Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Calcium hydroxylapatite associated soft tissue necrosis: a case report and treatment guideline

Calcium hydroxylapatite associated softtissue necrosis: A case report and treatmentguideline
Lauren Tracy , James Ridgway , J. Stuart Nelson Nelson Lowe , Brian Wong
a Department of Otolaryngology e Head and Neck Surgery, University of California Irvine, 101 The CityDrive, Bldg. 56, Suite 500, Orange, CA 92868, USAb Larrabee Center for Plastic Surgery, 600 Broadway, Suite 280, Seattle, WA 98122, USAc Beckman Laser Institute and Medical Clinic, University of California Irvine, 1002 Health Sciences RoadEast, Irvine, CA 92612, USAd 999 North Tustin Avenue, Suite 117, Santa Ana, CA 92705, USA
Received 28 May 2013; accepted 6 August 2013
We present an uncommon case of nasal alar and facial necrosis following calcium
Injectable filler;
hydroxylapatite filler injection performed elsewhere without direct physician supervision. The
patient developed severe full-thickness necrosis of cheek and nasal alar skin 24 h after injec-
tions into the melolabial folds. Management prior to referral included oral antibiotics, predni-
sone taper, and referral to a dermatologist (day 3) who prescribed valacyclovir for a
presumptive herpes zoster reactivation induced by the injection. Referral to our institution
Nasal alar necrosis
was made on day 11, and after herpetic outbreak was ruled out by a negative Tzanck smear,debridement with aggressive local wound care was initiated. After re-epithelialization and thefashioning of a custom intranasal stent to prevent vestibular stenosis, pulsed dye laser therapywas performed for wound modification. The patient healed with an acceptable cosmeticoutcome. This report underscores the importance of facial vasculature anatomy, injectiontechniques, and identification of adverse events when using fillers. A current treatment para-digm for such events is also presented.
ª 2013 British Association of Plastic, Reconstructive and Aesthetic Surgeons. Published byElsevier Ltd. All rights reserved.
* Corresponding author. Tel.: þ1 (949) 824 6996; fax: þ1 (949) 824 8413.
E-mail addresses: (L. Tracy).
1748-6815/$ - see front matter ª 2013 British Association of Plastic, Reconstructive and Aesthetic Surgeons. Published by Elsevier Ltd. All rights reserved.


Calcium hydroxylapatite associated soft tissue necrosis
Injectable fillers are a common, minimally invasiveapproach in the early treatment of facial aging due tovolume depletion. Use of calcium hydroxylapatite (CHA)has grown in popularity following FDA approval in 2006 toimprove moderate to severe wrinkles. Radiesse (Merz Aes-thetics, San Mateo, CA) is the CHA approved for aestheticapplications in the United States, and is composed of25e45 mm spheres suspended in a carboxymethylcellulosecarrier. Therapeutic results can be expected to last a yearor more, depending on injection location. CHA must beinjected at the dermal-subcutaneous border. If injectedsuperficially CHA can lead to nodule formation and indu-ration. Use of CHA filler in areas with a thinner dermis, suchas the nasal dorsum and tear troughs, increases the risk of
Appearance of the infarcted area after complete
inadvertent product show through the skin. Many practi-
healing and treatment with pulsed dye laser. Photograph was
tioners have noted that CHA seems to expand during the
taken 4 months after the offending injection.
first 5 min following an injection, resulting in a transientdiscomfort noted by some patients. Other common adverseevents related to filler injection include tenderness, local
erythema, and bruising. In a recent 5-year review assessingsoft tissue fillers, CHA was associated with the greatest risk
The patient was a 41-year-old woman with a past medical
of complications (2.6%), which include cellulitis, tissue
history of rhinoplasty surgery, septal perforation, and
necrosis, and nodule More severe, but less
multiple prior dermal filler injections to the melolabial
common complications include herpes zoster reactivation,
folds, who received CHA injections to both melolabial folds
arterial embolization leading to infarction, temporary
with extension to the alar-facial creases. A nurse at a local
blindness and oculomotor palsyThe most feared
"med spa" performed the injection without direct physi-
complication is vascular compromise and tissue necrosis.
cian supervision. Approximately 24 h following the injec-
Although adequate data is not available to quantify the risk
tion, the patient noted swelling and skin changes to her left
of necrosis with CHA fillers, smaller studies estimate this
alar crease. She initially sought treatment at the spa and
incidence to correlate with the known 0.001% incidence of
was treated for presumptive infection with ciprofloxacin
collagen or hyaluronic acid fillers.eThe glabellar region is
and prednisone taper. On post-injection day 3, the patient
most notoriously at risk for tissue necrosis following fillerinjection due to its reliance on the supratrochlear bloodsupply. Similarly, there have been recently reported casesof nasal alar necrosis following both CHA and hyaluronicacid injection.We present a recent case of soft tissuenecrosis of the melolabial and nasal ala region that was notaccurately identified, leading to delay in therapeuticintervention and increase in patient morbidity.
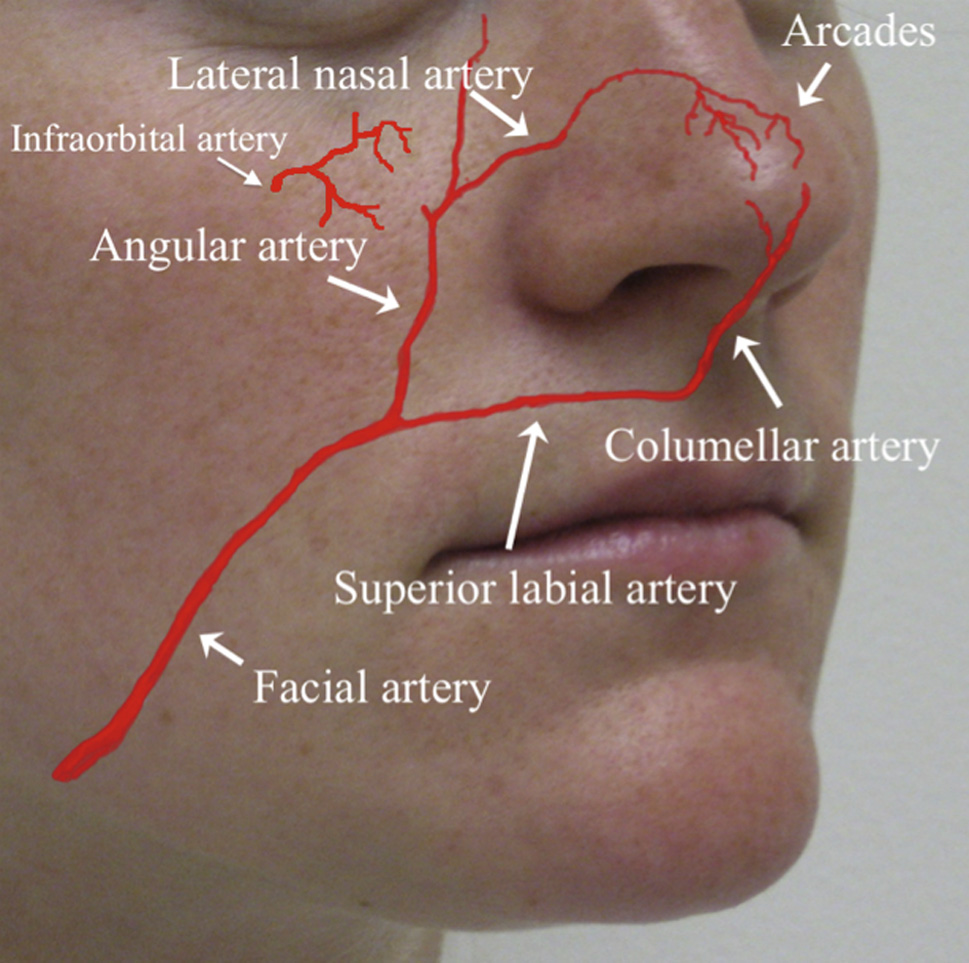
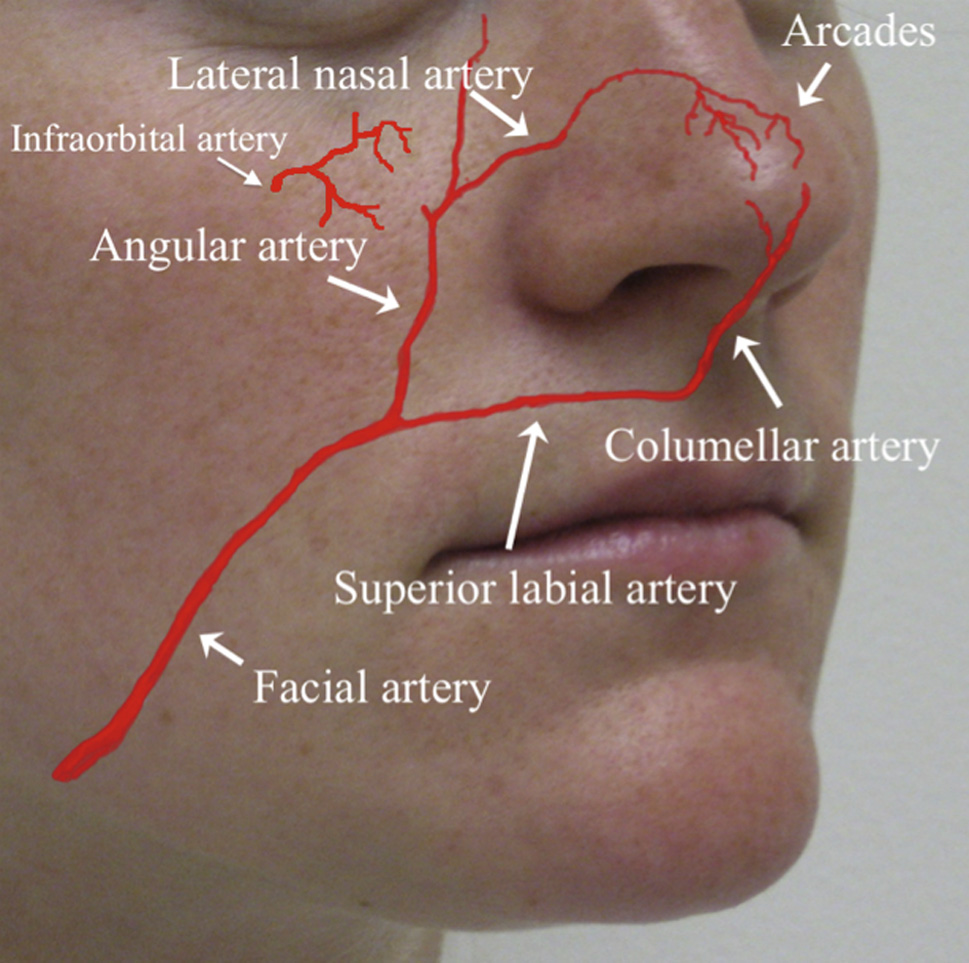
Native vascular anatomy to the nasal ala. Although
Necrosis, diffuse inflammation, and fibrinous
the infraorbital and dorsal nasal arteries provide some redun-
exudate were apparent upon presentation to our institute on
dancy, the nasal alar region receives most of its blood supply
day 11 following the filler injection.
from the angular artery.
L. Tracy et al.
developed soft tissue necrosis and was seen by a derma-
intranasal acrylic resin stent was fashioned to reduce the
tologist who prescribed valacyclovir for a presumptive
risk of cicatricial vestibular stenosis. Finally, on post-
herpes zoster reactivation induced by the injection. On
injection day 74, pulsed dye laser therapy was utilized to
post-injection day 11, the patient was referred to our
reduce scarring and hyperpigmentation. The patient healed
institution. On presentation, frank tissue necrosis, diffuse
with an acceptable result and declined additional scar
inflammation, and fibrinous exudate were observed. Gentle
revision surgery ).
debridement was performed revealing a partial thicknesstissue loss (An aggressive daily local wound careregimen was implemented and daily wound debridement
was performed. During this time herpes zoster reactivationwas ruled out with a Tzanck smear. The wound was then
Although rarely reported, nasal alar tissue necrosis is a
allowed to heal by secondary intention and a custom
known complication of injectable filler use. Tissue necrosis
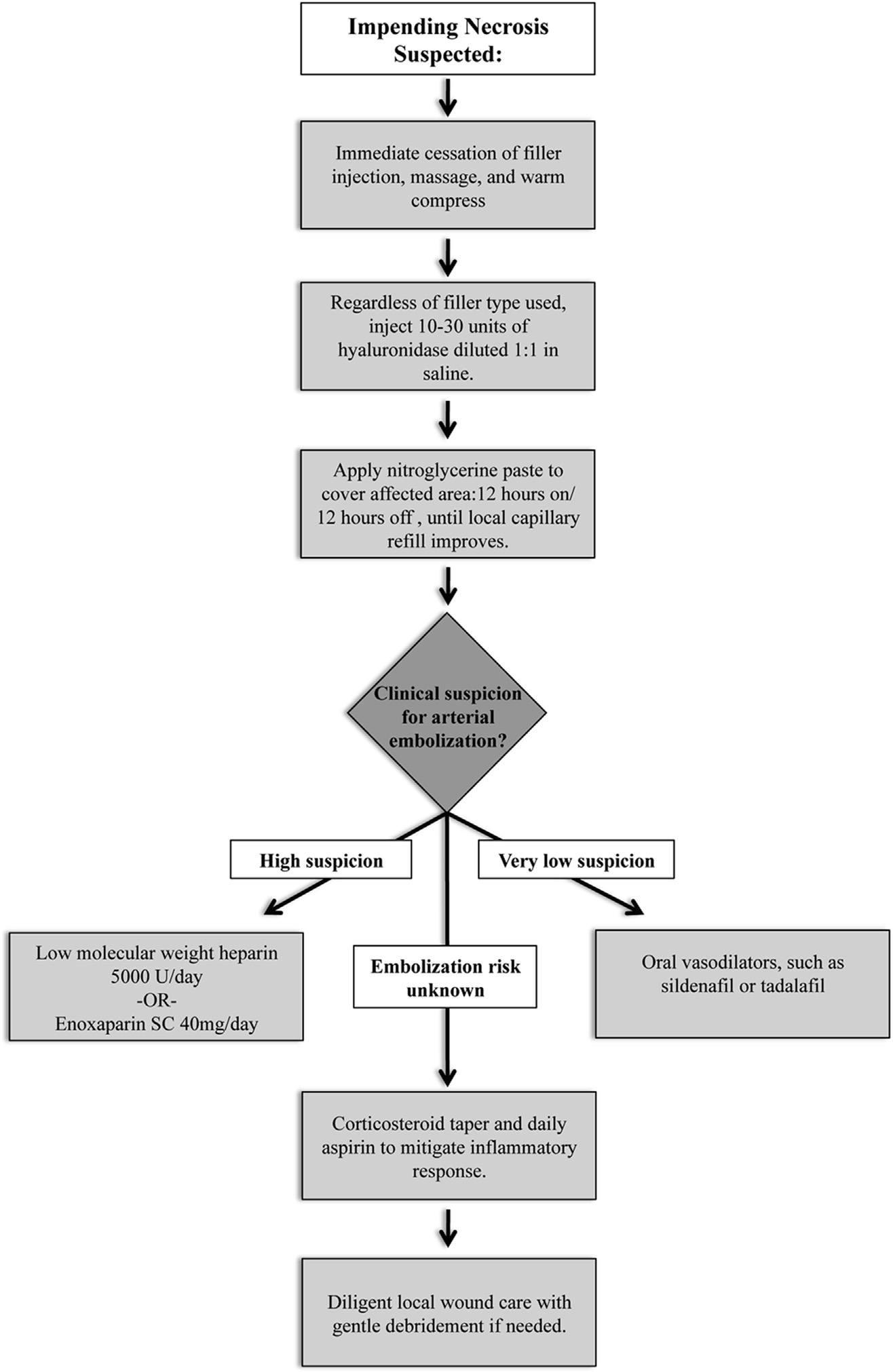
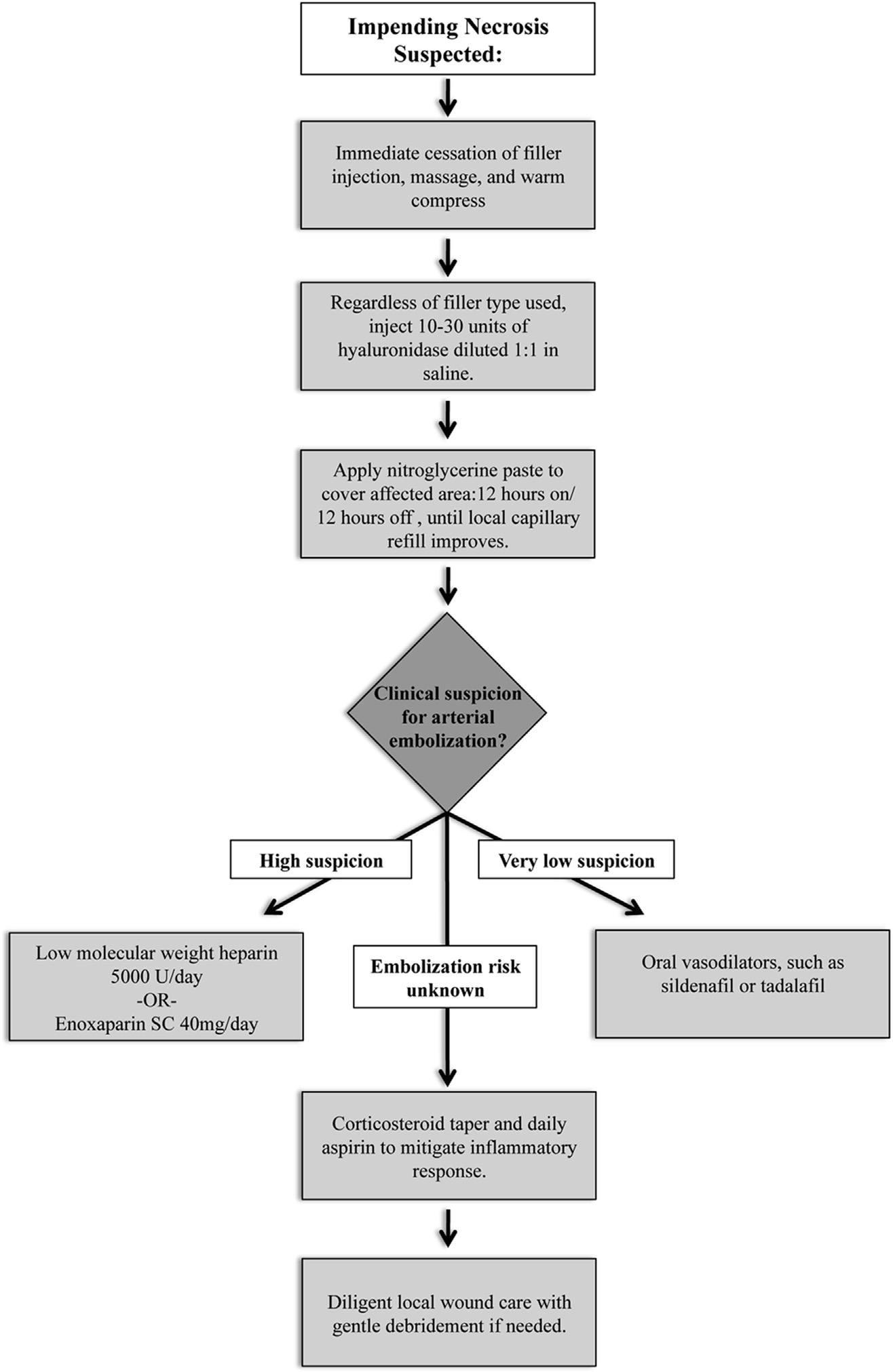
Management strategy for impending tissue necrosis associated with injection of CHA dermal filler.
Calcium hydroxylapatite associated soft tissue necrosis
can result from direct embolization of vasculature with
complete vascular occlusion and worsening necrosis. If filler
filler material or from compression of local vasculature by
embolization is suspected, low molecular weight heparin or
the filler product. The complication described in this case
enoxaparin may be useful to reduce further thrombus for-
represents an insult to the distribution of the angular
mation and minimize the extent of necrosis.
branch of the facial artery (The patient had un-dergone prior nasal surgery and it is likely that her native
vascular anatomy had been altered, leaving her nasal alarregion dependent on arcades from the superior labial and
To prevent injectable associated tissue necrosis a complete
infraorbital arteries. Given the delayed onset of symptoms
understanding of vascular anatomy, filler properties and
(approximately 24 h), arterial embolization is less likely
indications for use, as well as knowledge of the patient's
versus vascular compression. While excluded in this case, it
complete medical history is mandatory. In the circumstance
is important to consider an acute herpetic reactivation
of impending necrosis, early identification and the use of
which can mimic impending tissue Given the
appropriate vasodilatory, anti-inflammatory, and antimi-
significant morbidity and deformities associated with soft
crobial therapies is paramount to improve tissue survival
tissue necrosis, we advocate the consideration of this
and optimal wound healing. Consideration of an infectious
worst-case scenario to prevent any delay in therapeutic
or herpetic presentation should be made, but not at
the sacrifice of addressing vascular compromise. Finally,
To prevent filler associated tissue injury, a complete
custom prosthetics, such as an intranasal stent, are useful
understanding of facial vascular anatomy is necessary. In
in reducing soft tissue retraction and stenosis.
our practice, we inject only with a moving needle in aretrograde fashion and avoid large bolus injections in areasnear known vascular landmarks. We also use microcannulas
Conflict of interest
for product placement to reduce the incidence of common,transitory adverse events as well as vascular cannulization
or injuryMicrocannulas are highly flexible, have a roundblunted tip, and employ a side port for the actual injection
of filler material. Their flexibility and lack of the sharpbevel tip inherent in traditional needles make the risk of
arterial puncture with microcannulas much less likely.
Further, we feel that product placement is more accurateas a cutting needle tip creates a plane of injection while a
Appendix A. Supplementary data
microcannula follows the natural anatomic tissue planes.
If impending necrosis is suspected, or even considered,
Supplementary data related to this article can be found at
prompt treatment is absolutely mandatory (The
downside for taking action in a circumstance withoutvasculature injury is minimal in comparison to the case
example given. Current recommendations include imme-diate cessation of filler injection, prompt massage with the
intent to mechanically distribute the filler away from local
vasculature, application of a warm compress, and prompt
use of topical nitroglycerin paste to encourage vasodila-
2. Sires B, Laukaitis S, Whitehouse P. Radiesse-induced herpes
tion.The minimal amount of nitroglycerin paste needed to
zoster. Ophthal Plast and Reconstr Surg;24:218e9.
cover the affected area should be reapplied daily, 12 h on
3. Sung MS, Kim HG, Woo KI, Kim Y-D. Ocular ischemia and
and 12 h off, until local capillary refill times improve. We
ischemic oculomotor nerve palsy after vascular embolization of
recommend the use of 10e30 units hyaluronidase (Vitrase,
injectable calcium hydroxylapatite filler. Ophthal Plast and
ISTA Pharmaceuticals, Irvine, CA) diluted 1:1 in saline,
regardless of the type of filler Hyaluronan is a
known mediator of early inflammation, and hyaluronidase
has been shown to reduce edema and tissue necrosis in the
setting of myocardial infarction.Anecdotally, hyaluroni-
dase has been used successfully via the same presumptive
mechanism to mitigate inflammation and edema in cases of
necrosis related to dermal filler injection, even those using
CHA. Daily aspirin and a corticosteroid taper are used to
decrease the inflammatory component of the vascular
injury. If available, hyperbaric oxygen can also be utilized
to promote tissue oxygenation. If vascular compression
rather than filler embolus is suspected, consider the addi-
tional use of oral vasodilators such as sildenafil or tadalafil.
There is some concern that the use of vasodilatory agents in
the case of known arterial cannulization may further push
filler material into the tissue capillary bed, leading to
L. Tracy et al.
Source: http://pubs.bli.uci.edu/sites/default/files/publications/16_1.pdf
Is there a need for an expanded © 2011 Wolters Kluwer - Pharma Solutions All rights reserved, including that of translation into other languages. This booklet is protected by copyright. No part of this publication may be reproduced or transmitted in any form or by any means, electronically or mechanically, including photocopying, recording or any information storage or retrieval
Amplification of the Angiogenic Signal through theActivation of the TSC/mTOR/HIF Axis by the KSHV vGPCRin Kaposi's Sarcoma Bruno C. Jham1, Tao Ma1, Jiadi Hu1, Risa Chaisuparat1, Eitan R. Friedman1, Pier Paolo Pandolfi4, Abraham Schneider1,3, Akrit Sodhi5, Silvia Montaner1,2,3* 1 Department of Oncology and Diagnostic Sciences, School of Dentistry, University of Maryland, Baltimore, Maryland, United States of America, 2 Department of