Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Quintessenz journals

RANDOMISED CONTROLLED CLINICAL TRIAL
Marco Esposito, Carlo Barausse, Roberto Pistilli, Vittorio Checchi, Michele Diazzi, Maria Rosaria Gatto, Pietro Felice
Posterior jaws rehabilitated with partial prostheses
supported by 4.0 x 4.0 mm or by longer implants:
Four-month post-loading data from a randomised
Marco Esposito, DDS,
PhD
Freelance researcher and
Associated Professor,
Department of Biomaterials,
Key words
posterior jaws, short dental implants
The Sahlgrenska Academy at Göteborg University, Göteborg, Sweden
Purpose: To evaluate whether 4.0 x 4.0 mm dental implants could be an alternative to implants at
least 8.5 mm long, which were placed in posterior jaws in the presence of adequate bone volumes.
Carlo Barausse, DDS
Resident, Department of
Materials and methods: One hundred and fifty patients with posterior (premolar and molar areas)
Biomedical and Neuromotor
mandibles having at least 12.5 mm bone height above the mandibular canal or 11.5 mm bone height
Sciences, Unit of Peri-odontology and Implantol-
below the maxillary sinus, were randomised according to a parallel group design, in order to receive
ogy, University of Bologna, Bologna, Italy
one to three 4.0 mm-long implants or one to three implants which were at least 8.5 mm long, at three centres. All implants had a diameter of 4.0 mm. Implants were loaded after 4 months with de-
Roberto Pistilli, MD
Resident, Oral and Maxillo-
finitive screw-retained prostheses. Patients were followed up to 4-month post-loading and outcome
facial Unit, San Filippo Neri
measures were prosthesis and implant failures, any complications and peri-implant marginal bone
Hospital, Rome, Italy
Vittorio Checchi,
Results: No patients dropped-out before the 4-month evaluation. Three patients experienced the
DDS, PhD
Researcher, Department of
early failures of one 4.0 mm-long implant each, in comparison to two patients who lost one long
Medical Sciences, University
implant each (difference in proportion = 0.01; 95% CI -0.06 to 0.09; P = 0.50). Consequently, two
of Trieste, Trieste, Italy
prostheses in each group could not be delivered as planned (difference in proportion = 0; 95% CI
Michele Diazzi, DDS
Private practice in Bologna,
-0.07 to 0.07; P = 0.69), and one patient from each group is still waiting to have their prostheses
delivered. Three short implant patients experienced three complications versus two long implant
Maria Rosaria Gatto,
patients (difference in proportion = 0.01; 95% CI -0.06 to 0.09; P = 0.50). There were no statistically
significant differences in prosthesis failures, implant failures and complications. Patients with short
Researcher, Department of Biomedical and Neuromotor
implants lost on average 0.38 mm of peri-implant bone at 4 months and patients with long man-
Sciences, Unit of Peri-
dibular implants lost 0.42 mm. There were no statistically significant differences in bone level changes
odontology and Implantol-ogy, University of Bologna,
up to 4 months between short and long implants (mean difference = 0.04 mm; 95% CI: -0.041 to
0.117; P = 0.274).
Pietro Felice, MD,
Conclusions: Four months after loading, 4.0 x 4.0 mm implants achieved similar results as
DDS, PhD
Researcher, Department of
8.5 x 4.0 mm-long or longer implants in posterior jaws, however 5 to 10 years post-loading data are
Biomedical and Neuromotor
necessary before reliable recommendations can be made.
Sciences, Unit of Peri-odontology and Implantol-ogy, University of Bologna,
Conflict-of-interest statement: Global D (Lyon, France) donated implants and prosthetic components
and Tecnoss (Coazze, Italy) donated the biomaterials used in this study. Data property belonged to the
Correspondance to:
authors and by no means did the manufacturers interfere with the conduct of the trial or the publica-
Dr Marco Esposito, Casella Postale 34,
tion of its results.
20862 Arcore (MB), Italy Email: [email protected]
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
ing the quality of reports of parallel group randomised
Short dental implants are used as an alternative to long implants in intentionally augmented bone, in order to support fixed prostheses in the rehabili-
Materials and methods
tation of patients with atrophic jaws. There are a few randomised controlled trials (RCTs) comparing This study was designed according to a randomised the effectiveness of dental prostheses supported controlled multicenter trial of parallel group design by short implants with those supported by long with two arms, using, whenever possible, a blinded implants placed in augmented bone1-12. The results outcome assessor.
of these ongoing trials having follow-ups of up to
Any partially edentulous patient missing teeth
5-years post-loading, suggest that 5.0 to 8.0 mm-
in the premolar and molar area requiring one to
long implants can be a viable, if not a better, alterna-
three dental implants, being 18 years or older, and
tive to augmentation procedures, especially in pos-
able to sign an informed consent form was eligible
terior mandibles.
for inclusion in this trial. Vertical bone heights at
More recent clinical questions include whether implant sites had to be at least 12.5 mm above the
to use short implants also in those situations were mandibular canals and 11.5 mm below the maxillary long implants could have been used and how short sinuses. Bone thickness had to be at least 6.0 mm could an implant be in order to be able to provide as measured on cone beam computer tomography a good long-term outcome. There are at least two (CT) scans. Each patient was treated at only one manufacturers (Straumann and Global D) market-
side of the jaw and received one prosthesis only,
ing transmucosal 4.0 mm-long implants, and one according to a parallel group design. Exclusion cri-of these implant types was evaluated in a multicen-
tre non-controlled single-cohort prospective 2-year • general contraindications to implant surgery;post-loading study13. In this study 100 4.0 mm-long • subjected to irradiation in the head and neck area;implants were placed in the posterior region of 32 • immunosuppressed or immunocompromised;partially edentulous patients (three or four implants • treated or under treatment with intravenous in each patient). Seven implants failed before loading
in 4 patients and 2 additional patients were excluded • untreated periodontitis;for unclear reasons (most likely because of implant • poor oral hygiene and motivation;failures) so that only 26 patients received their pros-
• uncontrolled diabetes;
theses. Two years after loading one patient died and • pregnant or nursing;one requested to have all his implants removed13. • substance abusers;This means that the treatment with short implants • psychiatric problems or unrealistic expectations;failed in 23% (seven out of 31) of the treated patients • lack of opposite occluding dentition to the area 2 years after loading, and these initial figures are not
intended for implant placement;
very promising.
• acute or chronic infection/inflammation in the
The aim of this RCT was to compare the outcome
area intended for implant placement;
of partial fixed prostheses supported by 4.0 x 4.0 mm • participation in other trials, if the present protocol implants with prostheses supported by implants at
could not be properly followed;
least 8.5 x 4.0 mm long placed in posterior jaws, • referred only for implant placement and not hav-which have adequate bone volumes to be treated
ing the prosthesis or maintenance procedures
with medium to long implants. This report presents
performed at the treatment centres;
the preliminary clinical outcome up to 4-month post-
• unable to attend follow-up visits for 3 years after
loading. The aim was to follow-up these patients
to the third year of function. The present article is • post-extractive sockets if the upper portion of reported according to the CONSORT (Consolidated
the buccal wall was lower than 4 mm when com-
Standards of Reporting Trials) statement for improv-
pared to the palatal wall.
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
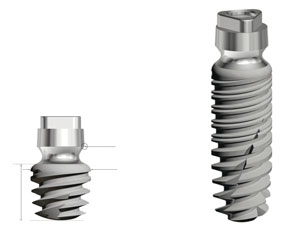
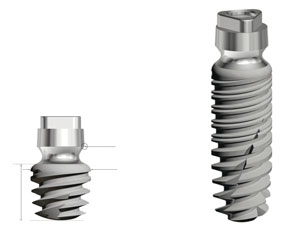
reference point for x-ray measurement
Fig 1 Illustration of 4.0 mm (a) and 13.0 mm (b) conical
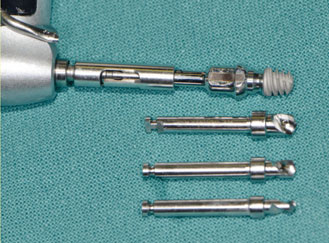
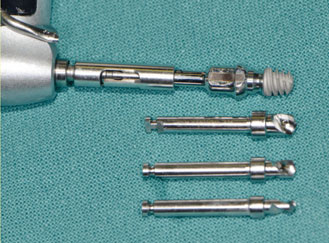
Fig 2 Sequence of drills used to prepare the implant sites
transmucosal Global D TwinKon® Universal SA2 implants
for shorter implants. Please notice the presence of stops
used in this study. Implants are made of Ti4V6Al alloy, have
with the drills.
a sand-blasted acid-etched surface and a peculiar external connection.
Patients were categorised into three groups for 1 min with 0.2% chlorhexidine. The area was
according to what they declared: non-smoker, mod-
locally anaesthetised with infiltration of articain with
erate smoker (up to 10 cigarettes per day) and heavy adrenaline 1:100.000. After crestal incision and flap smoker (more than 10 cigarettes per day). Patients elevation, or in the case of post-extractive implants were to be recruited and treated in three different after curettage of the socket, patients were randomly centres (50 patients per centre) by three different allocated, by opening the sequentially numbered operators, however one operator recruited and envelope corresponding to the patient recruitment treated only four patients, so his remaining quota number, where either they received one to three of patients were taken by one of the two remaining 4.0 x 4.0 mm long implants (Fig 1a) or one to three operators (Dr Pietro Felice), who treated patients in implants which were at least 8.5 mm long (8.5, 10.0, two Italian private practices and one university hos-
11.5 and 13.0 mm-long; Fig 1b) and 4.0 mm in diam-
pital, whereas the other operator (Dr Roberto Pis-
eter, according to the standard procedures as recom-
tilli) treated patients both in a hospital and a private mended by the manufacturer (TwinKon® Universal practice. All operators followed similar standardised SA2, Global D, Lyon, France). Surgical stents were procedures.
used to optimise implant positioning after flap eleva-
The principles outlined in the Declaration of tion. Drills with stops and increasing diameters were
Helsinki on clinical research involving human sub-
used to prepare the implant sites, which were slightly
jects were adhered to. The study was approved by underprepared (Fig 2). At implant insertion, the sur-the ethical committee of the Ospedale Maggiore in gical motor unit was set at a torque of 25 Ncm and Bologna, Italy on 14 June 2013 (Prot.N.554/CE). All resistance at implant insertion was recorded as < 25 patients received thorough explanations and signed Ncm or > 25 Ncm. The transition portion from the a written informed consent form prior to being machined to the roughened surface of the implant enrolled in the trial. Approximately 10 days before neck (Fig 1) was placed about 2 mm subcrestally. In the implant placement patients received at least one ses-
case of post-extractive implants, teeth were extracted
sion of professional oral hygiene.
using the flapless approach, in order to try to minimise the surgical trauma as much as possible and to spare the buccal wall of the socket. Sockets were carefully
Implant placement procedures
debrided from any remnants of granulation tissue.
Two grams of amoxicillin (or 100 mg minocycline In the presence of a horizontal buccal bone to im-for patients allergic to penicillin) were administered plant gap of 2 mm or more, gaps were filled with 600 1 h prior to implant placement and patients rinsed to 1000 microns diameter granules of pre-hydrated
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
cortico-cancellous porcine bone mixed with approxi-
Patients were enrolled in an oral hygiene pro-
mately 10% collagen gel (MP3, OsteoBiol, Tecnoss, gram with recall visits every 6 months for the entire Coazze, Italy) covered with a haemostatic resorbable duration of the study. Follow-ups were conducted by collagen sponge (Spongostan, 1 x 1 x 1 cm, Ethicon, independent outcome assessors (Dr Vittorio Checchi Johnson & Johnson, New Jersey, USA) of porcine ori-
at Dr Pietro Felice's and Luigi Checchi's centres and
gin, blocked with a cross-suture.
Dr Roberto Cassoni at Dr Roberto Pistilli's centre).
Healing abutments were placed on implants not
to be submerged, and healing screws on implants to
Outcome measures
be submerged and flaps were closed around non-submerged implants or over submerged implants with This study tested the null hypothesis that there were vicryl 4/0 sutures (Ethicon). The decision on whether no differences in the clinical outcomes between the to submerge the implant or not was based on the two procedures against the alternative hypothesis of thickness of the mucosa. Ideally all implants were to be a difference. Outcome measures were:submerged, however since these implants had a trans-
• Prosthesis failure: planned prosthesis which could
mucosal design, they could only be submerged when
not be placed due to implant failure(s), loss of
the soft tissues were sufficiently thick. Periapical radio-
the prosthesis secondary to implant failure(s) and
graphs (baseline) were made with the paralleling tech-
replacement of the prosthesis for any reasons.
nique. If bone levels around the study implants were • Implant failure: implant mobility, removal of sta-hidden or difficult to estimate, a second radiograph
ble implants dictated by progressive marginal
was made. Ibuprofen 400 mg was prescribed to be
bone loss or infection, and any mechanical com-
taken 2 to 4 times a day during meals, in the presence
plications rendering the implant unusable (e.g.
of pain, as long as required. Patients were instructed
implant facture). Stability of each individual im-
to place 1% chlorhexidine gel on the wounds twice a
plant was measured at delivery of definitive pros-
day for 2 weeks, to avoid brushing and trauma on the
theses (4 months after implant placement) and
surgical sites, and were advised to have a soft diet for
4 months after initial loading by tightening the
1 week. No removable prostheses were allowed on
abutment screws using a manual wrench with a
treated areas. Sutures were removed after 10 days,
25 Ncm force with the removed prostheses.
and patients were controlled at 20 days, one and two • Any biological or prosthetic complications. months after placement of dental implants.
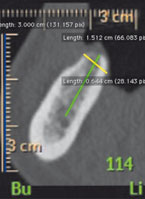
• Peri-implant marginal bone levels changes eval-
uated on intraoral radiographs taken with the paralleling technique at implant placement, at
Prosthetic procedures
delivery of definitive prostheses and 4 months
After 3 months of unloaded healing, when necessary,
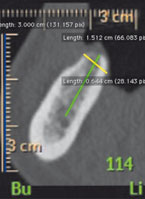
after loading. Radiographs were scanned in TIFF
implants were exposed, manually tested for stability,
format with a 600 dpi resolution, and stored in a
and impressions with the pick-up impression copings
personal computer. Peri-implant marginal bone
were taken using a polyether material (Impregum
levels were measured using the OsiriX (Pixmeo
3M/ESPE, Neuss, Germany) and customised resin
Sarl, Bernex, Switzerland) software. The soft-
impression trays. Impressions of submerged implants
ware was calibrated for every single image using
were taken after 2 weeks of soft tissue healing. Four
the known implant diameter. Measurements of
months after placement, implants were manually
the mesial and distal bone crest level adjacent to
tested for stability and definitive metal-composite or
each implant were made to the nearest 0.01 mm
metal-resin screw-retained restorations, rigidly join-
and averaged at implant level, then at patient
ing the implants, were connected directly on the
level and finally at group level. The measure-
implants, in light occlusion with the antagonistic
ments were taken parallel to the implant axis.
dentition, and oral hygiene instructions were deliv-
Reference points for the linear measurements
ered. Periapical radiographs of the study implants
were the most coronal margin of the implant
were taken, and in the case of unreadable radio-
collar and the most coronal point of bone-to-
graphs, new radiographs were taken.
implant contact.
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
Methodological aspects
lysed the data. The patient was the statistical unit of the analyses. Differences in the proportion of
Two clinicians (Dr Vittorio Checchi at Dr Pietro patients with prosthesis failures, implant failures and Felice's and Luigi Checchi's centres, and Dr Roberto complications (dichotomous outcomes) between the Cassoni at Dr Roberto Pistilli's centre) not involved two groups were compared using the Fisher's exact in patient treatment performed all clinical measure-
test and binomial 95% confidence intervals were
ments without knowing group allocation. One den-
computed. The non-Gaussian distribution of radio-
tist (Carlo Barausse) not involved in the treatment of graphic bone levels suggested the use of non- para-the patients performed all the radiographic assess-
metric tests. Difference of means for radiographic
ments and therefore the different implant lengths bone levels between the groups were compared could be easily identified on the periapical radio-
by Mann-Whitney U test and bias was corrected
and accelerated 95% confidence intervals were
A sample size calculation was performed using computed (IBM-SPSS Statistics Release 21). Com-
patients whom experienced at least one implant fail-
parisons between each time points and the baseline
ure as a primary outcome measure with 80% power measurements were made by the Wilcoxon test for ( = 0.2) and one-sided _ = 0.05. No previous study paired data, to detect any changes in marginal peri-on the same topic was carried out at the time of implant bone levels. A chi-square test was used to the research protocol. Consequently the sample size compare the number of prosthesis failures, implant was computed on the basis of a similar study7 that failures and complications and the Kruskal–Wallis reported that 3 years after loading, 7% of patients one-way analysis of variance was used to assess the lost short implants and 10% long implants. A failure marginal bone levels amongst the centres. All statis-rate of 0.07 in the control group was estimated. The tical comparisons were conducted at the 0.05 level minimal difference which was considered clinically of significance. relevant was set at 0.08, in agreement also with the clinicians' opinion. Based on this consideration, 160 patients were needed in total, however we only
Results
had sufficient resources to recruit 150 patients. One hundred and fifty patients with partial edentulism or One hundred and sixty-four patients were screened to be rendered partially edentulous in the posterior for eligibility, but 14 patients were not included in jaws were included in the trial: 75 patients received the trial because they did not want to be randomised 4.0 x 4.0 mm-long implants (short implant group) and wished to have longer implants. One hundred and 75 patients received 8.5 mm-long or longer and fifty patients were considered eligible and were implants (long implant group).
consecutively enrolled in the trial, four patients at
A computer generated restricted randomisation Dr Checchi's centre; 96 at Dr Felice's centre who
list was created. Only one of the investigators (Dr also treated those remaining 46 patients who should Maria Rosaria Gatto), not involved in the selection have been treated by Dr Checchi's centre, and 50 and treatment of the patients, was aware of the patients at Dr Pistilli's centre. Seventy-five patients random sequence and had access to the random were treated with short implants (Figs 3a to 3g) list stored in a password protected portable com-
and 75 patients with long implants (Figs 4a to 4f).
puter. Information on how to treat each patient All patients were treated according to the allocated was enclosed in sequentially numbered, identical, interventions.
opaque, sealed envelopes. Envelopes were opened
No patient dropped out from the study before
sequentially after flap elevation; therefore, treat-
the 4-month follow-up and data of all patients were
ment allocation was concealed to the investigators evaluated in the statistical analyses. No substantial in charge of enrolling and treating the patients.
deviations from the protocol occurred, except that
All data analysis was carried out according to a Dr Checchi treated only four patients out of the 50
pre-established analysis plan. A biostatistician with patients planned and the remaining quota of his expertise in dentistry (Dr Maria Rosaria Gatto) ana-
patients were treated by Dr Felice. In addition, one
Eur J Oral Implantol 2015;8(3):221–230



Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
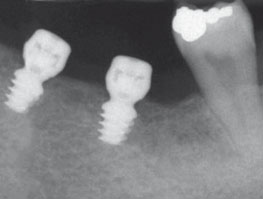
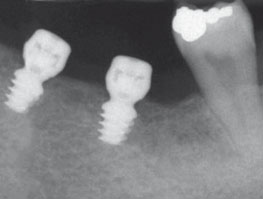
Fig 3 Treatment sequence of a patient with posterior mandibular edentulism randomly allocated to 4.0 x 4.0 mm implants: a) preoperative CBCT
showing the measurements to evaluate patient eligibility; b) surgical area after flap elevation; c) 4.0 x 4.0 mm-long implants to be placed; d) baseline
periapical radiograph taken after implant placement, showing two 4.0 x 4.0 mm-long implants; e) periapical radiograph taken at delivery of definitive
prosthesis 4 months after implant placement; f) periapical radiograph taken 4 months after initial loading; g) clinical view at 4-month post-loading.
Fig 4 Treatment sequence of a patient with posterior mandibular edentulism randomly allocated to the 8.5 x 4.0 mm or longer implant group: a)
preoperative CBCT showing the measurements to evaluate patient eligibility; b) baseline periapical radiograph taken after implant placement showing a
8.5 x 4.0 mm-long implant; c) clinical view after 4 months of non-submerged healing; d) periapical radiograph taken at delivery of definitive prosthesis
4 months after implant placement; e) periapical radiograph taken 4 months after initial loading; f) clinical view at 4-month post-loading.
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
Table 1 Patient and intervention characteristics.
4.0 mm-long implants
8.5 mm or longer
implants (75 patients)
Mean age at recruitment (range)
Smokers (smoking >10 cigarettes)
No. of implants in maxillas
No. of post-extractive implants
No. of augmented post-extractive implants
No. of implants placed with < 25 Ncm torque
Mean implant length
No. of patients with submerged implants
No. of patients receiving 1 implant
No. of patients receiving 2 implants
No. of patients receiving 3 implants
No. of patients rehabilitated with metal-resin prostheses
Table 2 Summary of the main results expressed as number of patients who experienced at least one negative event. All
patients had only one negative event each.
Differences in 95% CI
75 patients
75 patients
Patients with failed prostheses
Patients with failed implants
Patients with complications
patient of Dr Felice's group received a provisional P = 0.69; Table 2). Two prostheses (one from each resin prosthesis instead of the definitive one because group) were delivered with 4 months delay and two of financial problems.
patients (one from each group), at the moment of
Patients were recruited and had their implant writing this article, had their replacement implants
placed from September 2013 to February 2014. The healing unloaded.
follow-up of all patients was 4-month post-loading.
Five patients experienced one implant failure
The main baseline patient and intervention char-
each: three short and two long implants failed.
acteristics are presented in Table 1. Initially, 124 The difference in proportions for implant failures implants were placed in the short group and 116 in was not statistically significant (difference in pro-the long group. There were no apparent significant portion = 0.01; 95% CI -0.06 to 0.09; P = 0.50; baseline imbalances between the two groups with Table 2). In the short implant group one implant in the exception that more 4.0 mm-long implants were position 16, inserted with a torque < 25 Ncm, was placed in mandibles.
found to be mobile and painful at percussion. The
The main results up to 4-month post-loading are implant was removed and immediately replaced
summarised in Table 2.
by an identical implant 11.5 mm-long. It was suc-
Two prostheses could not be placed when cessfully loaded 4 months after. One immediate
planned because of early implant failures at both post-extractive implant in position 44 and inserted groups. The difference in observed proportions for with a torque < 25 Ncm, was found to be mobile prosthesis failures was not statistically significant 4 months after insertion and immediately replaced (difference in proportion = 0; 95% CI -0.07 to 0.07; with an identical implant 10.0 mm long. The implant
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
has not been loaded yet. Another implant, inserted implant placement and 4 months after loading (95% with a torque < 25 Ncm in position 36, was mobile CI: -0.041 to 0,117; P = 0.274) (Table 4) between and painful during impression taking and there-
the two groups for peri-implant bone level changes.
fore was removed. It was not replaced since there
There were no statistically significant differences
were successful implants in positions 35 and 37. for failures, complications and marginal bone level Two long implants failed: one 13 mm-long implant changes at 4-month post-loading between the three in position 26 was found to be mobile and painful centres (Table 5).
at percussion after 4 months. It was removed and immediately replaced with a short but wider implant (4.7 x 6.0 mm, I-RES Shape 1, I-RES, Milan, Italy).
After 4 months of submerged healing the implant was successfully loaded. Another 11.5 mm-long im-
This study evaluated whether a 4.0 x 4.0 mm implant
plant placed as an immediate post-extractive implant supporting a partial fixed prosthesis could be at higher in position 35 with an insertion torque < 25 Ncm was risk of failure than longer implants when placed in found to be mobile and painful 3.5 months after posterior jaws with adequate bone volumes. We were placement. The patient confessed to playing with the interested in assessing the clinical performance of very tongue on the implant. The implant was removed short implants (4.0 mm long) with a conventional and immediately replaced with an identical 10.0 x diameter of 4.0 mm in order to understand what is 4.0 mm implant inserted with a torque > 25 Ncm. the minimal amount of bone in order to be able to The implant was still unloaded at the time of writing support functionally loaded dental implants.
this manuscript
Previous studies suggested that short implants
Five patients experienced one complication each: can achieve clinical results which are as effective, if
three complications occurred for short implants not better, than long implants placed in augmented and two for long implants. There was no statistic-
bone up to 5 years after loading, however often sur-
ally significant differences with regard to complica-
geons use short implants with wider bodies to com-
tions between the two groups (difference in pro-
pensate for the lack of implant height3,5,14,15. While it
portion = 0.01; 95% CI -0.06 to 0.09; P = 0.50; is still unclear whether this ‘compensation' is actually Table 2). The following complications occurred needed, preliminary results of this and many other tri-for short implants: two patients experienced some als8,11,12,15-18 in which 5.0 to 6.0 mm-long implants pain when touching the implants. Both implants with diameters of 4.0 to 5.0 mm were used suggest were mobile and were removed. Another patient that short implants with diameters of 4.0 to 5.0 mm lost the cover screw 20 days after surgery, which perform well, at least up to 5-years post-loading. was replaced without any consequences. The two
When comparing the present data to those of
implants belonging to the long implant group cre-
previous similar RCTs16,18,19, all trials showed iden-
ated pain in patients when under pressure. Both tical trends: there were similar outcomes between implants were mobile and were removed. Failures 5.0 to 6.0 mm-long implants and 10.0 mm or longer were not considered as complications, unless pain implants up to 1-year post-loading, in the presence was present, therefore, the presence of pain was of adequate bone volumes. Obviously follow-ups considered as a complication.
of at least 5-years post-loading are needed to draw
Marginal bone levels are described in Table 3. more reliable conclusions. In the present trial, five
Both groups gradually lost statistically significant implants were lost in total: three 4 mm-long implants marginal peri-implant bone (P = 0.001) at loading and two longer ones. All failures were detected at (0.28 mm for short implants and 0.24 mm for long abutment connection and four of the failed implants implants) and 4 months after loading (0.38 mm were replaced. No apparent sign of infection were for short implants and 0.42 mm for long implants; noted but implants were usually painful during per-Table 4). There was no statistically significant dif-
cussion and mobile indicating that osseointegration
ference between implant placement and loading did not take place20. Failures occurring earlier are (95% CI: -0.157 to 0.077; P = 0.324) and between easier to handle, in fact four of the mobile implants
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
Table 3 Mean radiographic peri-implant marginal bone levels between groups and time periods.
4 months after loading
N Mean (SD)
N Mean (SD) 95% CI
N Mean (SD) 95% CI
75 0.021 (0.075)
74 0.298 (0.506) 0.205; -0.414 74 0.399 (0.264) 0.345; -0.457
73 0.255 (0.160) 0.218; -0.292 73 0.434 (0.245) 0.377; -0.497
Mann-Whitney U-test
Table 4 Comparison of mean changes in peri-implant marginal bone levels at loading and 4 months after loading.
Placement – loading
Placement – 4 months after loading
N Mean (SD) 95% CI
N Mean (SD) 95% CI
74 -0.277 (0.488)
-0.193; -0.388 74 -0.378 (0.248)
73 -0.237 (0.162)
-0.202; -0.268 73 -0.416 (0.240)
-0.157; 0.077 0.038
Mann-Whitney U-test P-value
Table 5 Comparisons between the three study centres at 4 months after loading.
Dr Felice
Dr Pistilli
Dr Checchi
96 patients
50 patients
4 patients
Patients with implant failures
Patients with prosthesis failures
Patients with complications
Mean peri-implant bone level changes in mm
from implant placement to 4 months after loading
were immediately replaced with other implants the
The main limitation of the present trial is the short
same day that they were removed, minimising patient duration of the follow-up, however longer follow-discomfort, although the delivery of the prostheses ups will be carried out. The positive aspects of this in those patients was delayed for up to 4 additional study are that all treated patients were accounted for months. In at least one case the patient declared that with no exclusions and all assessments were done by she was continuously touching the transmucosal independent assessors. The tested interventions were portion of the implant with her tongue and most of evaluated in real clinical conditions and the patient the failed implants were placed with insertion tor-
inclusion criteria were rather broad. Similar results
ques < 25 Ncm. It is possible that several unwanted should be obtained by other experienced operators movements disrupted the bone healing around treating patients with similar characteristics.
these implants and this could have been caused by the fibrointegration of these implants20. On the one hand, a short two-piece 4 mm-long implant without a
transmucosal portion, to be positioned at crestal level, could be developed and tested. However, peri-implant Short-term data (4 months after loading) indicate marginal bone loss was minimal (about 0.4 mm) for that 4.0 x 4.0 mm implants achieved similar results to both groups up to 1 year after loading. It may be that 8.5 x 4.0 mm-long or longer implants in the presence this minimal bone loss could be partly explained by of adequate bone volumes, however 5- to 10-years the lack of an implant-abutment junction at the level post-loading data from larger trials are necessary of the crest, which could harbour bacteria that could before reliable recommendations can be made. enhance peri-implant marginal bone loss.
Eur J Oral Implantol 2015;8(3):221–230
Esposito et al 4.0 x 4.0 mm versus longer implants in posterior jaws
11. Pistilli R, Felice P, Cannizzaro G, Piatelli M, Corvino V,
Barausse C, Buti J, Soardi E, Esposito M. Posterior atrophic
1. Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Wor-
jaws rehabilitated with prostheses supported by 6 mm long
thington HV, Coulthard P. Interventions for replacing missing
4 mm wide implants or by longer implants in augmented
teeth: horizontal and vertical bone augmentation techniques
bone. One-year post-loading results from a pilot randomised
for dental implant treatment. Cochrane Database Syst Rev
controlled trial. Eur J Oral Implantol 2013;6:359–372.
12. Pistilli R, Felice P, Piattelli M, Gessaroli M, Soardi E,
2. Felice P, Cannizzaro G, Checchi V, Marchetti C, Pellegrino G,
Barausse C, Buti J, Corvino V. Posterior atrophic jaws reha-
Censi P, Esposito M. Vertical bone augmentation versus
bilitated with prostheses supported by 5 x 5 mm implants
7-mm-long implants in posterior atrophic mandibles. Results
with a novel nanostructured calcium-incorporated titanium
of a randomized controlled clinical trial of up to 4 months
surface or by longer implants in augmented bone. One-year
after loading. Eur J Oral Implantol 2009;2:7–20.
results from a randomised controlled trial. Eur J Oral Implan-
3. Felice P, Checchi V, Pistilli R, Scarano A, Pellegrino G, Espos-
ito M. Bone augmentation versus 5-mm dental implants 13. Slotte C, Gronningsaeter A, Halmoy AM, Ohrnell LO, in posterior atrophic jaws. Four-month post-loading results
Stroh G, Isaksson S, Johansson LA, Mordenfeld A, Eklund J,
from a randomised controlled clinical trial. Eur J Oral Implan-
Embring J. Four-millimeter implants supporting fixed partial
dental prostheses in the severely resorbed posterior mandi-
4. Felice P, Pellegrino G, Checchi L, Pistilli R, Esposito M. Verti-
ble: two-year results. Clin Implant Dent Relat Res 2012;14
cal augmentation with interpositional blocks of anorganic
bovine bone vs. 7-mm-long implants in posterior mandibles:
14. Cannizzaro G, Felice P, Leone M, Viola P, Esposito M. Early
1-year results of a randomized clinical trial Clin Oral Implants
loading of implants in the atrophic posterior maxilla: lateral
sinus lift with autogenous bone and Bio-Oss versus crestal
5. Esposito M, Pellegrino G, Pistilli R, Felice P. Rehabilitation of
mini sinus lift and 8-mm hydroxyapatite-coated implants.
posterior atrophic edentulous jaws: prostheses supported by
A randomised controlled clinical trial. Eur J Oral Implant
5 mm short implants or by longer implants in augmented
bone? One-year results from a pilot randomised clinical trial.
15. Felice P, Cannizzaro G, Barausse C, Pistilli R, Esposito M.
Eur J Oral Implantol 2011;4:21–30.
Short implants versus longer implants in vertically aug-
6. Felice P, Soardi E, Pellegrino G, Pistilli R, Marchetti C, Ges-
mented posterior mandibles: a randomised controlled trial
saroli M, Esposito M. Treatment of the atrophic edentulous
with 5-year after loading follow-up. Eur J Oral Implantol
maxilla: short implants versus bone augmentation for placing
longer implants. Five-month post-loading results of a pilot ran-
16. Gulje F, Abrahamsson I, Chen S, Stanford C, Zadeh H, Palm-
domised controlled trial. Eur J Oral Implantol 2011;4:191–202.
er R. Implants of 6 mm vs. 11 mm lengths in the posterior
7. Esposito M, Cannizzaro G, Soardi E, Pellegrino G, Pistilli
maxilla and mandible: a 1-year multicenter randomized
R, Felice P. A 3-year post-loading report of a randomised
controlled trial. Clin Oral Implants Res 2013;24:1325–1331.
controlled trial on the rehabilitation of posterior atrophic 17. Gulje FL, Raghoebar GM, Vissink A, Meijer HJ. Single mandibles: short implants or longer implants in vertically
crowns in the resorbed posterior maxilla supported by either
augmented bone? Eur J Oral Implantol 2011;4:301–311.
6-mm implants or by 11-mm implants combined with sinus
8. Esposito M, Cannizzaro G, Soardi E, Pistilli R, Piattelli M,
floor elevation surgery: a 1-year randomised controlled trial.
Corvino V, Felice P. Posterior atrophic jaws rehabilitated with
Eur J Oral Implantol 2014;7:247–255.
prostheses supported by 6 mm-long 4 mm-wide implants or
18. Romeo E, Storelli S, Casano G, Scanferla M, Botticelli D.
by longer implants in augmented bone. Preliminary results
Six mm versus 10 mm long implants in the rehabilita-
from a pilot randomised controlled trial. Eur J Oral Implantol
tion of posterior edentulous jaws: a 5-year follow-up of a
randomised controlled trial. Eur J Oral Implantol 2014;7:
9. Cannizzaro G, Felice P, Minciarelli AF, Leone M, Viola P,
Esposito M. Early implant loading in the atrophic posterior
19. Cannizzaro G, Felice P, Buti J, Leone M, Ferri V, Esposito M.
maxilla: 1-stage lateral versus crestal sinus lift and 8 mm
Immediate loading of fixed cross-arch prostheses supported
hydroxyapatite-coated implants. A 5-year randomised con-
by flapless-placed supershort or long implants: 1-year results
trolled trial. Eur J Oral Implantol 2013;6:13–25.
from a randomised controlled trial. Eur J Oral Implantol
10. Esposito M, Felice P, Worthington HV. Interventions for
replacing missing teeth: augmentation procedures of the 20. Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological fac-maxillary sinus. Cochrane Database Syst Rev 2014 13;(5):
tors contributing to failures of osseointegrated oral implants
(II). Etiopathogenesis. Eur J Oral Sci 1998;106:721–764.
Eur J Oral Implantol 2015;8(3):221–230
Source: http://www.tekkaglobald.it/wp-content/uploads/2015/11/Esposito2015RCT-4x4-Global-D-4-month.pdf
HARMONIZING STANDARDS AS INSTITUTIONS Monika Tothova and James F. Oehmke (Paper Presented on the 7th International Conference on "Institutions in Transitions", Kranjska Gora, Slovenia, June 19-20, 2003) Integration efforts of the Central and Eastern European (CEE) countries are gradually materializing. Czech Republic, Estonia, Hungary, Latvia, Lithuania, Poland, Slovakia and Slovenia, and in addition to Cyprus and Malta, are to join the EU on May 1 2004 after the Accession Treaty is ratifiedthusiasm is apparent in every accession country, less optimistic opinions are also voiced. One of the first short- and medium-term priorities in each country was to establish and consolidate standardization and conformity assessment structures. While the concept of "deeper integration beyond abolition of import tariffs and quotas, to further measures to remove market segmentation and promote integration" (Venables 2000) is by and large not questioned, critical views on potential losses of national standards harming national identity – i.e., what constitutes "rum", and how to address cheeses made from non-pasteurized sheep milk – are seen as well. The issue of "lost national standards" is repeated: in 1987 the EU (then European Community) published its visionary plan on new, standardized Europe of 1992; a gain of 7 per cent of European income was estimated from harmonization (Emerson 1988, p.6). Even then British were opposed to some parts of it, claiming "brilliant green mushy peas" and "pink sausages" are part of their national identity, and eventually succeeded in getting the necessary exemptions (Krugman and Obstfeld 2002). Although the harmonization issue has been on the tables in Brussels at least since the late 1980s, it yet has to be concluded. Over the years "new" approach replaced the "old" one: instead of imposing technical solutions, the EU legislation is limited to establishing the essential requirements which products must meet (EC 2003). Differences in quality standards are protected by World Trade Organization's (WTO) recognition of countries' right to adopt the standards they consider appropriate – i.e., for human, animal or plant life or health, for the protection of the environment or to meet other consumer interests assuming their use is justified and they are not used as barriers to trade (WTO 2003). Although countries are urged to apply international food standards (when existing), suggestions of Codex Alimentarius result is a variety of standards and technical regulations across the world and consequent welfare losses. Reaching out for an example from outside Europe, tolerance levels for
CLINICAL CROSSROADS CONFERENCES WITH PATIENTS AND DOCTORS An 83-Year-Old Woman With ChronicIllness and Strong Religious BeliefsHarold G. Koenig, MD, Discussant strength was decreased, sensation to pinprick was de-creased in the digits bilaterally, and motor strength of the DR BURNS: MRS A IS AN 83-YEAR-OLD WOMAN WHO HAS MUL- lower extremities was 2/5 proximally and 3/5 distally. Her