooth saline implants occasionally for
appearance, and mammography, saline-filled
smooth double-lumen silicone gel–filled im-
implants do best when placed beneath all or
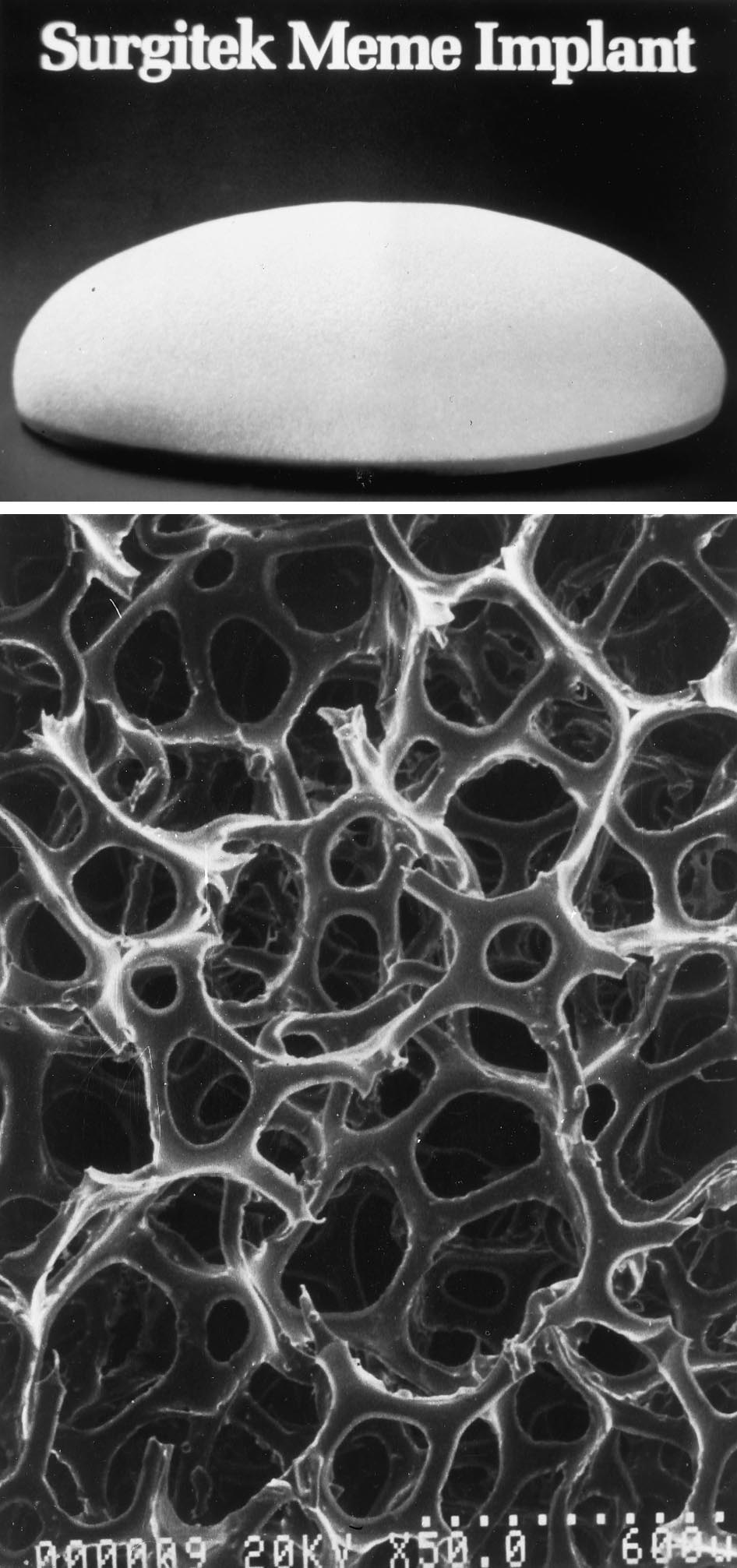
FIG. 5. A patient before (above) and after (below) subpectoral augmentation mammaplasty
using 360-cc round, smooth-surface, saline-filled breast implants. A patient with healthy andsufficient soft-tissue coverage such as this would also be an appropriate candidate for a sub-glandular breast implant for which surface texturing would provide added protection againstcapsular contracture without undue risk of undesirable palpability or visibility. The subpectoralapproach is still preferable in terms of mammography.
Vol. 105, No. 4 / AUGMENTATION MAMMAPLASTY
some portion of the pectoralis major muscle.
contracture, mammography, and implant pal-
In very thin and small-breasted women without
pability, this is better done subpectorally; it can
ptosis, even more or total muscle cover is an
also be done in the subglandular space in pa-
option. This finding is particularly true for sa-
tients with adequate soft tissue. Because of the
line-filled implants, even more so than for gel-
very low risk of capsular contracture around
filled implants because of possible palpability,
subpectoral, smooth-surface, round saline-
visibility, and rippling problems from saline.
filled implants, there would seem to be little
On the other hand, subglandular placement is
advantage in the use of round, textured-
a more reasonable option in patients with
surface, saline-filled implants in the subpec-
some breast tissue and subcutaneous fat, and a
toral position, except for reasons of personal
healthy, reasonably thick, elastic youthful skin
preference or perhaps in a patient who has a
envelope. The healthier the soft-tissue cover,
poor record with capsular contracture associ-
the better subglandular saline-filled implants
ated with an earlier smooth round device.
perform and feel. Published reviews support
Technically, breast augmentation with
the proposition that textured-surface implants
smooth, round saline-filled implants resembles
offer some special advantage in these patients
historical techniques with silicone gel implants,
for reducing capsular contracture when the
for which implant mobility and large pocket
implant is placed subglandularly (Table I).
dissection were desirable. With this large-
The ptotic patient with stretched out and thin
pocket approach by using saline-filled im-
skin is problematic. Although subpectoral po-
plants, particularly larger ones, there may be a
sitioning risks creating a double-bubble with
tendency for increased soft-tissue stretching
the breast hanging below the implant, subglan-
and thinning as a possible result of the repeti-
dular positioning with a textured saline-filled
tive water-hammer effect of the salt water. Al-
implant placed just beneath thinned-out breast
though also possible with silicone gel–filled
skin runs the risk of visible rippling and an
implants, particularly textured ones, this effect
implant that is too easily palpated. The same
was not commonly seen with them. Such soft-
may be true for the patient who has had pre-
tissue stretching would likely increase the risk
vious breast implants, for whom those implants
of rippling, palpability, and ptosis.
may have thinned or stretched out the soft
The textured-surface, saline-filled implants
tissues (Table II). In these difficult situations,
are designed to retain softness without the
repair of the soft tissues by using mastopexy or
need for the mobility seen with smooth ones.
flap techniques may be necessary to use a sa-
In breast augmentation with the McGhan Bio-
cell textured-surface implant, where tissue in-
However, surface texturing may also play a
growth or some adherence is a real possibility,
role when trying to control breast shape (Fig.
precise pocket dissection and conservative im-
6). The various designs of anatomic, saline-
plant volumes (volumes of 380 cc or less) can
filled implants come with textured surfaces.
yield breasts with minimal implant mobility,
Although not proven, it is believed by some
palpability, rippling or ptosis, yet with reason-
that these textured surfaces along with careful
able softness and an attractive, more natural
surgical dissection and appropriate postopera-
shape. However, the drawback of this approach
tive care may help to reduce implant rotation
is a certain lack of mobility, a solution that
and mobility so as to create and best control
some surgeons and patients do not accept. The
breast shape. Although for reasons of capsular
Mentor Siltex surface, although effective at re-
Capsular Contracture around Silicone Gel-Filled Implants
Cap. Contr. around
Cap. Contr. around
around Subgland.
around Subgland.
Textured Gel (site
not specific) (%)
not specific) (%)
Mentor Adj. Clin.
McGhan Core Clin.
Cap. Contr., capsular contracture; Subgland., subglandular; n/a, not applicable; Adj. Clin., adjunct clinical trial; Core Clin., core clinical trial.
PLASTIC AND RECONSTRUCTIVE SURGERY, April 2000
Capsular Contracture around Saline-Filled Implants
Cap. Contr. around
Cap. Contr. around
Textured Gel (site not
McGhan Core Clinical Study
Cap. Contr., capsular contracture.
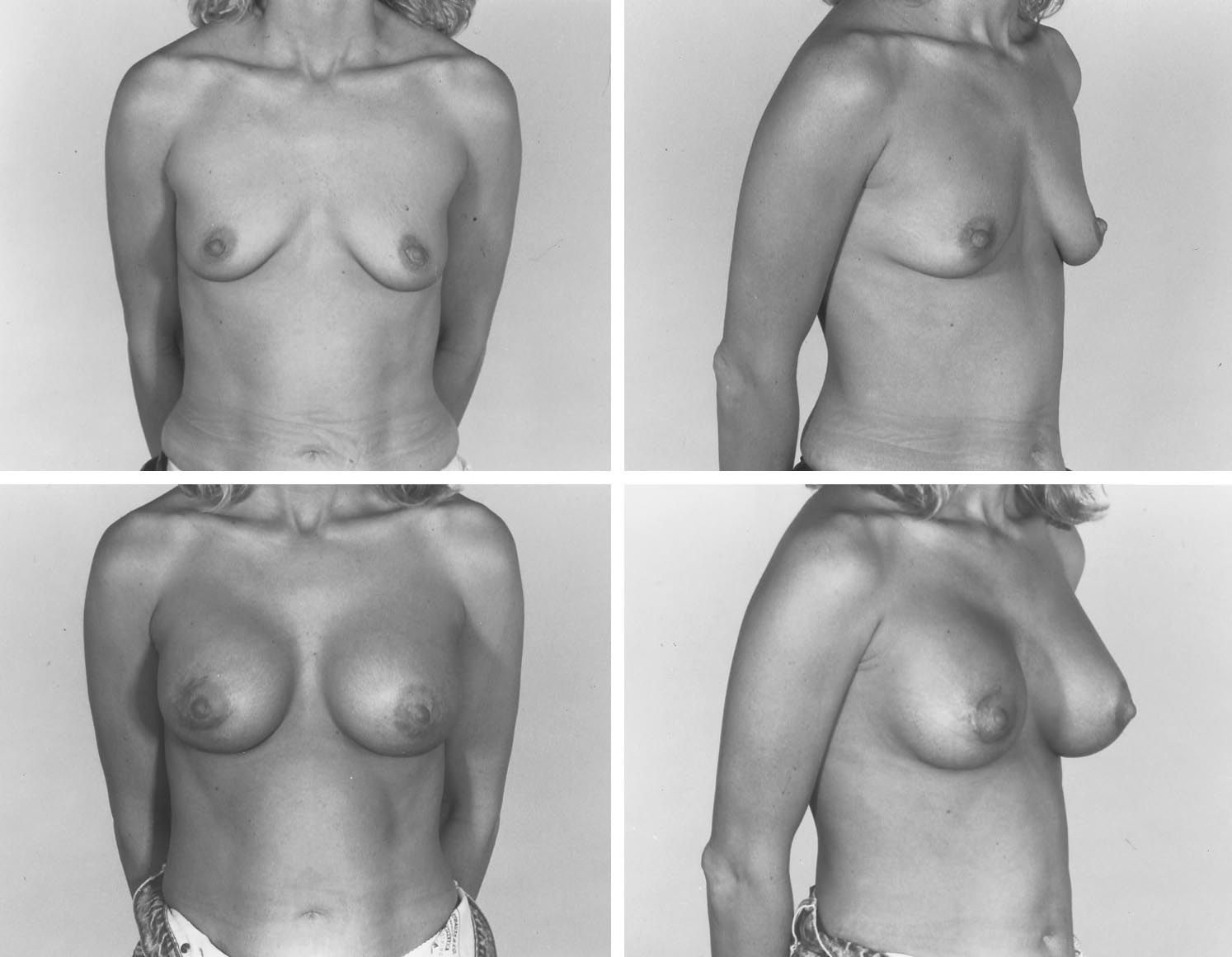
FIG. 6. A patient (above) before and (below) after subpectoral augmentation mammaplasty
using 300-cc anatomic, textured-surface, saline-filled breast implants. A patient with this muchsoft tissue might also be a reasonable candidate for a subglandular, textured, anatomic implantwith precise pocket dissection.
ducing capsular contracture, does so without
has been the historical bug-bear associated
tissue ingrowth or adherence. Clinically, the
with the efficacy of silicone gel–filled breast
technique and results with the Mentor Siltex
implants, palpability, visibility, and rippling as
surface more closely resemble those with un-
well as capsular contracture have been the
encapsulated smooth implants for which mo-
problems with saline-filled ones. Surface tex-
bility rather than adherence is the rule. When
turing has, thus, played a more important role
the Biocell surface is used in secondary cases or
in silicone gel–filled implants than in saline-
after large pocket dissections, tissue ingrowth
filled ones. Textured, saline-filled breast im-
and adherence are also less likely, and in those
plants make the most sense in two scenarios:
circumstances too, mobility rather adherence
first, with anatomic designs where the goal is to
is the rule. For that reason, anatomically
better control and create a certain breast
shaped textured implants are best used only
shape; and second, in patients with adequate
when there is some control over the pocket
soft tissue for whom subglandular positioning
size, shape, and fit to the implant; otherwise,
is desired for whatever reason. For routine sub-
the implant will lose its proper orientation.
pectoral breast augmentation, there are not, at
In conclusion, whereas capsular contracture
the present time any clear documented advan-
Vol. 105, No. 4 / AUGMENTATION MAMMAPLASTY
tages or for that matter disadvantages to round
14. Ersek, R. A.
Rate and incidence of capsular contracture:
textured, saline-filled implants. Subpectoral
A comparison of smooth and textured silicone double-lumen breast prostheses. Plast. Reconstr. Surg. 87: 879,
positioning of saline-filled implants alone
seems very effective at reducing the incidence
15. Coleman, D. J., Foo, I. T. H., and Sharpe, D. T.
of capsular contracture without the added risk
tured or smooth implants for breast augmentation? A
of increased palpability and implant visibility,
prospective controlled trial. Br. J. Plast. Surg. 44: 444,
which may occur in subglandular positioning
16. Handel, N., Silverstein, M. J., Jensen, A., et al.
of textured saline-filled implants particularly in
parative experience with smooth and polyurethane
patients with inadequate soft-tissue cover.
breast implants using the Kaplan-Meire method of
Scott L. Spear, M.D.
survival analysis. Plast. Reconstr. Surg. 88: 475, 1991.
Division of Plastic Surgery
17. Bern, S., Burd, A., and May, J. W., Jr.
Georgetown University Medical Center
and histologic properties of capsules formed bysmooth and textured silicone implants in the rabbit.
3800 Reservoir Road, N.W.
Plast. Reconstr. Surg. 89: 1037, 1992.
Washington, D.C. 20007
18. Barone, F. E., Perry, L., Keller, T., and Maxwell, G. P.
The biomechanical and histopathologic effects of sur-face texturing with silicone and polyurethane in tissue
implantation and expansion. Plast. Reconstr. Surg. 90:77, 1992.
Special thanks to Dennis Hammond, M.D., George Picha,
19. Hakelius, L., and Ohlse´n, L.
A clinical comparison of
M.D., and the Mentor and McGhan Medical Corporations for
the tendency to capsular contracture between smooth
providing some of the illustrations and data for this review.
and textured gel-filled silicone mammary implants.
Plast. Reconstr. Surg. 90: 247, 1992.
20. Pollock, H.
Breast capsular contracture: A retrospective
1. Capozzi, A., and Pennisi, V. R.
Clinical experience with
study of textured versus smooth silicone implants.
polyurethane-covered gel-filled mammary prostheses.
Plast. Reconstr. Surg. 91: 404, 1993.
Plast. Reconstr. Surg. 68: 512, 1981.
21. Lavine, D. M.
Saline inflatable prostheses: 14 years' ex-
2. Mahler, D., and Hauben, D. J.
Retromammary versus
perience. Aesthetic Plast. Surg. 17: 325, 1993.
retropectoral breast augmentation: A comparative
22. Mladick, R. A.
"No-touch" submuscular saline breast
study. Ann. Plast. Surg. 8: 370, 1982.
augmentation technique. Aesthetic Plast. Surg. 17: 183,
3. McKinney, P., and Tresley, G.
Long-term comparison of
patients with gel and saline mammary implants. Plast.
23. Burkhardt, B. R., and Demas, C. P.
The effect of Siltex
Reconstr. Surg. 72: 27, 1983.
texturing and povidone-iodine irrigation on capsular
4. Asplund, O.
Capsular contracture in silicone gel and
contracture around saline inflatable breast implants.
saline-filled breast implants after reconstruction. Plast.
Plast. Reconstr. Surg. 93: 123, 1994.
Reconstr. Surg. 73: 270, 1984.
24. Cocke, W. M., Jr.
A critical review of augmentation
5. Schatten, W. E.
Reconstruction of breasts following
mammoplasty with saline-filled prostheses. Ann. Plast.
mastectomy with polyurethane-covered, gel-filled
Surg. 32: 266, 1994.
prostheses. Ann. Plast. Surg. 12: 147, 1984.
25. May, J. W., Jr., Bucky, L. P., Sohoni, S., and Ehrlich, H. P.
6. Eyssen, J. E., von Werssowetz, A. J., and Middleton, G. D.
Smooth versus textured expander implants: A double-
Reconstruction of the breast using polyurethane-
blind study of capsule quality and discomfort in si-
coated prostheses. Plast. Reconstr. Surg. 73: 415, 1984.
multaneous bilateral breast reconstruction patients.
7. Herman, S.
The Meˆme implant. Plast. Reconstr. Surg. 73:
Ann. Plast. Surg. 32: 225, 1994.
26. Bucky, L. P., Ehrlich, H. P., Sohoni, S., and May, J. W.
8. Puckett, C. L., Croll, G. H., Reichel, C. A., and Concan-
The capsule quality of saline-filled smooth silicone,
A critical look at capsule contracture in
textured silicone, and polyurethane implants in rab-
subglandular versus subpectoral mammary augmen-
bits: A long-term study. Plast. Reconstr. Surg. 93: 1123,
tation. Aesthetic Plast. Surg. 11: 23, 1987.
9. Melmed, E. P.
Polyurethane implants: A 6-year review of
27. Worseg, A., Kuzbari, R., Tairych, G., et al.
416 patients. Plast. Reconstr. Surg. 82: 285, 1988.
results of inflatable mammary implants. Br. J. Plast.
10. Hester, T. R., Jr., Nahai, F., Bostwick, J., and Cukic, J.
Surg. 48: 183, 1995.
5-year experience with polyurethane-covered mam-
28. Mladick, R. A.
Inflatable breast implants. Plast. Reconstr.
mary prostheses for treatment of capsular contrac-
Surg. 95: 600, 1995.
ture, primary augmentation mammoplasty, and breast
29. Burkhardt, B. R., and Eades, E.
The effect of Biocell
reconstruction. Clin. Plast. Surg. 15: 569, 1988.
texturing and povidone-iodine irrigation on capsular
11. Pennisi, V. R.
Long-term use of polyurethane breast
contracture around saline-inflatable breast implants.
prostheses: A 14-year experience. Plast. Reconstr. Surg.
Plast. Reconstr. Surg. 96: 1317, 1995.
86: 368, 1990.
30. Sinclair, T. M., Kerrigan, C. L., and Sampalis, J.
12. Caffee, H. H.
Textured silicone and capsule contrac-
degradation of polyurethane foam, revisited, in the rat
ture. Ann. Plast. Surg. 24: 197, 1990.
model. Plast. Reconstr. Surg. 96: 1326, 1995.
13. Gylbert, L., Asplund, O., and Jurell, G.
31. Asplund, O., Gylbert, L., Jurell, G., and Ward, C.
tracture after breast reconstruction with silicone-gel
tured or smooth implants for submuscular breast aug-
and saline-filled implants: A 6-year follow-up. Plast.
mentation: a controlled study. Plast. Reconstr. Surg. 97:
Reconstr. Surg. 85: 373, 1990.
PLASTIC AND RECONSTRUCTIVE SURGERY, April 2000
32. Rohrich, R. J., Beran, S. J., Ingram., A. E., and Young, V. L.
cone mammary implants: A 5-year follow-up. Plast.
Development of alternative breast implant filler ma-
Reconstr. Surg. 100: 1566, 1997.
terial: Criteria and horizons. Plast. Reconstr. Surg. 98:
38. Ersek, R. A., and Salisbury, A. V.
Textured surface, non-
silicone gel breast implants: Four years' clinical out-
33. Malata, C. M., Feldberg, L., Coleman, D. J., et al.
come. Plast. Reconstr. Surg. 100: 1729, 1997.
tured or smooth implants for breast augmentation?
39. Copeland, M., Choi, M., and Bleiweiss, I.
Three-year follow-up of a prospective randomised
down and capsular synovial metaplasia in textured-
controlled trial. Br. J. Plast. Surg. 50: 99, 1997.
wall saline breast prosthesis. Plast. Reconstr. Surg. 94:
34. Wickman, M., and Jurell, G.
Low capsular contraction
rate after primary and secondary breast reconstruc-
40. Batch, C., Williams, J., and King, R.
tion with a textured expander prostheses. Plast. Re-
products from a biodegradable foam implant.
constr. Surg. 99: 692, 1997.
J. Biomed. Mater. Res. Appl. Biomat. 23: 311, 1989.
35. Tarpila, E., Ghassemifar, R., Fagrell, D., and Berggren, A.
41. Mentor Corporation.
Capsular contracture with textured versus smooth sa-
42. Maxwell, G. P., and Falcone, P. A.
Eighty-four consec-
line-filled implants for breast augmentation: A pro-
utive breast reconstructions using a textured silicone
spective clinical study. Plast. Reconstr. Surg. 99: 1934,
tissue expander. Plast. Reconstr. Surg. 89: 1022, 1992.
43. McGhan Medical Study Corporation.
36. Gutowski, K. A., Mesna, G. T., and Cunningham, B. L.
Saline-filled breast implants: A Plastic Surgery Educa-
44. Spear, S. L., and Majidian, A.
Immediate breast recon-
tional Foundation multicenter outcomes study. Plast.
struction in two stages using textured, integrated valve
Reconstr. Surg. 100: 1019, 1997.
tissue expanders and breast implants: A retrospective
37. Hakelius, L., and Ohlse´n, L.
Tendency to capsular con-
review of 171 breast reconstructions from 1989 to
tracture around smooth and textured gel-filled sili-
1996. Plast. Reconstr. Surg. 101: 53, 1998.
Source: http://www.silimedespana.es/wp-content/uploads/2013/12/artigo_4.pdf
BEVACIZUMAB IN EYE CONDITIONS: ISSUES RELATED TO QUALITY, USE, EFFICACY AND SAFETY REPORT BY THE DECISION SUPPORT UNIT Edith Poku, John Rathbone, Emma Everson-Hock, Munira Essat, Ruth Wong, Abdullah Pandor, Allan Wailoo School of Health and Related Research, University of Sheffield Decision Support Unit, ScHARR, University of Sheffield, Regent Court, 30 Regent Street
Russischer Militärexperte: H1N1-Grippe soll Überschuß. Russischer Militärexperte: H1N1-Grippe soll Überschuß an Menschen beseitigen In Abwesenheit von Rumpelstilz füllt das autarke „Leerer-Kollektiv"zwischenzeitlich die Leere ein wenig. Samstag, den 29. Mai 2009 geg. 21 Uhr ERINNERUNG AN EINEN IMMER NOCH NICHT AUFGEKLÄRTEN TODESFALL DERBRD-DIKTATUR 2004!