Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Doi:10.1016/j.gie.2008.01.028

Role of endoscopy in the bariatric surgery patient
This is one of a series of statements discussing the uti-
frankly obese, and 4.8% had a BMI R 40 kg/m2.Further-
lization of GI endoscopy in common clinical situations.
more, several studies showed that obesity is associated
The Standards of Practice Committee of the American
with an increased risk for morbidity and all-cause
Society for Gastrointestinal Endoscopy (ASGE) prepared
mortality.In recognition of these risks and the evidence
this text. In preparing this guideline, MEDLINE and
for risk reduction associated with weight loss,the National
PubMed databases were used to search for publications
Institutes of Health has recommended weight loss surgery
from the last 15 years that are related to endoscopy by us-
as an appropriate alternative in carefully selected individ-
ing the keyword ‘‘endoscopy'' and each of the following:
uals with severe obesity (BMI R 40 kg/m2 or those with
‘‘bariatric,'' ‘‘obesity,'' ‘‘gastroplasty,'' ‘‘gastric bypass,''
a BMI R 35 kg/m2 and with serious comorbid conditions)
‘‘Roux-en-Y,'' and ‘‘weight loss.'' The search was supple-
when dietary, behavioral, and pharmacotherapy interven-
mented by accessing the ‘‘related articles'' feature of
tions failed.
PubMed with articles identified on MEDLINE and
Bariatric surgery results in durable and significant
PubMed as the references. Pertinent studies published
weight loss. The rising prevalence of obesity and the suc-
in English were reviewed. Studies or reports that
cess of surgical interventions led to a marked increase in
described fewer than 10 patients were excluded from
the number of weight-loss surgeries performed in the
analysis if multiple series with more than 10 patients
United States, from 13,365 in 1998 to 102,794 in
that addressed the same issue were available. The resul-
Early bariatric surgical techniques (eg, jejunoileal bypass)
tant quality indicators were adequate for analysis. The
are no longer performed because they resulted in clini-
reported evidence and recommendations based on
cally significant and serious vitamin deficiencies, steatohe-
reviewed studies were graded on the strength of the
patitis, and even cirrhosis in some patients.Instead,
supporting evidence .
various procedures that cause weight loss through volume
Guidelines for appropriate utilization of endoscopy
restriction, limited malabsorption and maldigestion, be-
are based on a critical review of the available data
havioral modification, or some combination thereof
and expert consensus. Further controlled clinical studies
were developed. The most commonly used bariatric sur-
may be needed to clarify aspects of this statement, and
geries are laparoscopic or open Roux-en-Y gastrojejunal
revision may be necessary as new data appear. Clinical
bypass (RYGB) and laparoscopic adjustable gastric band-
consideration may justify a course of action at variance
ing (LOther surgeries include vertical banded
to these recommendations.
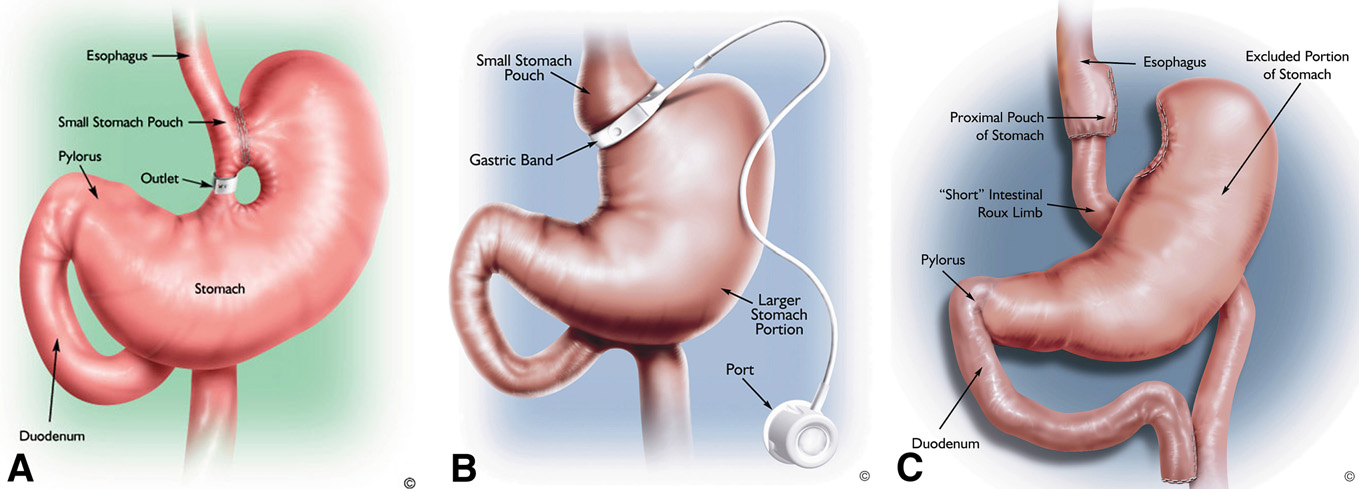
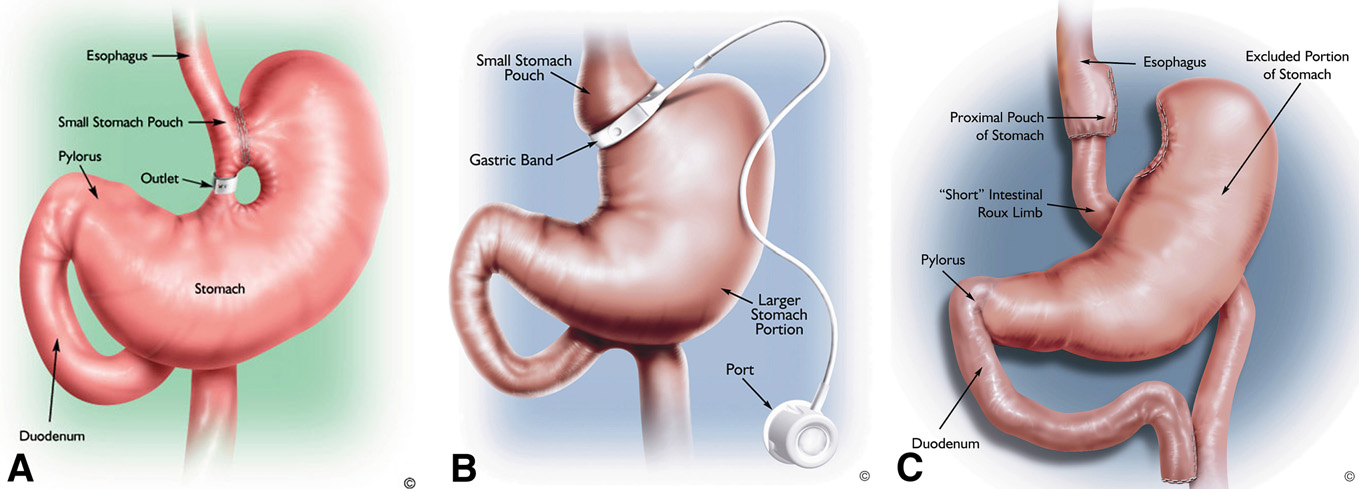
gastroplasty (VBG), and sleeve gastrectomy alone orwith duodenal switch and biliopancreatic diversion (DS/BPD). It is useful to understand the anatomical alterationscreated by these operations as they pertain to the mecha-
nisms for weight loss (, ), expected compli-cations, and considerations for endoscopic evaluation.
Obesity in the United States is a major health problem
that contributes to increased morbidity and mortality andto a host of disease processes.Body mass index (BMI) is
EVALUATION OF THE PREOPERATIVE PATIENT
calculated as weight/height2 (kg/m2) and is commonlyused to classify overweight (BMI 25.0-29.9 kg/m2) and obese
The role of upper endoscopy in the preoperative
(BMI R 30.0 kg/m2) adults. Based on data obtained from
evaluation of patients undergoing bariatric surgery may
the National Health and Nutrition Examination Survey
be based, in part, on the presence or absence of symp-
from 2003 to 2004, 61% of adults over the age of 20 years
toms. The performance of an upper endoscopy in a patient
in the United States are overweight or obese, 32.2% are
with reflux symptoms, dysphagia, and/or dyspepsia hasbeen covered in recent guidelines and is equally relevantin the preoperative patHowever, because RYGBand DS/BPD render the distal stomach and/or duodenuminaccessible by a standard upper endoscope, the thresh-
Copyright ª 2008 by the American Society for Gastrointestinal Endoscopy0016-5107/$32.00
old for performing a preoperative endoscopic evaluation
of the upper-GI tract is lower than for other surgeries.
Volume 68, No. 1 : 2008 GASTROINTESTINAL ENDOSCOPY 1
Role of endoscopy in the bariatric surgery patient
TABLE 1. Grades of recommendation
Grade of recommendation
Clarity of benefit
Methodologic strength support-
Randomized trials without
Strong recommendation; can be
important limitations
applied to most clinical settings
Randomized trials with important
Strong recommendation; likely to
limitations (inconsistent results,
apply to most practice settings
nonfatal methodologic flaws)
Overwhelming evidence from
Strong recommendation; can apply
observational studies
to most practice settings in mostsituations
Observational studies
Intermediate-strengthrecommendation; may changewhen stronger evidence is available
Randomized trials without
important limitations
recommendation; best action maydiffer depending on circumstancesor patients' or societal values
Randomized trials with important
Weak recommendation; alternative
limitations (inconsistent results,
approaches may be better under
nonfatal methodologic flaws)
some circumstances
Observational studies
Very weak recommendation;alternative approaches likely to bebetter under some circumstances
Expert opinion only
Weak recommendation; likely tochange as data become available
*Adapted from Guyatt G, Sinclair J, Cook D, et al. Moving from evidence to action. Grading recommendations: a qualitative approach. In: Guyatt G, Rennie D,editors. Users' guides to the medical literature. Chicago: AMA Press; 2002. p. 599-608.
studies in this group. However, the presence of a large hi-
TABLE 2. Mechanism of weight loss for common obesity
atal hernia represents a relative contraindication to LAGB
because of an increased risk for band slippage.In addi-tion, some surgeons advocate crural tightening in patients
with a hiatal hernia when these patients are undergoing
any weight loss operat
Multiple studies have been published that demonstrate
that routine endoscopy before LAGB,and
Roux-en-Y can identify a variety of pathologies, including
hiatal hernia, esophagitis, and gastric ulcers. The majority
of patients with pathology in these studies were asymp-
tomatic. Importantly, no malignancies were identified, al-
though, in 2 studies, the endoscopic findings resulted inan alteration of the surgical approach or a delay in sur-
The rationale for performing an EGD before bariatric sur-
geryGuidelines from outside the United States rec-
gery is to detect and/or treat lesions that might potentially
ommend preoperative upper endoscopy in all patients
affect the type of surgery performed, cause complications
before bariatric surgery, regardless of the presence or
in the immediate postoperative period, or result in symp-
absence of symAlthough an upper endoscopy
toms after surgery. In particular, a recent meta-analysis
in patients without symptoms can identify lesions that
showed that obesity was associated with a significantly in-
may alter surgical management, there are no studies that
creased risk of GERD, erosive esophagitis, and esophageal
evaluated the effect of a preoperative endoscopy on surgi-
adenocarcinoma.The value of a routine endoscopy be-
cal outcome. Contrast studies may be an alternative to an
fore bariatric surgery in the patient without symptoms re-
endoscopy and can provide complementary information
mains controversial because of limited observational
2 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 1 : 2008

Role of endoscopy in the bariatric surgery patient
Figure 1. Illustrations of various weight loss surgeries. A, VBG. B, Laparoscopic adjustable gastric band. C, RYGB. (Courtesy Ethicon Endo-Surgery, Inc.)
Helicobacter pylori infection is present in 30% to 40%
of patients scheduled for bariatric surgery, and preopera-tive testing in these patients may be usefIn onestudy of patients without symptoms who were scheduledfor an RYGB, the patients with a positive rapid urease testwere significantly more likely to have an abnormal endos-copy than those who tested negative (94% vs 51%).Inanother study, patients with H pylori infection weremore likely to develop postoperative marginal ulcersIn patients without symptoms and who were not undergo-ing an endoscopy, noninvasive H pylori testing, followedby treatment, if positive, is recommended.
ENDOSCOPY IN THE POSTOPERATIVE PATIENT
General principles
When an endoscopy is considered in a patient who had
bariatric surgery, the endoscopist should be aware of the
Figure 2. Illustration of sleeve gastrectomy. (Courtesy Ethicon Endo-Sur-
operative procedure performed and the findings on
preprocedural imaging studies, and must understand theexpected anatomy, including the extent of resection andthe length of surgically created limbs. Direct communica-
radiography as an initial diagnostic test. Contrast studies
tion with the surgeon, if possible, is advisable. Feitoza and
are complementary to an endoscopy and are also helpful
published a detailed review of endoscopy in
in delineating anatomy.
patients with postsurgical anatomy, including information
The expected endoscopic findings after an RYGB in-
on the equipment needed for successful completion of di-
clude a normal esophagus and gastroesophageal junction.
agnostic and therapeutic procedures, and tips on access-
The size of the gastric pouch varies. Special care should be
ing the distant or excluded portions of the GI tract. The
made to examine the pouch and suture line for fistulas
choice of endoscope will depend on the indication and
and ulcerations. The gastrojejunal stoma should be care-
the need for intubation of the excluded limb or therapeu-
fully examined. The width of the anastomosis is generally
tic intervention (eg, ERCP). In patients who are in the
10 mm to 12 mm in diameter. Beyond the anastomosis,
early postoperative period, air insufflation may have
a short, blind limb is often visible alongside the efferent
potentially detrimental effects in the presence of leaks
jejunal limb. The jejunojejunal anastomosis can some-
and/or tenuous anastomoses. If there is suspicion of
times be reached with an upper endoscope, depending
a leak, then the endoscopist should consider contrast
on the length of the Roux limb. It should be noted that
Volume 68, No. 1 : 2008 GASTROINTESTINAL ENDOSCOPY 3

Role of endoscopy in the bariatric surgery patient
TABLE 3. Signs and symptoms prompting possibleendoscopic evaluation after bariatric surgery
Upper-GI symptoms
TABLE 4. Upper-GI postbariatric surgical complications
Figure 3. Illustration of DS/BPD. (Courtesy Ethicon Endo-Surgery, Inc.)
the length of the Roux limb after an RYGB can vary signif-
Band erosion and slippage
icantly from standard Roux limbs created for nonbariatric
procedures and can range from 50 to 150 cm. The distal orexcluded stomach cannot be visualized in the absence ofa fistula with a regular gastroscope. A VBG produces a gas-tric pouch somewhat similar in appearance to an RYGB.
INDICATIONS FOR AN ENDOSCOPY IN THE
The banded stoma is generally 10 to 12 mm in diameter,
PATIENT AFTER GASTRIC BYPASS OR WITH
and, once traversed, the distal stomach and duodenum
A PREVIOUS BYPASS
can be visualized.
The sleeve gastrectomy produces a long tubular stom-
ach limited in expansion by a staple line that parallels
Nausea, vomiting, and abdominal pain are among the
the lesser curvature. The staple line should be examined
most commonly encountered symptoms after bariatric sur-
for defects and ulcerations. The duodenal switch proce-
gery and may result from one or several structural and func-
dure is often performed in conjunction with a sleeve gas-
tional etiologies. Symptoms are frequently associated with
trectomy, but also includes a duodeno-jejunal anastomosis
dietary noncompliance as to the volume and type of foods
visible just distal to an intact gastric pylorus. In the latter,
eaten, rapid ingestion, or inadequate chewing. Patients
the ampulla is thus not available for visualization or ERCP
with persistent symptoms, despite counseling and behavior
in a standard fashion.
modification, should be evaluated, because these symp-
Laparoscopic adjustable gastric bands produce a vari-
toms may indicate the development of marginal ulcers, gas-
able amount of extrinsic circumferential compression on
trogastric fistulas, postsurgical reflux disease, or partial or
the proximal stomach that is evident on upper endoscopy.
complete anastomotic obstruction. An endoscopy is the
At the time of endoscopic evaluation, the endoscopist
preferred strategy, unless there is a suspicion of leaks or fis-
should note the length of the pouch as measured from
tulas, when contrast radiography is more appropriate. Pa-
the gastroesophageal junction to the impression of the
tient history may be helpful in differentiating the etiology
band to assess for pouch dilatation or band slippage.
of pain and in guiding the type of investigation. Nausea,
The endoscopist should also evaluate for the possible
vomiting, abdominal distention, and bloating alone or in
presence of band erosion into the gastric walThere
conjunction with abdominal pain can suggest an obstruc-
are a variety of symptoms and unique postsurgical compli-
tive cause, such as strictures, internal hernias, or bezoars,
cations after bariatric surgery These will
but may also be an indication of dumping syndrome. Also,
be discussed in the following sections.
dysphagia can result from esophageal dysmotility or
4 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 1 : 2008
Role of endoscopy in the bariatric surgery patient
gastrojejunal anastomotic stenosis. In one study, 62% of pa-
can result in cutaneous fistula, peritonitis, abscess, sepsis,
tients who were seen with persistent nausea and vomiting
organ failure, and dClinical manifestations include
and 30% of those who are seen with abdominal pain or dys-
tachycardia; fever; nausea; vomiting; and flank, abdominal,
pepsia after an RYGB had significant findings on upper en-
or chest pain. Most leaks occur at the gastrojejunal anasto-
doscopy, including marginal ulcers, stomal stenosis, and
mosis, with nearly all the rest occurring in the remnant
staple-line dehiscence
(excluded) stomach; leaks from the jejunojejunal anasto-mosis are less common but do occur and usually require
reoperation. Early postoperative extraluminal leaks are
Marginal ulcers are typically seen 1 to 6 months after
usually diagnosed by upper-GI contrast studies or CT, al-
surgery and may present with abdominal pain, bleeding,
though the false-negative rate was reported at
or nausea, although they may also be asymptomatic
There is little role for an endoscopy in the presence of
The ulcers occur at the gastrojejunal anastomosis, usually
known leaks or fistulas in the early postoperative period.
on the intestinal side, and are thought to arise from a num-
An endoscopy can be considered if the patient is clinically
ber of factors, including local ischemia, staple-line disrup-
stable, there is uncertainty of the diagnosis, or if there is
tion, effects of acid on exposed intestinal mucosa, and the
a planned endoscopic interventio
presence of staples or suture material. Factors that in-
Chronic gastrogastric fistulas may be found in the pres-
crease the risk of marginal ulcers include smoking and
ence of marginal ulcers, and patients may present with
nonsteroidal anti-inflammatory drug use, whereas proton
nausea, vomiting, epigastric pain, and weight gain. An
pump inhibitor use appears to decrease the risk. The true
upper-GI contrast study is sensitive for their detection. A
incidence of a marginal ulcer after an RYGB is uncertain,
large fistula can also be visualized by an endoscopy.
with reports that range from !1% to 36%.
Endoscopic therapy for postoperative fistulas has beenperformed by using fibrin-glue injectioor self-ex-
panding stents.Case reports and small case series in-
Obesity itself is a risk factor for GERD, and symptomatic
dicate that fistula closure may also be achieved by using
GERD is frequent in the bariatric population, with a preva-
various combinations of mucosal ablation, glue, the
lence of 30% to The effects of bariatric interven-
application of endoscopic clips, the placement of self-
tions on GERD appear to be variable. Both gastric banding
expanding stents, and endoscopic suturing devices.
and RYGB were shown, in multiple series, to reduce GERD
However, these interventions cannot be routinely re-
symptoms at rates that approach or exceed
commended at this time, because of a lack of controlled
However, other studies suggest the converse, with in-
creased symptoms after surgeryand endoscopic evi-dence of reflux esophagitis in up to 56% of patients
Postoperative GERD may be related to gastrojejunal anas-
Gastrojejunal stomas are generally between 10 and
tomotic stenosis. In addition, patients who have postoper-
12 mm in diameter to maximize the restrictive nature of
ative symptoms may have underlying motility disorders;
the operation. Anastomotic strictures, defined as anasto-
one study suggests that gastric bands may aggravate symp-
moses that are smaller than 10 mm in diameter, are a com-
toms of GERD in this population.The variable results
mon complication of RYGB that occur in 3% to 28% of
may also represent differences in the size of the gastric
patients.The occurrence of gastrojejunal strictures
pouch or band position. It is suggested that the size of
may be associated with marginal ulcers. Patients with
the pouch and quantity of acid secretion influence the
anastomotic strictures generally present with nausea,
incidence and severity of GERD symptoms.
vomiting, or dysphagia, usually within the first year after
Symptoms of GERD after surgery should be managed
surgery.Stenosis can be identified by contrast radiogra-
as in patients who did not have a byAn endoscopy
phy, but direct endoscopic visualization is preferable,
should be reserved for the evaluation of symptoms refrac-
because it has high sensitivity.In addition, marginal
tory to medical therapy or to rule out complications of
ulceration can be identified, and dilation of strictures
GERD and inciting factors, such as obstruction of the gas-
can be performed.
trojejunal anastomosis, increased pouch size, or distal
Endoscopic dilation of anastomotic strictures can be
limb obstruction. Nonacid regurgitation in patients with
performed safely and effectively by using through-the-
a band might indicate an inappropriately tight band
scope balloon dilators and wire-guided bougie dila-
adjustment, and these patients should be referred to their
tors.If the stenosis cannot be traversed by an
surgeon for additional evaluation.
endoscopy, then fluoroscopy is useful to allow guidewirepassage. Gradual dilation over multiple sessions may
reduce the risk of perforaEven with multiple ses-
Gastric leaks and gastrogastric fistulas are potentially
sions, some stenoses cannot be adequately dilated by en-
serious complications of gastric bypass surgery and occur
doscopic means, and reoperation is needed.It is
in 1% to 6% of patients.Extraluminal gastric leaks
controversial if dilation to a diameter larger than 15 to
Volume 68, No. 1 : 2008 GASTROINTESTINAL ENDOSCOPY 5
Role of endoscopy in the bariatric surgery patient
16 mm should be performed, because it could possibly
phy. Band erosion may be asymptomatic or can produce
lead to weight regain. However, in one study, dilation to
abdominal pain, nausea, vomiting, abdominal access-
at least 15 mm was not associated with weight regain,
port–site infection, increased food intake or weight gain,
yet, it was associated with a reduced need for more
and GI bleeding. Band slippage may present with weight
gain, increasing reflux symptoms, or obstruction. Endo-
It is important to recognize that, in patients with an
scopic findings of band slippage may include an enlarged
RYGB, the Roux limb can be delivered to the upper abdo-
pouch size and reflux esophagitis, gastritis, or ulcers. In se-
men to connect with the gastric pouch in an antecolic fash-
vere cases, band slippage can lead to gastric necrosis, a po-
ion, in front of the transverse colon, or through a retrocolic
tentially life-threatening conditIn patients with
tunnel created in the transverse mesocolon. If this tunnel
VBG, endoscopic removal of the polypropylene mesh
is created too tightly or if postoperative stricturing occurs,
that had eroded into the stomach was repor
then this limb can be narrowed and lead to obstructivesymptoms.On endoscopic examination, the gastrojeju-
Bleeding and anemia
nal anastomosis will be normal, but the jejunum beyond
Bleeding in the patient after bariatric surgery may be
the anastomosis will be dilated until the point where it tra-
acute or chronic, and may present as iron deficiency ane-
verses the mesentery where the stricture will be seen. Be-
mia.Bleeding may arise anywhere in the upper-GI tract,
cause the risk of perforation is high, dilation in these cases
including the bypassed (excluded) portion of the stomach
is not adviseA review of the operative note and com-
in patients who had an RYGB. In the early postoperative
munication with the operating surgeon are helpful in
period, bleeding occurred from the anastomotic staple
knowing which type of limb delivery was used.
lines in approximately 1% to 4% of patients who under-went an RYGB.Bleeding is rare in patients who undergo
LAGB, with reported incidences as low as 0.1Pa-
Dumping syndrome is related to rapid emptying from
tients with signs or symptoms of acute or chronic bleeding
the stomach into the small bowel and does not occur after
should be evaluated with an endoscopy. Accessing the
VBG, LAGB, or DS/BPD. Symptoms may occur early
excluded portion of the stomach and the ‘‘Roux'' limb
(within 15-20 minutes) or be delayed (up to 2 hours) after
can be difficult and frequently requires the use of a colono-
a meal and include tachycardia, palpitations, diaphoresis,
scope or a double-balloon enteroscope.Recently, Shape-
flushing, diarrhea, nausea, and vomiting. The mechanism
lock technology (USGI Medical, Inc, San Clemente, Calif)
is believed to be related to rapid fluid shifts, release of va-
was used to access and evaluate the defunctionalized
soactive peptides, and fluctuations in serum glucose. The
stomacWhen traditional approaches to an endoscopy
true incidence in patients who have had bariatric surgery
in the patient with bleeding or anemia are unsuccessful,
is unknown but has been reported to be 14% in a meta-
access may be gained through a surgically created
analysis of 62 studiIndividual studies reported rates
as high as 70%.The diagnosis of dumping syndrome is
Iron deficiency is also a common feature after an RYGB,
made based upon clinical presentation, but an endoscopy
with an estimated prevalence of 30% to 50%.It has
may be considered to rule out other causes of associated
also been described with varying prevalence in patients
who have undergone DS/BPD.The mechanism ofiron deficiency is multifactorial. If GI bleeding is sus-
pected, then an appropriate workup should include endo-
Food bezoars can occur in patients who had weight-
scopic evaluation.
loss surgery, most commonly after gastric banding.They may form within the first month after surgery or
Diarrhea and nutritional deficiencies
be seen later, with symptoms of nausea, vomiting, and
Some bariatric procedures are designed to cause intes-
dysphagia.Bezoars can be diagnosed and treated by an
tinal malabsorption. A full description of the nutritional is-
endoscopy with fragmentation and reAssociated
sues in these patients is beyond the scope of this
gastrojejunal anastomotic stenoses, if present, should be
guideline. An endoscopic evaluation for symptoms of diar-
managed with dilation.
rhea or nutritional deficiencies should only be pursued ifthere is a suspicion of small-bowel mucosal disease as
Band slippage and erosion
a cause for diarrhea.
Band erosion into the gastric lumen and band slippage
In patients with diarrhea, evaluation should follow algo-
can occur after an LAGB. In a long-term study, a 9.5% rate
rithms similar to those advocated for the evaluation of pa-
of band erosion and a 6.3% rate of pouch dilatation/band
tients without a history of bariatric surgery. The role of
slippage were seen. In another study, band erosion was
endoscopy in the evaluation of diarrhea was reviewed in
identified in 11% of 75 patients with symptoBand
a separate guideline.Bacterial overgrowth can also occur
erosions are best diagnosed at an endoscopy, whereas
because of a blind loop syndrome in the excluded small
band slippage may best be diagnosed by contrast radiogra-
bowel. An empiric trial of antibiotics can be useful in
6 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 1 : 2008
Role of endoscopy in the bariatric surgery patient
patients with clinical features consistent with bacterial
gastric fistula from staple-line dehiscence, a large patulous
overgrowth and is a reasonable initial approach. In pa-
gastrojejunal anastomosis that fails to restrict food intake,
tients who do not respond to antibiotics, breath testing
or dilatation of the gastric pouch. While these may be di-
for bacterial overgrowth or endoscopic aspiration for
agnosed by contrast radiography, confirmation of the di-
quantitative bacterial culture from the excluded segment
agnosis or visualization by an endoscopy may be
should be considered. Obstruction of the excluded
desirable. Furthermore, some small gastrogastric fistula
segment can be ruled out with an endoscopy.
can be managed endoscopically.Excessively patulousgastrojejunal anastomoses were treated successfully with
Choledocholithiasis and ERCP after bypass
4-quadrant endoscopic injection of sodium morrhuate
Morbid obesity is a risk factor for gallstone formation,
into the stoma to cause scarBy using this method,
and rapid weight loss is an independent and potentially
a stomal size of %12 mm was achieved in 18 of 28
compounding risk factor. Patients who had bariatric sur-
patients (64%). Emerging technologies may allow endo-
gery have a high rate of preoperative cholelithiasis and
scopic revision of the gastrojejunal anastomosis and re-
postoperative gallstone formation. Preoperative and intra-
duction of the pouch size in patients with weight regain
operative studies indicated incidences of cholelithiasis of
27% in band candand 14% in patients with a gastricbypass, respectively.Postoperative rates of gallstone de-tection may be as high as 22% to 71%, and cholecystec-
Endoscopic treatments for obesity
tomy was required in 7% to 41% of patients who
Endoscopic therapy for morbid obesity is desirable.
underwent gastric bypass.Rates of choledocholithiasis
Currently, the endoscopic devices used for the treatment
after a gastric bypass are unknown. Whereas an ERCP
of obesity are space occupying. The first device used in
usually can be performed after gastric banding, an ERCP
the United States was the Garren-Edwards gastric bubble
in a patient with an RYGB presents significant technical
(American-Edwards Laboratories, Irvine, Calif), a 220-mL
challenges. No large series of ERCP has been published
polyurethane cylindrical device with a self-sealing valve.
in this population, and success rates of duodenal intuba-
A double-blind crossover sham study demonstrated no
tion are likely dependent on operator skill and surgical
benefit over diet and behavioral modifications.Compli-
factors, such as jejunal limb and afferent loop length.
cations included gastric erosions, ulcers, small-bowel
Both side-viewing endoscopes and forward-viewing endo-
obstruction, Mallory-Weiss tears, and esophageal lacera-
scopes have been used successfully. In the largest re-
tions.There may be a role for such devices in patients
ported series composed of 15 patients, the papilla was
who are massively obese before consideration of bariatric
reached and successfully cannulated in 66% of patients
surgery. One study found that preoperative placement of
Needle-knife sphincterotomy, sphincter of Oddi manome-
the Garren-Edwards gastric bubble induced a 10% mean
try, stone extraction, and biliary stent placement were suc-
weight loss over 3 montAnother study reported
cessfully perforIn cases that are not accessible by
that preoperative placement significantly reduced liver
standard endoscopy, laparoscopically assisted transgastric
volume, possibly facilitating an RYGB.Other endo-
ERCP was reported.In another series, percutaneous
scopic treatments are currently under investigation.
gastroenterostomy tubes were placed into the gastric rem-nant, and a pediatric duodenoscope was advanced intothe gastric remnant.Alternative means of diagnosis(eg, MRCP) and therapy (eg, percutaneous transhepatic
SUMMARY AND RECOMMENDATIONS
intervention) should be considered when treating patientswith an RYGB with choledocholithiasis. Because of the ex-
Bariatric surgical intervention presents new challenges
ceedingly high incidence of cholelithiasis and symptom-
to the endoscopist:
atic gallbladder disease after biliopancreatic diversion
An upper endoscopy should be performed in all
and a distal (extremely long) RYGB, many surgeons per-
patients with upper-GI–tract symptoms who are to
form prophylactic cholecystectomy at the time of the ini-
undergo bariatric surgery. (Level 2C)
Upper endoscopy should be considered in all patients
cholecystectomy in patients without symptoms and who
who are to undergo an RYGB, regardless of the pres-
are undergoing standard RYGB and LAGB remains contro-
ence of symptoms. (Level 3)
versial, prophylactic administration of ursodiol in these
In patients without symptoms and who are not undergo-
patient populations appears to reduce the incidence of
ing an endoscopy, noninvasive H pylori testing followed
by treatment, if positive, is recommended. (Level 3)
In patients without symptoms and who were undergo-
ing gastric banding, a preoperative upper endoscopy
Failing to lose weight or regaining weight after an ini-
should be considered to exclude large hernias that
tial weight loss may indicate the development of a gastro-
may change the surgical approach. (Level 2C)
Volume 68, No. 1 : 2008 GASTROINTESTINAL ENDOSCOPY 7
Role of endoscopy in the bariatric surgery patient
An endoscopic evaluation is useful for diagnosis and
20. Verset D, Houben JJ, Gay F, et al. The place of upper gastrointestinal
management of postoperative bariatric surgical symp-
tract endoscopy before and after vertical banded gastroplasty for
toms and complications. (Level 2C)
morbid obesity. Dig Dis Sci 1997;42:2333-7.
21. Sharaf RN, Weinshel EH, Bini EJ, et al. Endoscopy plays an important
An ERCP is difficult in patients who had an RYGB, and
preoperative role in bariatric surgery. Obes Surg 2004;14:1367-72.
an MRCP should be performed in cases where other
22. Schirmer B, Erenoglu C, Miller A. Flexible endoscopy in the
noninvasive imaging studies are inconclusive. An ERCP
management of patients undergoing RYGB. Obes Surg 2002;12:
in RYGB patients should be selectively performed.
23. Sauerland S, Angrisani L, Belachew M, et al. European Association for
Endoscopic Surgery. Obesity surgery: evidence-based guidelines ofthe European Association for Endoscopic Surgery (EAES). Surg
Abbreviations: ASGE, American Society for Gastrointestinal Endoscopy;
BMI, Body mass index; DS/BPD, duodenal switch and biliopancreatic
24. Frigg A, Peterli R, Zynamon A, et al. Radiologic and endoscopic
diversion; LAGB, laparoscopic adjustable gastric banding; RYGB,
evaluation for laparoscopic adjustable gastric banding: preoperative
Roux-en-Y gastrojejunal bypass; VBG, vertical banded gastroplasty.
and follow-up. Obes Surg 2001;11:594-9.
25. Azagury D, Dumonceau JM, Morel P, et al. Preoperative work-up in
asymptomatic patients undergoing RYGB: is endoscopy mandatory?
Obes Surg 2006;16:1304-11.
26. Feitoza AB, Baron TH. Endoscopy and ERCP in the setting of previous
1. Overweight and obesity. Available at:
upper GI tract surgery. Part I: postsurgical anatomy without alteration
Accessed February 18, 2008.
of the pancreaticobiliary tree. Gastrointest Endosc 2001;54:743-9.
2. Kuczmarski RJ, Carroll MD, Flegal KM, et al. Varying body mass index
27. Lattuada E, Zappa MA, Mozzi E, et al. Band erosion following gastric
cutoff points to describe overweight prevalence among U.S. adults:
banding: how to treat it. Obes Surg 2007;17:329-33.
NHANES III (1988 to 1994). Obes Res 1997;5:542-8.
28. Wilson JA, Romagnuolo J, Byrne TK, et al. Predictors of endoscopic
3. Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and
findings after Roux-en-Y gastric bypass. Am J Gastroenterol 2006;
obesity in the United States, 1999-2004. JAMA 2006;295:1549-55.
4. Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable
29. Sapala JA, Wood MH, Sapala MA, et al. Marginal ulcer after gastric by-
to obesity in the United States. JAMA 1999;282:1530-8.
pass: a prospective 3-year study of 173 patients. Obes Surg 1998;8:
5. Must A, Spadano J, Coakley EH, et al. The disease burden associated
with overweight and obesity. JAMA 1999;282:1523-9.
30. MacLean LD, Rhode BM, Nohr C, et al. Stomal ulcer after gastric
6. McGee DLDiverse Populations Collaboration. Body mass index and
bypass. J Am Coll Surg 1997;185:1-7.
mortality: a meta-analysis based on person-level data from twenty-
31. Nelson LG, Gonzalez R, Haines K, et al. Amelioration of gastroesoph-
six observational studies. Ann Epidemiol 2005;15:87-97.
ageal reflux symptoms following RYGB for clinically significant
7. Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in
obesity. Am Surg 2005;71:950-3.
a prospective cohort of U.S. adults. N Engl J Med 1999;341:1097-105.
32. Klaus A, Gruber I, Wetscher G, et al. Prevalent esophageal body mo-
8. Bray GA. The missing link: lose weight, live longer. N Engl J Med 2007;
tility disorders underlie aggravation of GERD symptoms in morbidly
obese patients following adjustable gastric banding. Arch Surg 2006;
9. Clinical guidelines on the identification, evaluation, and treatment of
overweight and obesity in adults-the evidence report. National Insti-
33. Foster A, Richards WO, McDowell J, et al. Gastrointestinal symptoms
tutes of Health. Obes Res 1998;6:51S-209S.
are more intense in morbidly obese patients. Surg Endosc 2003;17:
10. Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical
procedures. JAMA 2005;294:1909-17.
34. Di Francesco V, Baggio E, Mastromauro M, et al. Obesity and gastro-
11. Griffen WO Jr, Bivins BA, Bell RM. The decline and fall of the jejunoi-
esophageal acid reflux: physiopathological mechanisms and role of
leal bypass. Surg Gynecol Obstet 1983;157:301-8.
gastric bariatric surgery. Obes Surg 2004;14:1095-102.
12. Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes
35. Perry Y, Courcoulas AP, Fernando HC, et al. Laparoscopic RYGB for
recalcitrant gastroesophageal reflux disease in morbidly obese
13. Ikenberry SO, Harrison ME, Lichtenstein D, et al. American Society for
patients. JSLS 2004;8:19-23.
Gastrointestinal Endoscopy. The role of endoscopy in dyspepsia. Gas-
36. Raftopoulos I, Awais O, Courcoulas AP, et al. Laparoscopic gastric by-
trointest Endosc 2007;66:1071-5.
pass after antireflux surgery for the treatment of gastroesophageal
14. Lichtenstein DR, Cash BD, Davilla R, et al. American Society for Gas-
reflux in morbidly obese patients: initial experience. Obes Surg
trointestinal Endoscopy. Role of endoscopy in the management of
GERD. Gastrointest Endosc 2007;66:219-24.
37. Nguyen NT, Varela JE, Sabio A, et al. Reduction in prescription
15. Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the
medication costs after laparoscopic gastric bypass. Am Surg 2006;
risk for gastroesophageal reflux disease and its complications. Ann
Intern Med 2005;143:199-211.
38. Suter M, Dorta G, Giusti V, et al. Gastric banding interferes with
16. Greenstein RJ, Nissan A, Jaffin B. Esophageal anatomy and function in
esophageal motility and gastroesophageal reflux. Arch Surg 2005;
laparoscopic gastric restrictive bariatric surgery: implications for
patient selection. Obes Surg 1998;8:199-206.
39. Cobey F, Oelschlager B. Complete regression of Barrett's esophagus
17. Dolan K, Finch R, Fielding G. Laparoscopic gastric banding and crural
after RYGB. Obes Surg 2005;15:710-2.
repair in the obese patient with a hiatal hernia. Obes Surg 2003;13:
40. Westling A, Bjurling K, O
¨ hrvall M, et al. Silicone-adjustable gastric
banding: disappointing results. Obes Surg 1998;8:467-74.
18. Korenkov M, Sauerland S, Shah S, et al. Is routine preoperative upper
41. Filho AJ, Kondo W, Nassif LS, et al. Gastrogastric fistula: a possible
endoscopy in gastric banding patients really necessary? Obes Surg
complication of RYGB. JSLS 2006;10:326-31.
42. Carrodeguas L, Szomstein S, Soto F, et al. Management of gastrogas-
19. Zeni TM, Frantzides CT, Mahr C, et al. Value of preoperative upper
tric fistulas after divided RYGB surgery for morbid obesity: analysis of
endoscopy in patients undergoing laparoscopic gastric bypass.
1,292 consecutive patients and review of literature. Surg Obes Relat
Obes Surg 2006;16:142-6.
Dis 2005;1:467-74.
8 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 1 : 2008
Role of endoscopy in the bariatric surgery patient
43. Gould JC, Garren MJ, Starling JR. Lessons learned from the first 100
66. Hwang RF, Swartz DE, Felix EL. Causes of small bowel obstruction
cases in a new minimally invasive bariatric surgery program. Obes
after laparoscopic gastric bypass. Surg Endosc 2004;18:1631-5.
67. Wetter A. Role of endoscopy after Roux-en-Y gastric bypass surgery.
44. Gumbs AA, Duffy AJ, Bell RL. Management of gastrogastric fistula
Gastrointest Endosc 2007;66:253-5.
after laparoscopic RYGB. Surg Obes Relat Dis 2006;2:117-21.
68. Monteforte MJ, Turkelson CM. Bariatric surgery for morbid obesity.
45. Carucci LR, Turner MA, Conklin RC, et al. RYGB surgery for morbid
Obes Surg 2000;10:391-401.
obesity: evaluation of postoperative extraluminal leaks with upper
69. Pories WJ, Caro JF, Flickinger EG, et al. The control of diabetes
gastrointestinal series. Radiology 2006;238:119-27.
mellitus (NIDDM) in the morbidly obese with the Greenville Gastric
46. Gonzalez R, Sarr MG, Smith CD, et al. Diagnosis and contemporary
Bypass. Ann Surg 1987;206:316-23.
management of anastomotic leaks after gastric bypass for obesity.
70. Ahn LB, Huang CS, Forse RA, et al. Crohn's disease after gastric
J Am Coll Surg 2007;204:47-55.
bypass surgery for morbid obesity: is there an association? Inflamm
47. Merrifield BF, Lautz D, Thompson CC. Endoscopic repair of gastric
Bowel Dis 2005;11:622-4.
leaks after Roux-en-Y gastric bypass: a less invasive approach. Gastro-
71. Parameswaran R, Ferrando J, Sigurdsson A. Gastric bezoar complicat-
intest Endosc 2006;63:710-4.
ing laparoscopic adjustable gastric banding with band slippage.
48. Eisendrath P, Cremer M, Himpens J, et al. Endotherapy including
Obes Surg 2006;16:1683-4.
temporary stenting of fistulas of the upper gastrointestinal
72. Veronelli A, Ranieri R, Laneri M, et al. Gastric bezoars after adjustable
tract after laparoscopic bariatric surgery. Endoscopy 2007;39:625-30.
gastric banding. Obes Surg 2004;14:796-7.
49. Garcia-Caballero M, Carbajo M, Martinez-Moreno JM, et al. Drain
73. Pinto D, Carrodeguas L, Soto F, et al. Gastric bezoar after laparo-
erosion and gastro-jejunal fistula after one-anastomosis gastric bypass:
scopic Roux-en-Y gastric bypass. Obes Surg 2006;16:365-8.
endoscopic occlusion by fibrin sealant. Obes Surg 2005;15:719-22.
74. Frigg A, Peterli R, Zynamon A, et al. Radiologic and endoscopic eval-
50. Papavramidis ST, Eleftheriadis EE, Papavramidis TS, et al. Endoscopic
uation for laparoscopic adjustable gastric banding: preoperative and
management of gastrocutaneous fistula after bariatric surgery by us-
follow-up. Obes Surg 2001;11:594-9.
ing a fibrin sealant. Gastrointest Endosc 2004;59:296-300.
75. Iannelli A, Facchiano E, Sejor E, et al. Gastric necrosis: a rare compli-
51. Kriwanek S, Ott N, Ali-Abdullah S, et al. Treatment of gastro-jejunal
cation of gastric banding. Obes Surg 2005;15:1211-4.
leakage and fistulization after gastric bypass with coated self-
76. Foletto M, De Marchi F, Bernante P, et al. Late gastric pouch necrosis
expanding stents. Obes Surg 2006;16:1669-74.
after Lap-Band, treated by an individualized conservative approach.
52. Salinas A, Baptista A, Santiago E, et al. Self-expandable metal stents
Obes Surg 2005;15:1487-90.
to treat gastric leaks. Surg Obes Relat Dis 2006;2:570-2.
77. Evans JA, Williams NN, Chan EP, et al. Endoscopic removal of eroded
53. Fukumoto R, Orlina J, McGinty J, et al. Use of Polyflex stents in treat-
bands in vertical banded gastroplasty: a novel use of endoscopic
ment of acute esophageal and gastric leaks after bariatric surgery.
scissors (with video). Gastrointest Endosc 2006;64:801-4.
Surg Obes Relat Dis 2007;3:68-71.
78. Adam LA, Silva RG Jr, Rizk M, et al. Endoscopic argon plasma
54. Roberts KE, Duffy AJ, Bell RL. Laparoscopic transgastric repair of a gas-
coagulation of Marlex mesh erosion after vertical-banded gastro-
trogastric fistula after gastric bypass: a novel technique. Surg Innov
plasty. Gastrointest Endosc 2007;65:337-40.
79. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a system-
55. Merrifield BF, Lautz D, Thompson CC. Endoscopic repair of gastric
atic review and meta-analysis. JAMA 2004;292:1724-37.
leaks after RYGB: a less invasive approach. Gastrointest Endosc
80. Nguyen NT, Longoria M, Chalifoux S, et al. Gastrointestinal
hemorrhage after laparoscopic gastric bypass. Obes Surg 2004;14:
56. Torres-Villalobos G, Leslie D, Kellogg T, et al. A new approach for
treatment of gastro-gastric fistula after gastric bypass. Obes Surg
81. Rao AD, Ramalingam G. Exsanguinating hemorrhage following
gastric erosion after laparoscopic adjustable gastric banding. Obes
57. Schwartz ML, Drew RL, Chazin-Caldie M. Factors determining conver-
sion from laparoscopic to open Roux-en-Y gastric bypass. Obes Surg
82. Biertho L, Steffen R, Ricklin T, et al. Laparoscopic gastric bypass
versus laparoscopic adjustable gastric banding: a comparative study
58. Sanyal AJ, Sugerman HJ, Kellum JM, et al. Stomal complications of
of 1,200 cases. J Am Coll Surg 2003;197:536-44, discussion 544-5.
gastric bypass: incidence and outcome of therapy. Am J Gastro-
83. Sakai P, Kuga R, Safatle-Ribeiro AV, et al. Is it feasible to reach the by-
passed stomach after Roux-en-Y gastric bypass for morbid obesity?
59. Carrodeguas L, Szomstein S, Zundel N, et al. Gastrojejunal anastomotic
The use of the double-balloon enteroscope. Endoscopy 2005;37:566-9.
strictures following laparoscopic Roux-en-Y gastric bypass surgery:
84. Pai RD, Carr-Locke DL, Thompson CC. Endoscopic evaluation of the
analysis of 1291 patients. Surg Obes Relat Dis 2006;2:92-7.
defunctionalized stomach by using ShapeLock technology (with
60. Podnos YD, Jimenez JC, Wilson SE, et al. Complications after laparo-
video). Gastrointest Endosc 2007;66:578-81.
scopic gastric bypass: a review of 3464 cases. Arch Surg 2003;138:
85. Sundbom M, Nyman R, Hedenstro¨m H, et al. Investigation of the
excluded stomach after Roux-en-Y gastric bypass. Obes Surg 2001;
61. Messmer JM, Wolper JC, Sugerman HJ. Stomal disruption in gastric
partition in morbid obesity (comparison of radiographic and endo-
86. Halverson JD. Micronutrient deficiencies after gastric bypass for
scopic diagnosis). Am J Gastroenterol 1984;79:603-5.
morbid obesity. Am Surg 1986;52:594-8.
62. Escalona A, Devaud N, Boza C, et al. Gastrojejunal anastomotic
87. Amaral JF, Thompson WR, Caldwell MD, et al. Prospective hemato-
stricture after Roux-en-Y gastric bypass: ambulatory management
logic evaluation of gastric exclusion surgery for morbid obesity.
with the Savary-Gilliard dilator. Surg Endosc 2007;21:765-8.
Ann Surg 1985;201:186-93.
63. Peifer KJ, Shiels AJ, Azar R, et al. Successful endoscopic management
88. Skroubis G, Sakellaropoulos G, Pouggouras K, et al. Comparison of
of gastrojejunal anastomotic strictures after Roux-en-Y gastric
nutritional deficiencies after Roux-en-Y gastric bypass and after bilio-
bypass. Gastrointest Endosc 2007;66:248-52.
pancreatic diversion with Roux-en-Y gastric bypass. Obes Surg 2002;
64. Go MR, Muscarella P 2nd, Needleman BJ, et al. Endoscopic manage-
ment of stomal stenosis after Roux-en-Y gastric bypass. Surg Endosc
89. Dolan K, Hatzifotis M, Newbury L, et al. A clinical and nutritional com-
parison of biliopancreatic diversion with and without duodenal
65. Peifer KJ, Shiels AJ, Azar R, et al. Successful endoscopic management
switch. Ann Surg 2004;240:51-6.
of gastrojejunal anastomotic strictures after Roux-en-Y gastric
90. Eisen GM, Dominitz JA, Faigel DO, et al. Use of endoscopy in diarrheal
bypass. Gastrointest Endosc 2007;66:248-52.
illnesses. Gastrointest Endosc 2001;54:821-3.
Volume 68, No. 1 : 2008 GASTROINTESTINAL ENDOSCOPY 9
Role of endoscopy in the bariatric surgery patient
91. Kiewiet RM, Durian MF, van Leersum M, et al. Gallstone formation
bypass: a possible new option for patients with weight regain.
after weight loss following gastric banding in morbidly obese Dutch
Surg Endosc 2006;20:1744-8.
patients. Obes Surg 2006;16:592-6.
104. Meshkinpour H, Hsu D, Farivar S. Effect of gastric bubble as a weight
92. Villegas L, Schneider B, Provost D, et al. Is routine cholecystectomy
reduction device: a controlled, crossover study. Gastroenterology
required during laparoscopic gastric bypass? Obes Surg 2004;14:
105. Gostout CJ, Rajan E. Endoscopic treatments for obesity: past, present
93. Wudel LJ Jr, Wright JK, Debelak JP, et al. Prevention of gallstone
and future. Gastroenterol Clin North Am 2005;34:143-50.
formation in morbidly obese patients undergoing rapid weight
106. Alfalah H, Philippe B, Ghazal F, et al. Intragastric balloon for preoper-
loss: results of a randomized controlled pilot study. J Surg Res
ative weight reduction in candidates for laparoscopic gastric bypass
with massive obesity. Obes Surg 2006;16:147-50.
94. Puzziferri N, Austrheim-Smith IT, Wolfe BM, et al. Three-year follow-
107. Frutos MD, Morales MD, Luja´n J, et al. Intragastric balloon reduces
up of a prospective randomized trial comparing laparoscopic versus
liver volume in super-obese patients, facilitating subsequent laparo-
open gastric bypass. Ann Surg 2006;243:181-8.
scopic gastric bypass. Obes Surg 2007;17:150-4.
95. Wright BE, Cass OW, Freeman ML. ERCP in patients with long-limb
108. Schauer P, Chand B, Brethauer S. New applications for endoscopy:
Roux-en-Y gastrojejunostomy and intact papilla. Gastrointest Endosc
the emerging field of endoluminal and transgastric bariatric surgery.
Surg Endosc 2007;21:347-56.
96. Ceppa FA, Gagne DJ, Papasavas PK, et al. Laparoscopic transgastric
endoscopy after RYGB. Surg Obes Relat Dis 2007;3:21-4.
97. Martinez J, Guerrero L, Byers P, et al. Endoscopic retrograde cholan-
giopancreatography and gastroduodenoscopy after RYGB. Surg
ASGE STANDARDS OF PRACTICE COMMITTEE
Michelle A. Anderson, MD, MSc
98. Martinez J, Guerrero L, Byers P, et al. Endoscopic retrograde cholan-
giopancreatography and gastroduodenoscopy after RYGB. Surg
Robert D. Fanelli, MD, SAGES Representative
Todd H. Baron, MD, Chair
99. Mason EE, Renquist KE. Gallbladder management in obesity surgery.
Subhas Banerjee, MD
Obes Surg 2002;12:222-9.
Brooks D. Cash, MD
100. Sugerman HJ, Brewer WH, Shiffman ML, et al. A multicenter, placebo-
Jason A. Dominitz, MD, MHS
controlled, randomized, double-blind, prospective trial of prophylac-
M. Edwyn Harrison, MD
tic ursodiol for the prevention of gallstone formation following
Steven O. Ikenberry, MD
gastric-bypass-induced rapid weight loss. Am J Surg 1995;169:91-6,
Sanjay B. Jagannath, MD
discussion 96-7.
David R. Lichtenstein, MD
101. Miller K, Hell E, Lang B, et al. Gallstone formation prophylaxis
after gastric restrictive procedures for weight loss: a randomized
Kenneth K. Lee, MD, NASPGHAN Representative
Trina Van Guilder, RN, SGNA Representative
Leslie E. Stewart, RN, SGNA Representative
102. Catalano MF, Rudic G, Anderson AJ, et al. Weight gain following
This document is a product of the Standards of Practice Committee. This
bariatric surgery as a result of a large gastric stoma: endotherapy
document was reviewed and approved by the Governing Board of the
with sodium morrhuate may prevent the need for surgical revision.
American Society for Gastrointestinal Endoscopy.
Gastrointest Endosc 2007;66:240-5.
This document was reviewed and endorsed by the SAGES Guidelines
103. Thompson CC, Slattery J, Bundga ME, et al. Peroral endoscopic reduc-
Committee and Board of Governors.
tion of dilated gastrojejunal anastomosis after Roux-en-Y gastric
10 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 1 : 2008
Source: http://www.cogentixmedical.com/hubfs/original-sages_asge_role_of_endoscopy_in_bariatrics.pdf?t=1467054032615
di Giosue Carducci Letteratura italiana Einaudi Edizione di riferimento:a cura di Luigi Banfi, Mursia, Milano 1987 Letteratura italiana Einaudi Alla signorina Maria A. 1Nel chiostro del Santo 2Jaufré Rudel 3In una villa 4Piemonte 6Ad Annie 12A C. C. 13Bicocca di San Giacomo 14La guerra 20Nicola Pisano 23Cadore 26Carlo Goldoni 33A Scandiano 36Alla figlia di Francesco Crispi 37Alla città di Ferrara 39Mezzogiorno alpino 46L'ostessa di Gaby 47Esequie della guida E. R. 48La moglie del Gigante 50Per il monumento di Dante a Trento 52La mietitura del Turco 54La chiesa di Polenta 55Sabato Santo 60In riva al Lys 61Elegia del Monte Spluga 62Sant'Abbondio 64Alle Valchirie 65Presso una Certosa 67Congedo 68
JBC Papers in Press. Published on May 31, 2011 as Manuscript M111.253674 OPTOGENETIC CONTROL OF MOTOR COORDINATION BY Gi/o PROTEIN-COUPLED VERTEBRATE RHODOPSIN IN CEREBELLAR PURKINJE CELLS. Davina V. Gutierrez2, Melanie D. Mark1, Olivia Masseck1, Takashi Maejima1, Denise Kuckelsberg1, Robert A. Hyde2, Martin Krause1, Wolfgang Kruse1, and Stefan Herlitze1,2