Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Journal 2007 new
Malaysian Journal Of Dermatology
Jurnal Dermatologi Malaysia
Antibiotic Resistance Pattern of Neisseria gonorrhoeae in
Hospital Kuala Lumpur, Malaysia (2001-2005)
Azura Mohd Affandi, MBBS, MRCP, HB Gangaram, MBBS, FRCP and Suraiya H Hussein, MBBS, FRCP
Department of Dermatology, Hospital Kuala LumpurKuala Lumpur
Correspondence
Azura Mohd Affandi, MBBS, MRCP
Genito-urinary (GUM) Medicine Clinic
Department of Dermatology, Hospital Kuala Lumpur
50580 Kuala Lumpur
Email :
[email protected]
Keywords Gonorrhoea, Antibiotic Resistance Pattern
Background Gonorrhoea is the third most common sexually
transmitted infection (after syphilis and non-gonococcal urethritis)
Gonorrhoea is amongst the most common sexually
seen in patients attending the Genitourinary Medicine (GUM) Clinic
transmitted infections in the world and is caused by gram
in Hospital Kuala Lumpur (HKL). Its association with poor
negative bacterium
Neisseria gonorrhoeae. It usually infects
reproductive health outcomes and the increasing prevalence of
the mucosal surfaces, causing sexually transmitted urethritis
antimicrobial resistance has made it a major public health concern.
in men and endocervicitis in women. It can also causeanorectal and pharyngeal infections and in neonates,
Objective To determine the antibiotic resistance pattern of
Neisseria
ophthalmic infection is acquired during passage through the
Gonorrhoeae in patients attending the GUM Clinic in HKL and its
birth canal. Complications particularly affect women, and
comparison with other countries.
include salpingitis, pelvic inflammatory disease, first
Method A retrospective study of all patients with
gonorrhoea (new and
trimester abortion and decreased fertility. In men, extension
recurrent) between 2001-2005. Antimicrobial susceptibility testing by
of mucosal infection to contiguous areas may give rise to
standard disc diffusion method was performed to detect sensitivity to
epididymo-orchitis and thus reduced fertility. In a small
penicillin, tetracycline, kanamycin, ciprofloxacin, spectinomycin,
proportion of patients, gonococcaemia may occur and result
ceftriaxone and cefuroxime.
in septic arthritis, endocarditis and meningitis. It is wellrecognized that gonorrhea, together with genital ulcer
Results A total of 416 positive culture isolates of
N.gonorrhoeae from
disease, are potent amplifiers of the spread of HIV1. Rates
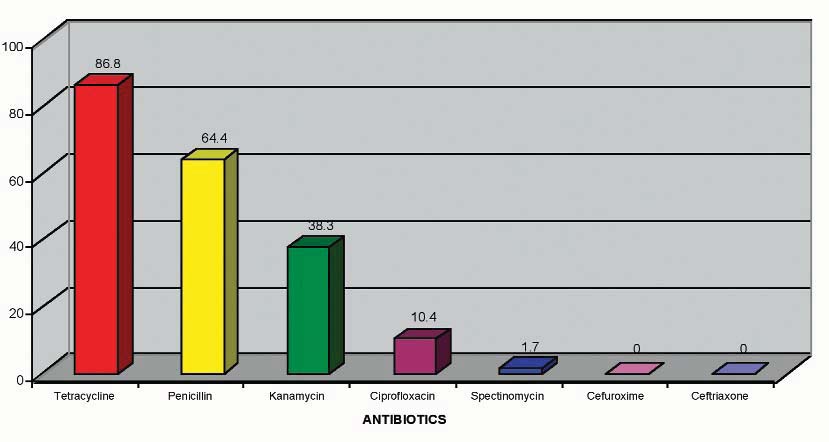
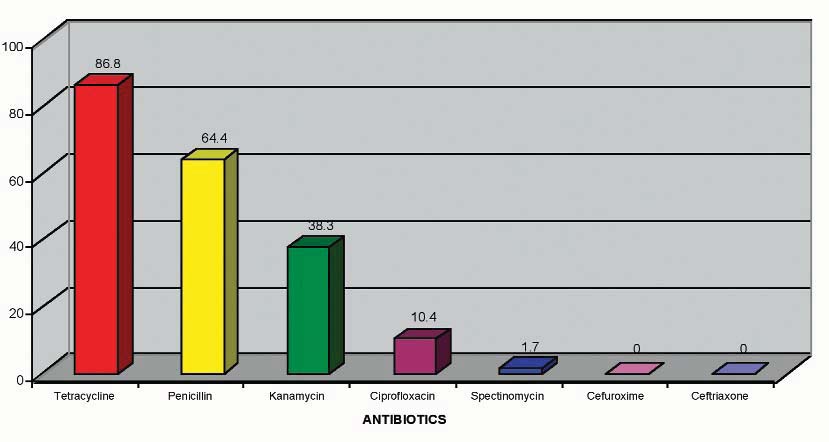
2001-2005 were reviewed. Highest level of resistance was detected to
of HIV transmission in those with gonorrhoea may be as
tetracycline (86.8% of 296 isolates). Resistance to penicillin was noted
much as 5 times more than in persons without gonorrhoea1.
in 64.4% of all isolates. Penicillinase Producing
N.gonorrhoeae (PPNG)
Those with gonorrhoea are also more susceptible to
accounted for 62% of cases. Both penicillin and tetracycline showed an
acquisition of HIV infection2.
increasing resistance trend from 2001-2005. The third commonestantibiotic resistance was to kanamycin (38.3%), followed byciprofloxacin (10.4%). The resistance to spectinomycin was 1.7%. No
Gonorrhoea remains a major global disease with an
resistance was detected to ceftriaxone and cefuroxime. All gonorrhea
estimated 60 million cases per year globally, making it a
patients in GUM Clinic, HKL were treated with ceftriaxone, and
major public health concern3. About half of these cases
subsequent cultures on follow-up were negative. We compared our
occur in the Western Pacific and South East Asia regions5.
results with the data obtained from the Gonococcal Resistance to
In GUM Clinic, HKL, gonorrhoea accounts for the third
Antimicrobials Surveillance Programme (GRASP)6 and the WHO
most common sexually transmitted infection (after syphilis
Western Pacific Gonococcal Antimicrobial Surveillance Programme
and non-gonococcal urethritis). In the recent years,
incidence of gonorrhoea has also increased in otherdeveloped countries, with the highest rates in the socially
Conclusion Penicillin and tetracycline resistance remain high in
and economically deprived subpopulations, and in
Malaysia and other Western Pacific countries. Resistance to
homosexual men4.
ciprofloxacin was however lower in Malaysia compared to othercountries. There was no resistance to ceftriaxone and cefuroxime. Thecurrent first line antibiotic for treating gonorrhoea in GUM Clinic,HKL is ceftriaxone.
Malaysian Journal Of Dermatology
Jurnal Dermatologi Malaysia
Attempts to treat and control gonorrhoea are compromised
Table 1. Positive culture isolates of N.gonorrhoeae
by the emergence and spread of antibiotic resistant
Neisseria
Number of isolates
gonorrhoeae. There are many surveillance programmes onantibiotic resistance pattern of N.gonorrhoeae such as
GRASP (Gonococcal Resistance to Antimicrobial
Surveilance Programme), which is based in London, UK
and WHO WPR GASP (World Health OrganizationWestern Pacific Region Gonococcal Antimicrobial
Surveilance Programme)5, 6. Tetracycline resistance is
encountered in many countries. Since penicillin resistance
emerged in the late 1970's, it has spread to most parts of theworld7. This is either due to Penicillinase Producing
Neisseria gonorrhoeae (PPNG) or chromosomally mediated
Majority of the patients (51.7%) were between the ages of
resistance (CMRNG). South East Asian countries are
21-30 years old (Figure 1). 96.6% were males and 3.4%
noted to have high PPNG rates7. Resistance to quinolones
females. The majority of the patients were Malays (63.7%),
was first observed in the South East Asia and the Western
followed by Indian (23.6%), Chinese (8.9%) and others(3.8%). (Racial distribution of patients attending the GUM
Pacific regions in the 1990's, and have now spread widely
Clinic, HKL from 2001-2005 : Malay-44.7%, Indian-25.3%
within and beyond the Western Pacific Regions8. There
Chinese-18.6% and Others-11.4%).
were also reported cases of altered susceptibility to thirdgeneration cephalosporin in the Western Pacific Region9, 10and recently these strains have also appeared in centresoutside the region. Antibiotic resistance pattern vary
Materials and methods
between different geographical areas. Therefore, it is
This is a retrospective study of all patients with gonorrhoea
important to know the local antibiotic resistance pattern, so
(new and recurrent), attending the GUM Clinic, HKL
that appropriate treatment can be instituted. In HKL,
between 2001-2005. Antimicrobial susceptibility testing by
kanamycin was used during the early 1970's and 80's, which
standard disc diffusion method was performed to detect
was subsequently changed to spectinomycin, followed by
resistance to penicillin,
ceftriaxone since the early 1990's.
ciprofloxacin, spectinomycin, ceftriaxone and cefuroxime.
All information was obtained from patients' case notes.
Objectives
To determine the antibiotic resistance pattern of
N.gonorrhoeae in patients attending the GUM Clinic, HKL
A total of 416 positive culture isolates of Neisseria
and to compare it with other countries.
gonorrhoeae from 2001-2005 were reviewed. The number
of isolates for each year is shown in
Table 1.
Figure 1. Age of patients with gonorrhoea (n=416)
Malaysian Journal Of Dermatology
Jurnal Dermatologi Malaysia
Table 2. Summary of antibiotic resistance pattern of N.gonorrhoeae (2001-2005)
Year / Antibiotics
Figure 2. Antibiotic resistance pattern of N.gonorrhoeae (2001-2005)
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Figure 3. Overall antibiotic resistance pattern of N.gonorrhoeae (2001-2005)
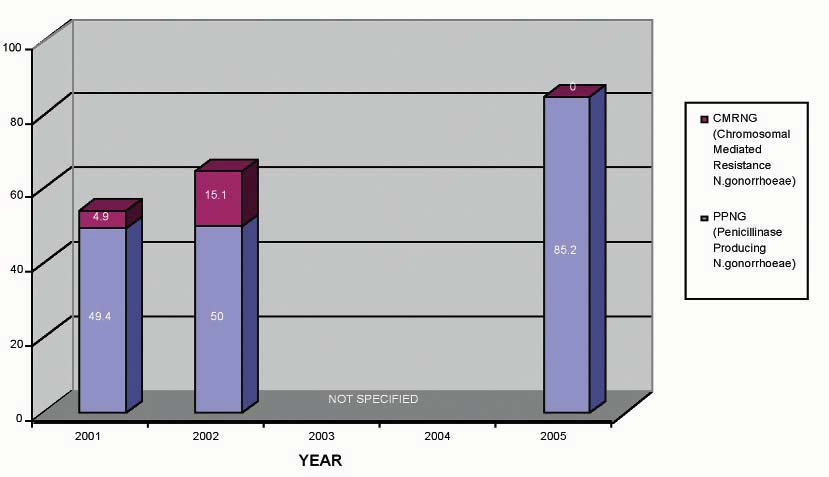
Figure 4. Resistance of N.gonorrhoeae to Penicillin
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Table 3. Comparison of N.gonorrhoeae antibiotic resistance pattern in Hospital Kuala Lumpur (HKL)
with other countries
Country / Centre
% Penicillin Resistant
England and Wales6
7The WHO Western Pacific Gonococcal Antimicrobial Surveilance Programme (GASP) 20046The Gonococcal Resistance to Antimicrobials Surveilance Programme (GRASP) 2004
Antibiotic resistance pattern of
Ciprofloxacin is not the first line treatment for gonorrhoeain our clinic. However, it is used by the primary care doctors
for treating gonorrhoea due to its accessibility and ease of
Tetracycline has never been used for treating gonorrhoea in
administration. Susceptibility testing to ciprofloxacin was
HKL as the resistance is very high. Nevertheless, the
done since 2002. There was a gradual increase from 8.7% in
resistance pattern is continuously monitored for
2002 to 12.5% in 2005 (Table 2 and Figure 2). The overall
epidemiological purposes. In 2002, 57.4% of the isolates
resistance rate from 2001-2005 is 10.4% (Figure 3).
were resistant to tetracycline and the levels have continued
to rise, reaching 100% in 2004 (Table 2 and Figure 2). The
overall tetracycline resistance from 2001-2005 is 86.8%
Spectinomycin showed a low resistance rate of 1.2% in 2001
(Figure 3).
and 2.3% in 2002 (Table 2 and Figure 2). The susceptibility
testing was discontinued in 2003. The overall resistance to
spectinomycin from 2001-2005 is 1.7% (Figure 3).
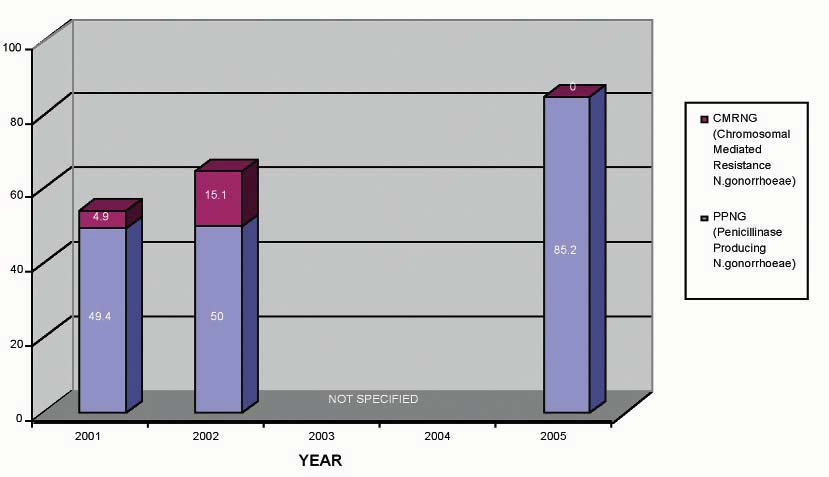
Resistance to penicillin also showed an increasing trend
from 54.3% in 2001 to 85.2% in 2005 (Table 2 and Figure
6. Cephalosporins - Cefuroxime and Ceftriaxone
2). The overall resistance rate from 2001 to 2005 is 64.4%
Susceptibilty of N.gonorrhoeae to cefuroxime was tested in
(Figure 3). This can be due to Penicillinase Producing
2001 and 2002. None of the isolates were found to be
N.gonorrhoeae (PPNG) or Chromosomal Mediated
resistant to cefuroxime. Similarly, since 2001 to 2005, none
Resistance N.gonorrhoeae (CMRNG) (Figure 4). Of the
of the N.gonorrhoeae isolates were found to be resistant to
isolates resistant to penicillin, 62% were PPNG and 6.7%
ceftriaxone (Table 2, Figure 2 and Figure 3). All patients in
our clinic were treated with ceftriaxone and subsequentcultures on follow-up were negative.
3. Kanamycin
Kanamycin was used for treating gonorrhoea in HKL in the
early 1970's and 80's. However, because of increasing
44.3% of the N.gonorrhoeae isolates were found to be
resistance since the early 1990's, it is not used anymore.
resistant to both penicillin and tetracycline. 5.1% of the
Resistance of N.gonorrhoeae to kanamycin was done in 2001
isolates were resistant to all 3 antibiotics-penicillin,
and 2002 only. There was a marked increase in the
tetracycline and ciprofloxacin.
resistance pattern from 13.6% in 2001 to 89.7% in 2002
(Table 2 and Figure 2). The overall resistance to kanamycin
from 2001 to 2005 is 38.3% (Figure 3).
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
The summary of N.gonorrhoeae antibiotic resistance pattern
Surveillance of antibiotic resistance in Neisseria gonorrhoeae
from 2001 to 2005 is illustrated in Table 2 and Figure 2.
in the WHO Western Pacific Region, 1998. Commun Dis Intell
The overall (average) antibiotic resistance pattern from
Tapsall JW. Antibiotic Reistance in Neisseria gonorrhoeae. Clin
2001-2005 is shown in Figure 3.
Infect Dis 2005;41:S263-268.
GRASP Steering Group. The Gonococcal Resistance to
Antimicrobials Surveillance Programme (GRASP) Year 2004
Attempts to treat and control gonorrhoea are compromised
report. London: Health Protection Agency 2005.
by the emergence and spread of antibiotic-resistant N.
The WHO Western Pacific Gonococcal Antimicrobial Surveillance Programme. Surveillance of antibiotic resistance in
gonorrhoeae. WHO expert committee has recommended
Neisseria gonorrhoeae in the WHO Western Pacific Region,
that treatment regimens be altered once resistance to a
2004. Commun Dis Intell 2006;30:129–132.
particular antibiotic reaches 5 percent.11 Penicillin and
WHO Western Pacific Region Gonococcal Antimicrobial
tetracycline resistant N.gonorrhoeae remain high in Malaysia
Surveillance Programme. Surveillance of antibiotic susceptibility of Neisseria gonorrhoeae in the WHO Western
and other Western Pacific countries and the resistance rate
Pacific Region 1992–4. Genitourin Med 1997;73:355–361.
continue to increase. Resistance to ciprofloxacin was
The WHO Western Pacific Gonococcal Antimicrobial
however lower in Malaysia compared to other countries.
Surveillance Programme. Surveillance of antibiotic resistance in
However, the level is gradually increasing and has to be
Neisseria gonorrhoeae in the WHO Western Pacific Region,
monitored closely. Current first line antibiotic for treating
2001. Commun Dis Intell 2002;26:541–545.
The WHO Western Pacific Gonococcal Antimicrobial
gonorrhoea in GUM Clinic, HKL is ceftriaxone, which has
Surveillance Programme. Surveillance of antibiotic resistance in
no documented resistance so far.
Neisseria gonorrhoeae in the WHO Western Pacific Region, 2000. Commun Dis Intell 2001;25:274-276.
Guidelines for the management of sexually transmitted
We would like to convey our special gratitude to Dr Akbal
infections WHO/HIV-AIDS. Geneva: World Health Organization; 2001. Report No.WHO/RHR/01.10. Available online.
Kaur, Encik Othman Thani and other staff from the
Genitourinary Medicine Clinic, HKL for data collection.
/who_hiv_aids_2001.01/
Ito M, Deguchi T, Mizutani KS, Yasuda M, Yokoi S, Ito S et al. Emergence and spread of Neisseria gonorrhoeae clinical
isolates harbouring mossaic-like structure of penicillin-binding protein 2 in Japan. Antimicrob Agent Chemother 2005;49:137-
Cohen MS. Sexually transmitted diseases enhance HIV
transmission: no longer a hypothesis. Lancet 1998;351
Tapsall JW. Annual Report of the Australian Gonococcal
(Suppl III):5-7.
Surveilance Programme, 2004. Commun Dis Intell 2005;29:136-
Cohen MS, Hoffman IF, Royce RA et al. Reduction of
concentration of HIV-1 in semen after treatment of urethritis:
Wang SA, Lee MV, O'Connor N, Iverson CJ, Ohye RG, Whiticar
implications for prevention of transmission of HIV-1. Lancet
PM et al. Multidrug-resistant Neisseria gonorrhoeae with
decreased susceptibility to cefixime - Hawaii, 2001. Clin Infect
Gerbase AC, Rowley JT, Heyman DHL, Berkley SFB, Piot P.
Global prevalence and incidence estimates of selected curable STDs. Sex Transm Inf 1998;74 (suppl 1):S12-S16.
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
A 10-year Retrospective Study on Changing Pattern
of Sexually Transmitted Infections in
Hospital Kuala Lumpur, Malaysia
Penny Lim, MBBS, MRCP, HB Gangaram, MBBS, FRCP and Suraiya H Hussein, MBBS, FRCP
Genito-Urinary Medicine (GUM) ClinicDepartment of Dermatology, Hospital Kuala Lumpur 50580 Kuala Lumpur
Correspondence
Dr Penny Lim Poh Lu, MBBS, MRCP
Department of Dermatology, Hospital Kuala Lumpur
50580 Kuala Lumpur
Email : [email protected]
which remained unchanged in both the study periods. Based onethnicity, there was an increase in the percentage of Malays being
Background Sexually transmitted infections (STIs), and HIV
infected in STIs in the later study period. Syphilis was the commonest
especially, are a major health problem in Malaysia. The emergence of
STI seen in both the study periods. The second commonest STI seen
HIV infection has increased the importance of early and effective
in 1995-1999 was gonorrhoea and non-gonococcal urethritis (NGU).
treatment of STIs as any delay may lead to enhance transmission or
In 2005, there were 184 patients with syphilis; 64% were heterosexuals;
acquisition of HIV infection. A proper understanding of the patterns
39.6% homosexuals and 1.6% bisexuals. Majority (82%) were
of STIs is necessary for effective planning and control strategies. The
asymptomatic (latent syphilis with positive syphilis serology at
present study is designed to determine the changing pattern of STIs in
presentation. Symptomatic patients with early infectious syphilis
the Genito-urinary Medicine Clinic (GUM), Hospital Kuala Lumpur
constituted 15% (Primary 8%; Secondary 7%). Screening for HIV was
positive in 31 (16.8%) patients. HIV infection was noted to be thecommonest STI associated with syphilis.
Objective To study the sociodemographic characteristics of patients
with STIs attending the GUM Clinic in HKL and to analyze any
Conclusion was an overall decline in the number of patients with
changes in the pattern of STIs seen between the 2 study periods of
STIs attending the GUM clinic, HKL. The decline was more evident
1995-1999 and 2001-2005.
with bacterial STIs; viral STIs however showed an increasing trend.
Syphilis was still the commonest STI seen in the two study periods
Method A retrospective review of case notes of new patients with
although the percentage has declined. Non specific urethritis has
STIs attending the GUM clinic, HKL was done during two study
superseded gonorrhoea as the second commonest STI. HIV was found
periods of 1995-1999 (Poster presentation on "Pattern of STDs" at
to be the commonest STI seen in association with syphilis.
14th RCD, Asia-Australasia, 26-30 July 2000, KL, Malaysia by HBGangaram et al) and 2001-2005.
Keywords Changing pattern, Sexually transmitted infections, STI
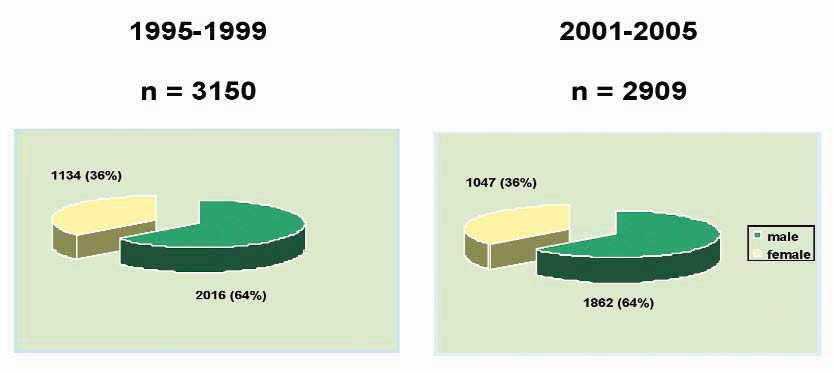
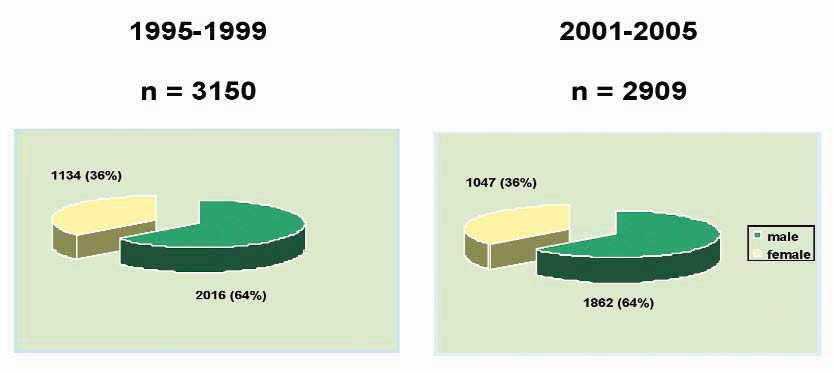
Results In 1995-1999, a total of 3150 STI patients were studied.
Among them, 2016 (64%) were males and 1134 (36%) were females. In
Nearly one million new people are infected with sexually
2001-2005, a total of 2909 STI patients were examined, of which 1862
transmitted infections (STIs) every day nationwide. World
(64%) were males and 1047 (36%) were female. There was a decrease
Health Organization (WHO) estimated that approximately
of 8.3% in the total number of cases seen in 2001-2005 as compared to
340 million new cases of the four main curable STIs
1995-1999. The decline was more evident with bacterial STIs which
gonorrhoea, NGU, syphilis and trichomoniasis occur every
included syphilis, gonorrhoea, NGU and chancroid. Viral STIs which
year2,13. STIs are responsible for an enormous burden on
consisted of herpes genitalis, genital warts and HIV showed an
morbidity and mortality in many developing countries
increasing trend.
because of their effects on reproductive and child health and
A younger age group (20-39 years old) appeared to be infected with
STIs in 2001-2005. Males outnumbered females in the ratio of 1.8:1,
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
their role in facilitating the transmission of HIV infection.
The emergence of HIV infection has increased the
This study included a total of 2909 patients in 2001-2005
importance of measures aimed at control of STIs. A proper
as compared to 3150 patients in 1995-1999 (Table 1).
understanding of the patterns of STIs prevailing in different
There was a decrease of 8.3% in the total number of cases
geographic regions of a country is necessary for proper
seen in 2001-2005.
planning and implementation of STI control strategies4. Itis with this aim that the present study was undertaken.
Majority of the patients (51.7%) were between the ages of30-49 years old in 1995-1999. In the present study, a
younger age group between 20-39 years old appear to be
To study the sociodemographic characteristics of patients
infected with STIs1,2,3,4,9,10 as shown in Figure 2. 64% were
with STIs attending the Genitourinary Medicine Clinic
males and 34% females in both the study periods. In 1995-
(GUM), Hospital Kuala Lumpur and to analyze any
1999, Malay comprised the majority of the patients (38%),
changes in the pattern of STIs seen between the 2 study
followed by Indian (22%), Chinese (17%), foreigners (18%)
periods of 1995-1999 and 2001-2005.
and others (5%). In 2001-2005, there is was increase in thepercentage of Malays (47.8%) being infected with STIs,
Materials and Methods
followed by Indian (21.4%), Chinese(18.9%), foreigners
This is a retrospective review of case notes of new patients
(8.0%) and others (3.9%) (refer Figure 2). (Ethnic
with STIs attending the GUM Clinic, HKL during two
Distribution of Patients Attending the GUM Clinic, HKL from
study periods of 1995-1999 and 2001-2005. The National
2001-2005 : Malay-44.7%, Indian-25.3% Chinese-18.6%
Statistics figures were obtained from the Department of
Public Health, Malaysia.
Table 1. Classification of Syphilis in GUM Clinic 2005 (n=184)
Figure 1. Total number of new patients with STI in GUM
Figure 2. Age distribution of new patients with STI
Age group (Age)
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Figure 3. Sex distribution of new patients with STI
Figure 4. Ethnic distribution of new patients with STI
Syphilis was the commonest STI seen in both the study
commonest STI seen in 1995-1999 was gonorrhoea and
periods although there was a decline from 982 (31.2%) to
non-gonococcal urethritis (NGU) in the present study
702 (24.1%) (Figure 5). In 2005, there were 184 patients.
(Figure 5). Generally, there was an overall decrease in
118 (64.1%) were heterosexual, 73 (39.6%) homosexuals
bacterial STI (syphilis, gonorrhoea, NGU and chancroid)
and 3 (1.6%) and 3 (1.6%) bisexuals (Figure 7). Majority
with an increase in viral STI (genital warts, genital herpes
(82%) were asymptomatic (latent syphilis with positive
and HIV)1,4,8,9 Figure 6.
syphilis serology at presentation (Table 1). The second
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Figure 5. Types of STIs between 1995-1999 and 2001-2005
ypes of STIs
T
Figure 6. Comparison between Bacterial STI and Viral STI
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Figure 7. Syphilis in GUM Clinic, HKL 2005 (n=184)
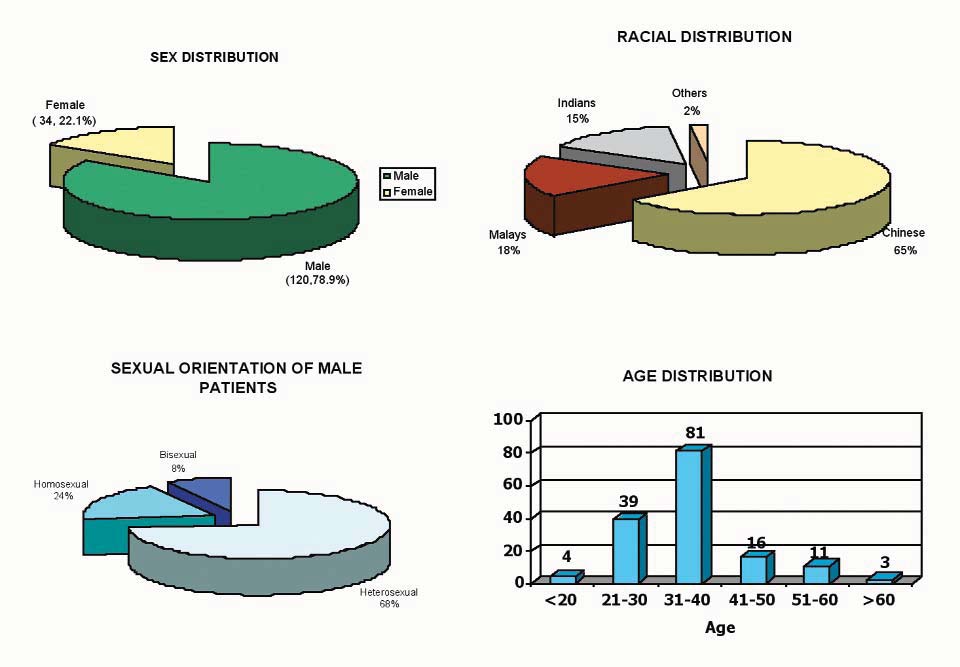
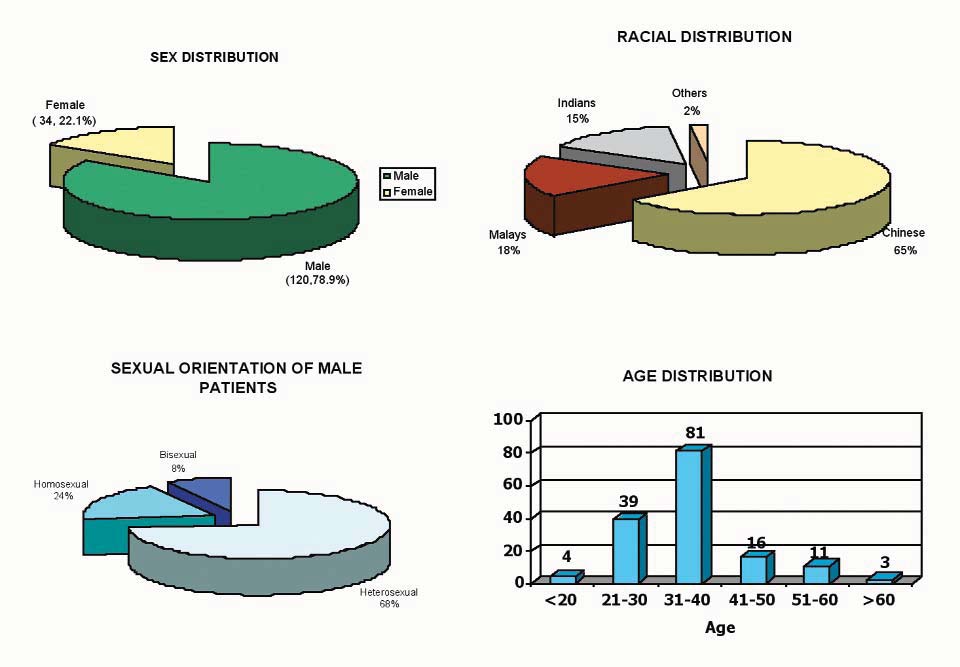
HIV seropositivity was 5.3% of all clinic attendes during 2001-2005. Of these 78 % were males and 22% females. 68 %were homosexuals, 24% heterosexuals and 8% bisexuals in HIV male patients. Chinese comprised the majority of patients(65%) followed by Malays (18%), Indian (15%) and others (2%). Majority of patients were in the age group 21-40 yearsold which is also the most sexually active age group.
Figure 8. HIV patients in GUM Clinic, HKL 2001-2005 (n=154)
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
This study demonstrated an overall decline in the total
There was an overall decline in the total number of patients
number of STI cases1,4,8.9. The total number of patients with
with STIs attending the GUM Clinic, HKL. The decline
bacterial STIs such as syphilis, chancroid and gonorrhoea
was more evident with bacterial STIs; viral STIs however
also showed a declining trend. However there was an
showed an increasing trend. Syphilis was still the
increase in viral STIs like HIV, herpes genitalis and genital
commonest STI seen in the two study periods although the
warts. This is similar to the findings in other studies. This
percentage has declined. NGU has superseded gonorrhoea
decline in the number of patients with STIs attending the
as the second commonest STI. HIV was found to be the
GUM clinic could be attributed to either a true decline in
most common STI seen in association with syphilis.
STIs with the onset of HIV more commonly patientsseeking treatment at private general practitioner (GP)
clinic, expecting more confidentiality in dealing with these
We would like to convey our special gratitude to Dr Akbal
diseases. Awareness and fear of contracting HIV have
Kaur, Encik Abdul Manaf B. Yusoff and other staff from
influenced the risk-taking behaviour of people, thereby
Genitourinary Medicine Clinic, HKL for data collection.
reducing the likelihood of being infected with STIs.
In the present study, males outnumbered females by 1.8:1.
This pattern of male preponderance is also seen in other
Krishna Ray et al; Changing trends in sexually transmitted
studies1,4,8,9. Of particular interest, the age group with the
infections at a Regional STD Centre in north India; Indian J Med
highest number of cases has shifted to a younger age11,14 (20-
39 years old ). This is not surprising as the average age for
WHO Europe; Trends in sexually transmitted infections and HIV
sexual debut nowadays occurs earlier. Factors that could
in the European Region, 1980-2005; technical briefing document
contribute to this include increasing exposure to sex
01B/06, Copenhagen, 12 September 2006.
Sevgi O. Aral et al; Sexually Transmitted Infections and HIV in
periodicals, advertisements, the theater, radio, television and
the Southern United States: An Overview; Sexually Transmitted
the internet. This group are at a high risk of being
Diseases; July (suppl) 2006;33(7):1-5.
behaviourally more vulnerable to STI acquisition, as they
Narayanan B; A retrospective study of the pattern of sexually
generally have a higher number of sexual partners and more
transmitted diseases during a ten-year period; IJDVL 2005;71(5):333-7.
concurrent partnerships and change partners more often
Kevin A. Fenton et al; Reported Sexually Transmitted Disease
than older age groups. Being the economically productive
Clinic Attendance and Sexually Transmitted Infections in Britain:
group, there is great loss of workforce due to STI morbidity,
Prevalence, Risk factors and Proportionate Population Burden;
measured as disability adjusted life years (DALYS)1 lost.
The Journal of Infectious Diseases 2005;191(Suppl 1):127-38.
Although the teenagers were not spared, the percentage of
Christopher J. Smith; Social geography of sexually transmitted diseases in China; Asia Pacific Viewpoint; April 2005;46(1):65-80.
STI cases was not high. Nevertheless the young adults and
E.N. Nnoruka and A.C.J.Ezeoke; Evaluation of syphilis in patients
adolescents should constitute the priority target group in
with HIV infection in Nigeria; Tropical Medicine and
STI control programme.
International Health; Jan 2005;10:58-64.
Abdul Wahab Al-Fouzan and Nawaf Al- Mutairi; Overview of
The disporportionate attendance of Chinese patients could
Incidence of Sexually Transmitted Diseases in Kuwait; Clinics in Dermatology; 2004; 22:509-512.
be their preference for seeking treatment from GP clinics as
Sharma VK, Khandpur S.; Changing patterns of sexually
compared to government hospitals/ clinics.
transmitted infections in India, Natl Medical Journal India;2004;17(6):310-319.
Syphilis is the commonest STI seen in both the study
Jaswal AK et al; Changing trends in Sexually transmitted diseases in North Eastern India; IJDVL2002;68(2):65-66.
periods although there is a decline. Of the different types,
Hiok-Hee Tan, Roy Chan; Sexually transmitted infections in
latent syphilis was the most common. The second
Singapore Youths; National Skin Centre, Singapore 2005.
commonest STI seen in 1995-1999 was gonorrhoea whilst
William K.Bosu; Syndromic management of sexually transmitted
in the present study it was non-gonococcal urethritis
diseases; Tropical Medicine and International Health ; February
(NGU). This pattern change was also seen in most
WHO, Office of Information; Sexually transmitted infections
countries. HIV was the commonest STI seen in association
increasing- 250 million new infections annually,1990;(152):1-6.
with syphilis. Syphilis increases the risk of both
Donald WH; The changing pattern of sexually transmitted
transmitting and getting infected with HIV and can be
diseases in adolescents; Practitioner;1979; 222(1329):383-5.
harder to cure and may progress more quickly and severely
Raval RC et al; A study of a changing patterns of sexually transmitted diseases and HIV prevalence during intervals of
in people infected with HIV2. However, further studies are
different years; International Conference AIDS July 7-12,
required to confirm this association.
2002;14: Abstract No. C10895
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Allergic Contact Dermatitis in a private practice
Dermatology Clinic in Ipoh: A Seven-Year Retrospective
Study
Henry BB Foong, MBBS, FRCP1, Elizabeth M Taylor, MBBS1 and N Ibrahim2
1Foong Skin Specialist Clinic33A Persiaran Pearl, Fair Park, Ipoh 31400, Malaysia2Medical Student (Phase 3A), Universiti Kuala Lumpur RoyalCollege of Medicine Perak, Ipoh, Malaysia
Correspondence
HBB Foong, FRCP,
Foong Skin Specialist Clinic
33A Persiaran Pearl, Fair Park, Ipoh 31400, Malaysia
Email : [email protected]
recorded. All were patch tested to the NSC standard battery
Patch testing has been accepted as the most important investigative
(Chemotechnique) and additional allergens where
technique of assessing allergic contact dermatitis (ACD) and
indicated. The test allergens were mounted on Scanpore
identifying the contact allergens. The epidemiology of ACD differs in
tape. The allergens were removed at 48 hours and reaction
different geographic region as the environmental allergens vary in
recorded 15 minutes after removal. The reactions were
different populations. In this study 59.8% of the patients had a positive
recorded again at 96 hours.
patch test reaction to one or more allergens. The prevalence of ACDwas 64.7% in women and 51.4% in men. The commonest causes of
Reactions were recorded according to the standard scoring
ACD were nickel (30.4%), fragrance mix (18.16%) and balsam of Peru
system recommended by International Contact Dermatitis
Research Group. NR = nonreactive; +/- = erythema; + =erythema with papules; ++ = palpable erythema, papules and
Keywords contact dermatitis, prevalence, patch tests
vesicles; +++ = palpable erythema, vesicles, bullae; IR =irritant reactions. Reactions of + and greater were
considered positive. The prevalence of ACD (patients with
Patch testing has been accepted as the most important
one or more positive reactions) was evaluated.
investigative technique of assessing allergic contactdermatitis (ACD) and identifying the contact allergens1
The epidemiology of ACD differs in different geographic
During the study period, 317 women and 173 men were
region as the environmental allergens vary in different
patch tested. The age ranged from 6-86 years with a mean
populations. A study done in Hospital Kuala Lumpur using
of 37.5 years. The prevalence of contact dermatitis was
the European standard allergens for the period 1994-1996
64.7% (205/317) in women and 51.4% (89/173) in men.
showed the top three allergens to be nickel (36%), rubberchemicals (19%) and fragrance mix (17%) while in
Table 1 shows the prevalence of positive reaction according
Singapore nickel (13.9%), fragrance mix (8.4%), flavine
to age and sex. Most were in the 20-29 years age group.
(6.3%) and potassium dichromate (6.3%)2,3. The prevalence
The rate appeared to increase with age. For those less than
of ACD in 2471 patients patch tested in Singapore was
40 years old it was 58.2% (174/299) and more than 40 years
49.2% in women and 49.8% in men3. The epidemiology of
62.8% (120/191).
ACD in a private practice dermatology clinic has not beenwell documented. This is an epidemiologic study of ACD of
Table 2 shows the prevalence of contact dermatitis
patients attending a private practice dermatology specialist
according to the ethnic group. The rate was not significantly
clinic in Ipoh. It also aims to identify the most common
different from the major ethnic groups but was highest in
contact allergens in this population.
the Chinese followed by Malays and Indians.
Materials and methods
Table 3 shows the prevalence of contact dermatitis to
All patients seen at the Foong Skin Specialist Clinic
standard allergens according to sex. Nickel (30.4%),
between 1999 and 2006 who have had patch tests done were
fragrance mix (18.16%), Balsam of Peru (6.73%), cobalt
included in the study. The age and sex of the patient were
(5.31%), potassium dichromate (3.47%), neomycin (3.27%),wool alcohol (3.27%) and parabens (3.27%). were thecommonest
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Table 1. Prevalence of Allergic Contact Dermatitis according to the age group and sex
Age Group
Table 2. Prevalence of Allergic Contact Dermatitis according to ethnic group and sex
Ethnic Group
Table 3. Prevalence of Allergic Contact Dermatitis according to standard battery
allergens and sex.
Female n+317
Male n=173
Total n=490
Potassium dichromate
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
commonest allergens. Nickel allergy was more common in
dermatitis under the chin as a result of the pin worn by
women. Female patients outnumbered the male patients in
Muslim women. The use of costume jewellery and ear
their allergens for the above except potassium dichromate
piercing are among the common causes of sensitization to
and parabens where the reverse is true.
Fragrance mix (18.16%) was the second commonest contact
Allergic contact dermatitis (ACD) is an important
allergen in this study. The rate appeared to be higher in
dermatologic disease with considerable morbidity and
women (21.14%) than in men (12.72%). Fragrance is
economic impact. It represents delayed type hypersensitivity
present in most perfumes, cosmetics, toiletries and many
to small molecular weight chemicals which acts as haptens.
household products. They are important in our community
It is caused when contact with a specific allergen elicits a
because they are widely used. Balsam of Peru formed the
specific immunologic inflammatory response in the allergic
third commonest contact allergen. Balsam of Peru is a plant
individual 24 to 72 hours after re-exposure. Diagnosis of
product, a balsam derived from the trees of the genus
ACD is frequently facilitated or confirmed through the use
Myroxylan found in Central and South America. It
of patch test procedure.
contains a mixture of fragrance constituents such ascinnamic acid, eugenol, benzyl benzoate, benzyl alcohol,
The prevalence of contact dermatitis to various allergens
vanillin, etc. As such it is a useful marker to detect fragrance
differs in different population group. Therefore, it is
allergy. Not surprising, it was higher in women (9.74%)
important for dermatologists to be aware of the common
than in men (1.73%).
allergens and to monitor them in their place of practice. Atour dermatology clinic in Ipoh, 59.8% of patients had a
Other common contact allergens were cobalt (5.31%),
positive patch test reaction to one or more allergens. The
potassium dichromate (3.47%), neomycin (3.27%), wool
prevalence was 49.5% in Singapore3, 55% in Scotland4 and
alcohol (3.27%) and parabens (3.27%). In women, co-
60.5% in Spain5. In this study the prevalence of ACD and
sensitivity of cobalt and nickel occur commonly due to
the causative allergens are not much different from existing
wearing of costume jewellery. In men, cobalt allergy is often
published epidemiological studies.
associated with chromate allergy due to occupationalcement exposure.
It has been found that allergic contact dermatitis was morefrequent in women as compared to men6. Thepreponderance in women could be due to the high rate of
sensitization to certain allergens such as nickel and
Ang P, Ng SK. Chapter editor: "The Principles and Practice of
fragrances. In our study the prevalence of allergic contact
Contact and Occupational Dermatology in the Asia-Pacific
dermatitis was 64.7% (205/317) in women and 51.4%
Region." Edited by Ng SK and Goh CL. Investigative techniques
(89/173) in men. The prevalence of ACD was significantly
in Contact Dermatitis." World Scientific 2001.
higher in women than in men. (test of significance, p value
Rohna R. Pattern of contact and photocontact dermatitis at
<0.05) However, Goh in his study found that men and
Hospital Kuala Lumpur - a two year study (1994-1996). Paper presented at the Update Contact Allergy Occup Dermatoses,
women were equally susceptible to epicutaneous
Kuala Lumpur, 6 April 1996.
sensitization. In his study the prevalence was 49.2% in
Goh CL. Epidemiology of Contact Allergy in Singapore. Int J
women and 49.8% in men3.
Husain SL. Contact Dermatitis in the west of Scotland. Contact Dermatitis 1977;3:327-332.
ACD in different ethnic groups has seldom been studied
Romaguera, C, Grimalt F. Statistical and comparative study of
before. The prevalence between black and white Americans
4600 patients tested in Barcelona (1973-1977). Contact
appeared to be the same8. In our study, Chinese had the
highest prevalence rate (63%), while Malays had a
Rees JL et al. Sex differences in susceptibility to development
prevalence rate of 55.4% and Indians 41.7%.
of contact hypersensitivity to dinitrochlorobenzene (DNCB) Br J Dermatol 1989; 120:371-374.
Hammershoy O. Standard patch test results in 3225 consecutive
Nickel allergy (30.4%) was the commonest cause of ACD in
Danish patients from 1973-1977. Contact Dermatitis 1980; 6:263-
our study. It was more common in women (36.3%) than in
men (19.3%). The unique ethnic lifestyle has brought about
Leyden JJ, Kligman AM. Allergic contact dermatitis: sex
peculiar presentation of nickel allergy as scarf button
differences. Contact Dermatitis 1977; 3:332-336.
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Prevalence of herpes simplex virus infection in patients
with genital herpes using the immunofluorescent
antibody test
HB Gangaram, MBBS, FRCP1, Akbal Kaur, MBBS1, S Mangalam, MBBS, FRCPath2 and Suraiya H Hussein, MBBS, FRCP1
1Genito-Urinary Medicine Clinic, Department of Dermatology, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia2Department of Pathology, Hospital Kuala LumpurKuala Lumpur, Malaysia
Correspondence
Gangaram Hemandas, MBBS, FRCP
Department of Dermatology
Hospital Kuala Lumpur, 50586 Kuala Lumpur
Email : [email protected]
Conclusions In our study, HSV-2 was still more common causing
57% of the cases seen,
HSV-1 29% and HSV-1 and HSV-2
Background Herpes genitalis (HG) is the commonest cause of
coinfection in 14%. An increased rate of HSV-1 seen could possibly be
sexually transmitted ulcerative disease in the world, including
due to a change in sexual behavior of the patients especially with
Malaysia1. Herpes simplex virus (HSV) type 2 is more frequently
regards to oro-genital sexual contact.
implicated than HSV type 1. This pattern has seen some changes inmany parts of the world, with increasing HSV type 1 rates2.
Keywords Genital herpes, Immunofluorescent antibody test, HSV
types
Objective The aim of this study was to determine the type of HSV
implicated in patients with herpes genitalis at the Genito-Urinary
Medicine Clinic, Department of Dermatology, Hospital Kuala
Herpes genitalis (HG) is the commonest cause of sexually
transmitted ulcerative disease in the world, includingMalaysia1. It is associated with not only physical but also
Methods A retrospective study was undertaken on 242 patients with
important psychosocial and economic consequences.
a diagnosis of herpes genitalis at the Genito-Urinary Medicine Clinic
Herpes simplex virus (HSV) type 2 is more frequently
from January 2000 to December 2004. The study included all cases of
implicated than type 1. This pattern has however seen some
genital herpes in patients aged over 12 years. The typing was done by a
changes in many parts of the world, with HSV type 1
immunofluorescent - labeled monoclonal antibody technique specific
becoming more common than HSV type 2. This is evident
for HSV antigens.
in most parts of the world including Australia, Europe andthe USA. Some of the reasons postulated included earlier
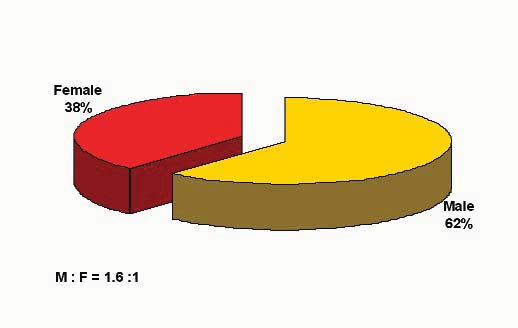
Results Majority (76%) were between the ages of 20-49 years. Males
onset of sexual debut, change in sexual behavior especially
outnumbered females by 1.6:1. Younger women (20-29 years old) tend
with regards to oro-genital sexual contact and lower rates of
to be more frequently affected than their male counterpart. One fourth
(25.7%) of the patients reported having sex with sex workers and lessthan 1% (0.4%) were sex workers. A significant percentage (30.5%) of
The aim of this study was to determine the type of HSV
married men reported extramarital relationship with sex workers or had
implicated in patients with herpes genitalis at the Genito-
a casual or regular partner. Usage of condoms was low at 12%. Clinical
Urinary Medicine Clinic, Department of Dermatology,
diagnosis at presentation was primary herpes genitalis (56%) and
Hospital Kuala Lumpur.
recurrent (44%). 162 (67%) out of a total of 242 patients had the herpesimmunofluorescent test done. 110 (68%) of those done were negative.
Materials and Methods
Only 34 (21%) of patients with herpes genitalis had a positive
A retrospective study was undertaken on 242 patients with
immunofluorescent antibody test. Of the 21%, herpes simplex virus
a clinical diagnosis of herpes genitalis at the Genito-
type 2 was found in 19 (12%) of patients with herpes genitalis, HSV
Urinary Medicine Clinic from January 2000 to December
type 1 in 10 (6%) and HSV types 1 & 2 coinfection in 5 (3%) patients.
2004. The study included all clinical cases of genital herpesin patients aged over 12 years. Specimens were collectedfrom

Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
from genital lesions with a cotton-tipped swab and smeared
Kingdom3. This direct immunofluorescent antibody
onto micro-wells of daflon-coated slides, air-dried, fixed
technique (IFAT) read with a fluorescent microscope was
with acetone and stained with ImagenTM HSV-1 or HSV-
utilized for HSV detection as well as typing. This is the
2 using specific monoclonal antibodies conjugated to FITC
routine, cost-effective and rapid detection method for
in two individual wells, from Dalco Cytomation Co; United
genital HSV in this hospital.
Table 1. Total number of new cases of
Table 2. Source of referral of herpes genitalis
herpes genitalis by year (n=242)
A total of 242 case notes were reviewed
Majority of the patients were self-referred or camefrom the outpatient department of the hospital
Table 3. Occupation of patients with herpes genitalis
Table 4. Distribution of herpes genitalis by age & sex
Younger women (20-29 years old) tend to suffer more fromherpes genitalis than men.
Majority were office-workers. Only 1% of the patientswere commercial sex workers.
Table 5. Risk factors and marital status in patients with
herpes genitalis (n=282)
Table 6. Provisional diagnosis at first visit (n=242)
Provisional diagnosis at first visit was :Primary herpes genitalis 135 (56%) Recurrent herpes
A significant percentage (30.5%) of married men reported
genitalis 107 (44%)
extramarital relationship with sex workers or had a casual orregular partner
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Table 7. Correlation of clinical presentation and
immunoflourescent test (n=162)
In primary herpes genitalis, HSV type 2 accounted for 70.6% ofthe positive cases, HSV type 1, 17.6% and HSV types 1 and 2coinfection in 11.8%. In recurrent herpes genitalis, HSV types 1and 2 were found to be equally frequent (41.2%) and HSV types1 and 2 coinfection in 17.6%.
Figure 1. Age distribution of patients with herpes
genitalis (n=242)
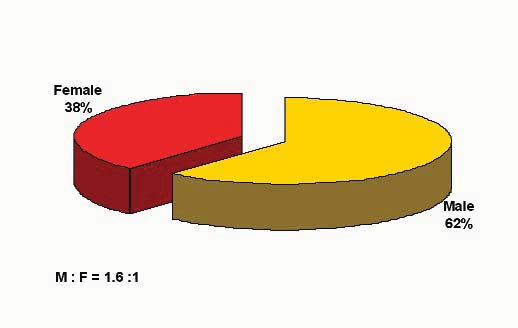
Figure 2. Distribution of herpes genitalis by sex (n=242)
Majority (76%) of the patients were between the ages of
Males outnumbered females by 1.6 :1
Figure 3. Racial distribution of patients with herpes genitalis
(n=242)
Malays accounted for 44%, Indians 28% and Chinese 25% of the totalpatients. This probably reflects the normal pattern of clinic attendance
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
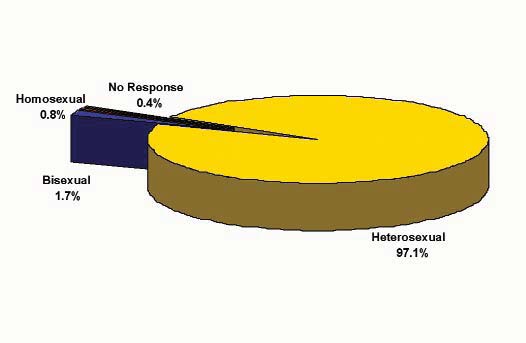
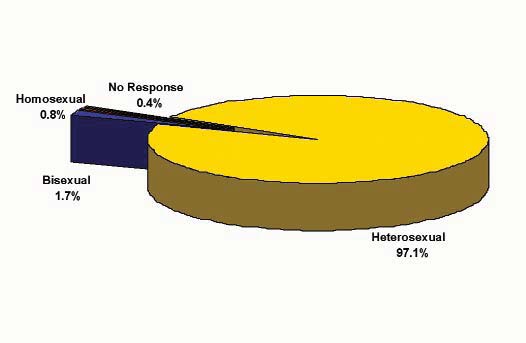
Figure 4. Sexual orientation of patients with herpes
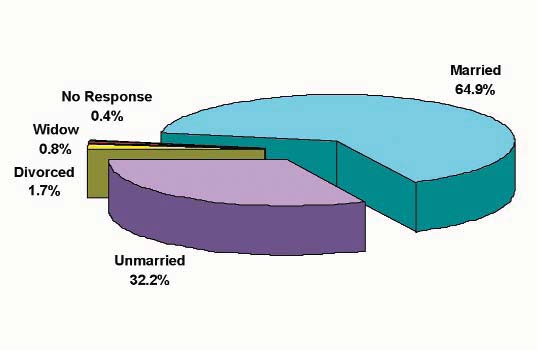
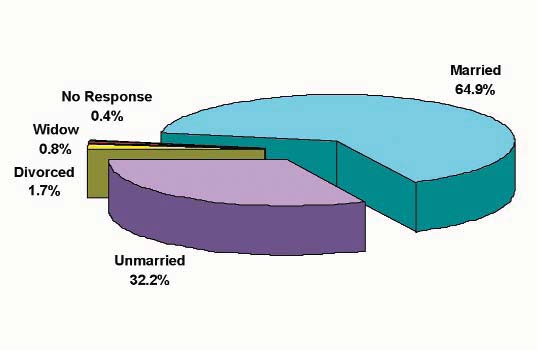
Figure 5. Marital status of patients with herpes genitalis
genitalis (n=242)
Majority (97%) of the patients were heterosexually
About two thirds (64.9%) of the patients were married
Figure 6. Risk factors in patients with herpes genitalis (n=242)
About 1/4 (25.7%) of the patients reported sex with sex workers. Lessthan 1% (0.4%) of the patients were sex workers
Figure 7. Use of condoms by patients with herpes genitalis (n=242)
Condom usage was low (12%)
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Figure 8. Herpes immunoflourescent test in patients with herpes genitalis
(n=162)
162 (67%) patients had the herpes immunofluorescent antibody test done.
110 (68%) of those done were negative. Only 34 (21%) patients with herpesgenitalis had a positive immunofluorescent antibody test. Of the 21%,herpes simplex virus type 2 was found in 19 (12%) patients with herpesgenitalis, HSV type 1 in 10 (6%) and HSV types 1 & 2 coinfection in 5 (3%)patients. Therefore, the most frequent type of HSV causing herpes genitalisin our study was found to be HSV type 2 (57%), HSV type 1 (29%) and HSVtype 1 & 2 coinfection (14%).
to new patients6, longer time between recurrences, and
Genital herpes is a common lifelong virally transmitted
lower clinical recurrence rates7. Once the primary or non-
sexually transmitted disease which may cause not only
primary attack has resolved, 88% of untreated patients with
significant physical but also severe psychological and
HSV-2 genital infection suffer episodes of recurrence at a
emotional impact on the life of a patient. It almost certainly
mean rate of 0.3 and 0.4 recurrences per month, compared
facilitates HIV acquisition4 and can cause a life-threatening
to 55% of people infected with HSV-1 with a mean
encephalopathy if transmitted to an infant around birth5. It
recurrence of 0.09 per month8.
is hence important that we make an accurate diagnosis. It isequally important to determine the infecting viral type in
Recent studies suggest that HSV-1 is becoming more
order to assess the natural history, prognosis and clinical
frequent as a cause for genital herpes2. The table below
management of a patient with genital herpes. The clinical
compares the prevalence of HSV-1 and 2 in genital herpes
presentation of genital primary HSV-1 and HSV-2
in various countries. A striking observation seen in both the
infections is similar. However, their natural history is
Bangkok and Sydney studies was the increase in rates of
different. Genital HSV-1 infections are characterized by
HSV-1 as a cause of genital herpes. Our HSV-1 rate is
less asymptomatic shedding, a lower transmission frequency
similar to the second study done in Sydney.
Prevalence of Herpes simplex virus using immunofluorescence antibody test type (IFAT)
Bangkok, Thailand*
Western Sydney, Australia2 **
*Used viral culture followed by IFAT **Used viral culture followed by IFAT
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
The sensitivity of the IFAT is about 75%. The specificity
however, is higher at 85%. Viral culture, said to be the ‘goldstandard', is not routinely available in our hospital.
S Zainah, M Sinniah, Y M Cheong et al. A microbiological study
Although the PCR assay is available in-house, we did not
of genital ulcers in Kuala Lumpur. Med J Malaysia 1991;46:274-
apply this technique for HSV diagnosis on genital lesions
L J Haddow, B Dave, A Mindel et al. Increase in rates of herpes
mainly because of the prohibitory cost. Moreover, the
simplex virus type 1 as a cause of anogenital herpes in western
genital lesion specimens are collected sporadically, not in
Sydney, Australia, between 1979 and 2003. Sex Transm Infect
batches. The IFAT can be applied to even one clinical
sample at a time, is rapid giving results within an hour, if
Patrick C.Y. Woo, Susan S Chiu, Wing-Wong Seto, Malik Peiris. Cost-effectiveness of rapid diagnosis of viral respiratory tract
necessary. The benefits of Imagen IFAT technique over
infections in pediatric patients. J Clin Mivrobiol 1997;35(6):1579-
viral isolation for reduction of hospitalization and
reduction of anti-bacterial use, are well established. The
Freeman EE, Weiss HA, Glynn JR, et al. Herpes simplex virus 2
immunofluorescence positive rate for herpes simplex virus
infection increases HIV acquisition in men and women:
in our study was about 21%. Being a retrospective study,
systematic review and meta-analysis of longitudinal studies. AIDS 2006;20:73-83.
some of the reasons for this would include the stage of the
Whitley R. Neonatal herpes simplex virus infections. J Med Virol
disease when the specimen was taken, possibility of
inadequate specimen for antigen testing, pretreatment with
Kinghorn GR. Limiting the spread of genital herpes. (Review)
specific anti-viral agents, and the technique itself.
(39 refs). Scand Infect Dis (suppl.) 1996;100:20-5.
Mindel A, Weller IV, Faherty A, Sutherland S, Fiddian AP, Adler MW. Acyclovir in first attacks of genital herpes and prevention
In conclusion, our study showed that HSV-2 was found in
of recurrences. Genitouri Med 1986;62:28-32.
12% of patients with herpes genitalis, HSV-1 in 6% and
Corey L. The current trend in genital herpes: progress in
HSV-1 & 2 co-infection in 3%. Therefore, the most
prevention. Sex Trans Dis 1994;21:S38-44.
common type of HSV causing herpes genitalis is HSV-2
Puthavathana P, Kanyok R, Horthongkham N, Roongpisuthipong A.Prevalence of herpes simplex virus infection in patients
(57%), followed by HSV-1 (29%) and HSV-1 & 2 co-
suspected of genital herpes; and virus typing by type specific
infection (14%). The increased rate of HSV-1 is possibly
fluorescent monoclonal antibodies. J Med Assoc Thai 1998
due to a change in sexual behavior of the patients especially
with regards to oro-genital sexual contact.
Bhattarakosol P, Visaprom S, Sangdara A, Mungmee V. Increase of genital HSV-1 and mixed HSV-1 and HSV-2 infection inBangkok, Thailand. J Med Assoc Thai 2005 Sep;88 Suppl4:S300-4.
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Autoimmune Bullous Diseases in Ipoh, Malaysia:
A 5-Year Retrospective Study
Tang MM, MD, MRCP, Chan LC, MD, MMed and Heng A, MBBS, MRCP
Department of Dermatology, Ipoh HospitalIpoh, Perak, Malaysia
Correspondence
Agnes Heng, MRCP
Department of Dermatology
Ipoh Hospital, 30990 Ipoh, Malaysia
Email : [email protected]
Introduction
Autoimmune bullous diseases (ABD) represent a group of
Background Autoimmune bullous diseases (ABD) represent a group
chronic blistering dermatoses in which management is
of chronic blistering dermatoses in which management is often
often challenging. Broadly, it encompasses the pemphigus
challenging. Epidemiologic data on these diseases in Malaysia has been
group in which 2 major subtypes are recognized, namely,
pemphigus vulgaris (PV) and pemphigus foliaceus (PF);and the subepidermal group which includes bullous
Objectives Our purpose was to study the spectrum of the various
pemphigoid (BP), dermatitis herpetiformis (DH), linear
ABD presented to the Department of Dermatology, Ipoh Hospital,
IgA bullous dermatosis (LABD),
and to determine the clinico-epidemiological pattern of the 2 main
pemphigoides (LPP), epidermolysis bullosa aquisita (EBA),
ABD, namely pemphigus and bullous pemphigoid.
cicatricial pemphigoid (CP), pemphigoid gestationis (PG)and bullous systemic lupus erythematosus (BSLE).
Methodology We performed a retrospective review of records for all
Epidemiologic data on these conditions in Malaysia has
patients who were diagnosed with ABD confirmed by histopathology
been limited. In 1992, a study carried out in a university-
and direct immunofluorescence test in this centre between 2001 and
based hospital in Malaysia on the epidemiology of ABD
2005. The data were analyzed with regard to age, sex, ethnicity,
showed that pemphigus vulgaris was the commonest ABD
subtypes of ABD, treatment provided and outcome.
encountered followed by bullous pemphigoid, with anincidence of 0.2/100,000/year and 0.12/100,000/year
Results There were a total of 79 cases of ABD presented to us during
respectively1. The study also showed that Indians were
this period. Bullous pemphigoid was observed to be the commonest
more likely to develop ABD, especially BP, when compared
(60.8%) followed by the pemphigus group (36.7%) with the mean
to the other ethnic groups in Malaysia.
incidence of 0.45/100,000/year and 0.28/100,000/year respectively.
44% of patients were of ethnic Chinese origin. There was an overall
We aim to study the spectrum of various ABD presented to
female preponderance. The mean age of presentation was 65.5 years for
the Dermatology Department, Ipoh Hospital, Malaysia and
bullous pemphigoid and 55 years for pemphigus group. The mean
to determine the clinico-epidemiological pattern of the 2
duration of disease before presentation was 1.6 months for bullous
main ABD, namely pemphigus and bullous pemphigoid.
pemphigoid and 6.3 months for pemphigus. Various combinations ofimmunosuppressive agents were used to treat the patients. 48% of
Materials and Methods
bullous pemphigoid cases were controlled with prednisolone alone
The Department of Dermatology, Ipoh Hospital, is the
while 67.9% of pemphigus group required at least 2
main referral centre for all dermatological diseases in the
immunosuppressive agents to achieve disease control.
state of Perak, Malaysia, with a catchment area of about2.15 million populations. The ethnic mix of Perak's
Conclusion In our study population, bullous pemphigoid was more
population between 2001 and 2005 comprised 53% Malay,
frequently seen than pemphigus.
31.5% Chinese, 12.8% Indian and 2.7% others. In thisretrospective study, the case records of all patients diagnosed
Keywords Autoimmune bullous diseases, bullous pemphigoid,
to have ABD in Ipoh Hospital between January 2001 and
pemphigus vulgaris
December 2005 were analyzed.
Patients with typical clinical and histopathological findingswere included. Diagnosis was further confirmed by directimmunofluorescence (DIF) test from perilesional skinbiopsy.
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
biopsy. Various clinico-epidemiological characteristics
achieve disease control was 3.8 months for BP and 13.6
including age, sex, ethnicity, duration of disease, treatment
months for pemphigus.
provided and the outcome were analyzed for all cases.
Disease was considered controlled when the skin eruptions
Among the 48 patients with BP, 11 (23%) died but none of
were minimal while the patients were receiving treatment.
the deaths were directly related to their disease. The cause
Remission was defined as no development of new lesions
of death was due to other medical problems like
and patients were able to taper down the
cerebrovascular accidents, ischaemic heart disease,
immunomodulators. The data findings were analyzed using
complications of diabetes and malignancy. Of the 5 out of
SPSS statistical analysis for Windows 10.
29 patients with pemphigus who died, 1 succumbed tosepsis while the others died of unrelated illnesses. None of
the BP patients had active disease at the time of death and
Over the 5 year period, 79 patients were diagnosed to have
were on low dose corticosteroids.
ABD in which 48 (60.8%) had bullous pemphigoid (BP);29 (36.7%) pemphigus (pemphigus vulgaris (PV) -16,
pemphigus foliaceus (PF) -11, pemphigus vegetans (PVG)
Bullous pemphigoid was the commonest ABD seen at our
-1 paraneoplastic pemphigus (PNP) -1); 1 (1.3%) linear
centre, representing 60.8% of all cases. This is in contrast to
IgA bullous dermatosis and 1 (1.3%) lichen planus
the previous study done in Malaysia1 in which pemphigus
pemphigoides. The racial distribution for all cases of ABD
was more commonly encountered. The incidence rate of
was as follows: 44% Chinese, 37% Malay and 16% Indian.
0.45/100,000/year and 0.28/100,000/year respectively for
There was a female preponderance in both BP and
BP and pemphigus is higher than previously thought.
pemphigus group with a male to female ratio of 1:1.53 and
However, the true incidence of ABD in this region may be
1:1.8 respectively. The estimated incidence of BP in the
higher than reported in this study as some cases may have
state of Perak, Malaysia was 0.45/100,000/year whereas for
been treated and followed up by dermatologists in private
the pemphigus group was 0.28/100,000/year. The age of
practice and hence, not captured in this study. Mild cases of
patients at presentation ranged from 15 to 91 years; the
BP with localized disease may have also been treated by
mean age of presentation for BP and pemphigus was 65.5
primary care physicians and not reaching us. There may also
years and 55 years respectively. Patients with BP appeared to
be some referral bias; for example pemphigus confined to
present earlier with the mean disease duration before first
the oral mucosa may have been referred to the dentists and
presentation of 1.6 months (range 0.3 – 12 months) for BP
CP to the ophthalmologists. Furthermore, some cases could
compared to 6.3 months (range 0.3 – 48 months) for the
have been treated by traditional/complementary medicine
pemphigus group (Table 1).
(TCM) practitioners instead as this is not an uncommonpractice among Malaysians. This could explain the lower
Among the pemphigus cases, PV was the predominant
incidence for both BP and pemphigus in this region as
subtype seen in 16 patients followed by PF in 11 patients,
compared to the incidence rate of other countries (Table 4).
pemphigus vegetans (PVG) in 1 patient and paraneoplasticpemphigus (PNP) in 1 patient. PV appeared to be more
There was a predilection of ABD for ethnic Chinese which
common among the Chinese (50%) while PF was more
comprised 44% of all cases although they constitute only
frequently seen among Malays (54.5%). The mean age of
31.5% of the Perak population during the study period. The
presentation was 49.6 years for PV and 65.2 years for PF.
Malays, on the other hand, were less likely to develop ABD
The mean duration of disease before presentation was 7.1
while the percentage of Indians affected corresponds to the
months for PV and 6.7 months for PF (Table 2). One
ethnic distribution of this region. This, again, differed from
patient presented with oral erosions for 4 years to various
the result of an earlier study done in this country which
doctors before the diagnosis of mucous membrane PV was
showed a predilection of ABD for ethnic Indians1.
made while another patient with PF took 3 years before
Although the incidence of ABD in the Malays was
presenting to us. Our only patient with PNP was a 65 year
relatively lower, it was observed that they were more
old Malay female with non-Hodgkin's lymphoma stage 3B
predisposed to develop PF where they made up of 54.5% of
who succumbed to her disease even before treatment was
all PF cases in this study (Table 2). The Singapore study
instituted. Majority of the PV patients had both oral
noted an over-representation of PF in their Malay
erosions and skin lesions while none of the PF patients had
population, which constituted 25% of all PF cases studied
when compared to their normal ethnic composition, ofwhich the Malays constitute 10%4.
Prednisolone was used alone or together with variouscombinations of immunomodulators to treat the ABD
Although an equal sex predisposition has been reported in
which included azathioprine, dapsone, cyclophosphamide,
the previous Malaysian study1, we observed a female
tetracycline and mycophenolate mofetil (Table 3). Majority
preponderance in both bullous pemphigoid (M:F = 1:1.53)
of the pemphigus cases (67.9%) required at least 2
and pemphigus (M:F = 1:1.8). A similar observation was
immunomodulators to treat while 47.9% of BP cases were
also seen in Kuwait2,3. Singapore reported an equal sex
controlled with prednisolone alone. The mean duration to
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Table 1. Comparison of characteristics between bullous pemphigoid and pemphigus
Bullous pemphigoid (n=48)
Incidence (per 100,000/year)
Duration to diagnosis (months)
Duration to disease control (months)
No. of deaths over 5 years
Table 2. Demographic data, treatment and course of disease in patients with pemphigus vulgaris and
pemphigus foliaceus
Duration of disease before diagnosis (months)
Prednisolone alone
Prednisolone + 1 adjuvant
6 (37.5%) 5 (45.5)
Prednisolone + 2 adjuvants
5 (31.3%) 2 (18.2%)
1 (6.3%) 2 (18.2%)
Course of disease
Duration to disease control (months)
No. of patients with disease controlled
No. of patients in remission
No. of patients with active disease
No. of patients transferred to other centre
No. of patients who died of disease/sepsis
No. of patients who died of unrelated causes
No. of patients lost to follow-up
* lost to follow-up before treatment was instituted
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Table 3. Therapy for bullous pemphigoid and pemphigus
Combinations of Immunomodulators
(PV + PF+ PVG)
Prednisolone alone
Prednisolone + Azathioprine
Prednisolone + Tetracycline
Prednisolone + Dapsone
Prednisolone + Cyclophosphamide
Prednisolone + Methotrexate
Prednisolone + Azathioprine + Dapsone
Prednisolone + Cyclophosphamide + Tetracycline
Prednisolone + Azathioprine + Tetracycline
Prednisolone + Mycophenolate +Tetracycline
* 1 BP patient and 3 pemphigus patients defaulted follow-up before treatment was instituted.
Table 4. Incidence of bullous pemphigoid and pemphigus in studies carried out in different regions of the
world
Incidence (per 100,000 per year)
Country and year of publication
Southern Saudi Arabia 200116
Current study (Perak, Malaysia)
distribution in pemphigus4 but a striking female
indirect immunofluorescence test at the time of the study
preponderance (M:F = 1:2) in their BP patients5. Similar
period and therefore some of the cases may have been
female predominance was also observed in previous
grouped together with BP since they share similar DIF
pemphigus studies from Greece6 (M:F = 1:2.25 ), Turkey7
findings. We also did not have any cases of BSLE despite
(M:F = 1:1.41) and Iran8 (M:F = 1:1.33). The factors
SLE being a fairly common disease in this region. This
responsible for this gender difference have yet to be
could either be due to the incidence of BSLE being rare in
this region or the cases were being treated byrheumatologists instead. We have had few cases of CP, PG
While the Singapore study reported EBA to be their second
and DH on our follow-up but no new cases during the 5
commonest subepidermal immunobullous disorder3, we had
year study period. This finding is similar to the studies done
none during our study period. This could be explained by
in Singapore5 and China11 which reflects the rarity of these
the fact that we did not have facilities for salt-split skin
diseases in this region.
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
The first line of treatment for all cases of ABD was with
incidence rate is higher for both BP and pemphigus than
oral prednisolone. Adjuvant therapy with various
previously thought. Chinese are more predisposed to ABD,
immunomodulators was added when prednisolone alone
especially BP and PV, while PF is more common in Malays.
was not enough to achieve disease control. The choice for
There is no evidence of a predilection for ethnic Indians as
adjuvant therapy was azathioprine or dapsone as they are
previously reported1. There is a female preponderance
effective and relatively inexpensive. In the event of an
among BP and pemphigus patients and a low occurrence of
adverse drug reaction or poor response to these 2
other subepidermal blistering diseases like EBA, CP, DH,
other drugs like methotrexate,
PG and BSLE in our patients. These results provide a basis
cyclophosphamide and mycophenolate mofetil were used
on which future research activities in this region can be
instead. Tetracycline was usually added as a third agent
when 2 drugs were not adequate to control the disease. Wefound mycophenolate mofetil to be an effective adjuvant
therapeutic agent in 2 of our pemphigus patients who hadfailed to respond the other conventional agents. In addition
Adam BA. Bullous diseases in Malaysia: epidemiology and
to systemic therapy, most of our patients also received
natural history. Int J Dermatol 1992; 31: 42-45.
treatment with potent topical corticosteroids.
Nanda A, Dvorak R, Al-Saeed K, Al-Sabah H, Alsaleh QA. Spectrum of autoimmune bullous diseases in Kuwait. Int J Dermatol 2004, 43: 876-881
As expected, BP was easier to control compared to
Alsaleh QA, Nanda A, Al-Baghli NM, Dvorak R. Pemphigus in
pemphigus. About half of the BP patients (47.9%) achieve
Kuwait. Int J Dermatol 1999; 38:351-356
disease control with prednisolone alone compared to only
Goon A, Tan SH. Comparative study of pemphigus vulgaris and
25% of pemphigus patients. The duration to disease control
pemphigus foliaceus in Singapore. Australasian J Dermatol 2001;42:172-5
was also shorter in BP compared to pemphigus, with a mean
Wong SN, Chua SH. Spectrum of subepidermal immunobullous
duration of 3.8 months and 13.6 months respectively (Table
disorders seen at the National Skin Centre Singapore: a 2-year
1). Although the number of deaths was higher in the BP
review. Br J Dermatol 2002; 147: 476-480.
group, all deaths were due to unrelated causes as most of the
Michailidou EZ, Belazi MA, Markopoulous AK, et al.
BP patients were older and had concomitant illnesses. It is
Epidemiologic survey of pemphigus vulgaris with oral manifestation in northern Greece: Retrospective study of 129
noteworthy that none of them had active disease at the time
patients. Int J Dermatol 2007; 46: 356-361
of death. This result is in keeping with a previous study
Uzun S, Durdu M, et al. Pemphigus in the Mediterranean region
done in Scotland9 which reported the first year mortality
of Turkey: A study of 148 cases. Int J Dermatol 2006, 45, 523-528
rate of 25%. Most deaths were related to old age and the
Salmanpour R, Shahkar H, Namazi MR, Rahman-Shenas MR.
general condition of the patient and rarely due to BP itself.
Epidemiology of pemphigus in South Western Iran: A 10-year retrospective study (1991-2000). Int J Dermatol 2006; 45,103-105.
Another study from Germany10 demonstrated the first year
Gudi VS, White MI, Cruickshank N, et al. Annual incidence and
mortality rate of 29% and they attributed low serum
mortality of bullous pemphigoid in the Grampian Region of
albumin, high dosage of corticosteroids and old age as risk
North-east Scotland. Br J Dermatol 2005; 153: 424-427.
factors for lethal outcome in BP.
Rzany B, Partscht K, Jung M et al. Risk factors for lethal outcome in patients with bullous pemphigoid: low serum albumin level, high dosage of glucocorticosteroids, and old age.
Between PV and PF, PV appeared to be more difficult to
Arch Dermatol 2002; 138: 903-8.
control with about one third of them requiring 2 adjuvant
Jin P, Shao C, Ye G. Chronic bullous dermotoses in China. Int J
agents to achieve disease control. The duration needed to
Dermatol 1993; 32: 48-52
achieve control was also longer. It is interesting to note that
Bernard P, Vaillant L, Labeille B, et al. Incidence and distribution of subepidermal autoimmune bullous skin diseases in three
our PF patients present at an older age (mean 65.2 years)
French regions. Arch Dermatol 1995; 131: 48-52.
when compared to neighbouring Singapore4 (57 years) and
Zillikens D, Wever S, Roth A, et al. Incidence of autoimmune
Turkey7 (52 years). The reason for this is unclear but it could
subepidermal blistering dermatoses in a region of central
explain the higher mortality encountered in these patients.
Germany. Arch Dermatol 1995; 131: 957-958.
Mahé A, Flageul B, Cissé I, et al. Pemphigus in Mali. A study of 30 cases. Br J Dermatol 1996; 134: 114-119.
Tsankov N, Vassileva S, Kamarashev J, et al. Epidemiology of
The results of our retrospective study demonstrate that BP
pemphigus in Sofia, Bulgaria. A 16-year retrospective study
is almost twice as common as pemphigus. This is
(1980-1995). Int J Dermatol 2000; 39: 104–108.
comparable to reports from Singapore where they found BP
Tallab T, Joharji H, Bahamdan K, et al. The incidence of pemphigus in Southern region of Saudi Arabia. Int J Dermatol
to be three times more common than pemphigus5. The
2001; 40: 570-572.
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
The effect of explanation and demonstration of topical
therapy on the clinical response of atopic eczema
Tang MM, MD, MRCP, Chan LC, MD, MMed and Heng A, MBBS, MRCP
Department of Dermatology, Ipoh Hospital, Ipoh, Perak, Malaysia
Correspondence
Tang Min Moon, MRCP (UK)
Department of Dermatology
Ipoh Hospital, 30990 Ipoh, Perak, Malaysia
Email : [email protected]
evidenced by a further reduction to 67% (p=0.001) by week 4. In groupB, a significant SASSAD score reduction (64.8%; p=0.002) was seen
Background Atopic eczema is a common dermatological condition
only at week 4 after patient education and demonstration. The
seen in our practice in which the mainstay of treatment is topical
magnitude of improvement in patients' symptoms which included itch,
medications. One of the main reasons for poor clinical response to
sleep disturbance and irritability, measured by the patient using visual
therapy in atopic eczema is the lack of understanding of topical
analog score, were only significant for group A after 4 weeks.
preparation usage and thus poor adherence to treatment.
Conclusions This study reinforces the importance of explanation and
Objectives The aim of this study is to determine the effect of
demonstration on the proper usage of topical medications in achieving
explanation and demonstration of topical medication on the clinical
better clinical response. Failure to explain on the use of topical
response of atopic eczema.
medications may lead to patient dissatisfaction, poor compliance andlack of treatment efficacy.
Methodology Twenty newly diagnosed patients with atopic eczema
who fulfilled the study criteria were recruited and randomized
consecutively into 2 groups - A & B. All patients were assessed on the
The cause of failure of response to therapy in many
severity of the eczema using the six area, six sign atopic dermatitis
dermatological skin conditions including atopic eczema is
severity score (SASSAD) and patients' assessment of itch, sleep
poor adherence, rather than severity of disease. This can
disturbance and irritability were recorded on 10-cm visual analogue
arise from a number of reasons, the most important of
scales. They were also assessed on their level of understanding on the
which is a lack of understanding of topical applications.
proper usage of topical medications using a questionnaire. Group A
Other reasons include failure to renew prescriptions, under-
then received explanation and demonstration on how to apply the
prescribing, lack of faith in the treatment, or insufficient
topical medications while Group B was not educated on these. They
time to apply the medication. About 80% of our patients are
were followed up 2 weeks after treatment and were re-evaluated on
prescribed more than one topical medication at any one
their understanding and the severity of their skin condition. This was
time. Confusion with treatment may arise when patients are
followed by education by a dermatology nurse on the proper usage of
not educated on the proper usage of the various topical
topical medications for both groups. A third evaluation was done 2
medications. So far there is no published record of any
weeks later.
studies carried out in Malaysia to support the fact thatimproving patients' knowledge of proper topical application
Results At baseline, 70% of the patients did not understand the
by explanation and demonstration will improve the
potency of topical corticosteroid and between 20-30% of them did not
outcome of treatment. Atopic eczema is chosen for this
know the correct sites, frequency, time and duration of each topical
study because it is one of the commonest conditions seen at
application prescribed. About two thirds of the patients claimed that
our clinic; the modality of treatment is mainly by topical
they did not receive any explanation or demonstration from either their
medications and the availability of a standard scoring
doctors or the pharmacy dispensers. After education on the proper
system of severity of disease.
usage of topical medications, the level of understanding improved to100% for group A at visit 2 and group B at visit 3. A clinical
In this study, we aim to determine the effect of explanation
improvement as measured by SASSAD score reduction was seen in
and demonstration of topical medications by a trained
both groups. In group A, a significant SASSAD score reduction of
dermatology nurse on the clinical response of atopic
49.5% (P=0.003) was seen after 2 weeks and it was sustainable, as
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Materials and Methods
New patients who were diagnosed with moderate to severe
A total of 20 patients participated in the study. At baseline,
atopic eczema using the Hanifin and Rajka Criteria1 at the
60% of the respondents recalled not receiving any
Dermatology Clinic Ipoh Hospital between February to
demonstration from the doctors on how to apply the topical
August 2006 were recruited into the study. Patients who
treatments and 55% claimed that the dispensers did not give
have had any previous consultations with a dermatologist or
any explanation to them. 70% of the respondents did not
at any dermatology department were excluded. Those who
understand the potency of the topical corticosteroid
have a skin disorder other than atopic eczema in the area to
prescribed and between 20-30% of them did not know the
be treated were also excluded from this study.
correct sites, frequency, time and duration of each topicalapplication prescribed.
Once the patients were enrolled, they were randomizedconsecutively into 2 groups, Group A and Group B. The
Only 14 patients were followed till the end of the study, 7
severity of atopic eczema was determined by a global
each for group A and B. The 6 patients who did not
physician assessment using the Six Area, Six Sign Atopic
complete the study were excluded from further analysis.
Dermatitis (SASSAD) severity score2 (Appendix 1). The
Out of the 6, 2 defaulted scheduled follow-up, 3 were not
patients' assessments of itch, sleep disturbances and
willing to spend additional time at the clinic for further
irritability were recorded on 10-cm visual analogue scales.
assessment and explanation, and therefore left aftercollecting their medications from the pharmacy and 1 felt
After consultation, a prescription was given to the patients
that the skin lesion had improved and did not want further
to collect their medications from the out-patient pharmacy.
consultation. After education on the proper usage of topical
They were instructed to return to the clinic after collecting
medications, the level of understanding had improved to
their medications to fill up a study questionnaire assessing
100% for group A at visit 2 and group B at visit 3.
their knowledge about the treatment given by their doctors.
For patients below 17 years of age, their parents or
Both groups showed a reduction in SASSAD score (clinical
guardians responded to the questionnaire. Patients who did
improvement) at Visit 2 and Visit 3 (Figure 1). A
not know how to read or write were interviewed by the
significant reduction of 49.5% (p=0.003) in the severity of
study nurse. Following that, Group A received explanation
eczema was noted after 2 weeks (Visit 2) in Group A and a
regarding their disease followed by demonstration on how
further reduction of 67% (p=0.001) was noted after 4 weeks
to apply the topical treatments by a trained nurse from the
(Visit 3). In Group B, a significant reduction of SASSAD
dermatology clinic. All their topical treatments were labeled
score (64.8%; p=0.002) was only noted at week 4 (Table 1).
with cartoon and multi-languages stickers. Patientinformation leaflets regarding the disease and the topical
For the improvement of symptoms based on visual analogue
treatments which were available in 3 languages (English,
scores, there was a reduction of score at every visit for both
Malay, and Mandarin), were handed out to the patients.
groups (Figure 2, 3, 4). At the end of the study, there was a
Group B, on the other hand, did not receive additional
significant improvement for itch, sleep disturbance and
explanation or demonstration from the nurse.
irritability for group A whereas in group B, only the scorefor sleep disturbance showed significant reduction at Visit 3
Both groups of patients were reviewed after 2 weeks (Visit
(Table 2).
2). All patients were re-assessed on their knowledge of thecorrect usage of topical treatments. The disease severity was
again assessed using SASSAD score and patients'
Due to the busy clinics and heavy workload, most doctors
assessments using visual analogue scale. They were given the
do not spend enough time explaining the nature of a disease
same prescription as the first visit and were instructed to
and the proper use of medications prescribed to their
return to the clinic after collecting their medications from
patients. Moreover, doctors tend to depend very much on
the pharmacy. This time, all patients from both Group A
the pharmacists or dispensers to teach patients on the usage
and Group B were educated on the methods of application
or administration of medications prescribed by them. In
of their medications. This was again reinforced using
addition, patient educational materials are also insufficient
written instructions. Medications were labeled and
for patients' reference after each consultation. Educating the
information leaflets on the disease were also given.
patients or parents helps them to take charge of themanagement of their illness. One trial had demonstrated
Both groups were followed up 2 weeks later (Visit 3) and
that education and demonstration of treatment for atopic
were re-assessed on their knowledge of the correct usage of
eczema improved parents' knowledge and the outcome of
topical treatments. The disease severity was assessed using
their child's eczema3. Our current study is the first study
SASSAD score and patients' assessments using visual
done in Malaysia to support this finding.
analogue scale. All results were analyzed and interpretedusing SPSS program version 10.0.
From the literature review, only 5-20% of parents hadreceived or recalled receiving any explanation of the causesof eczema or demonstration on how to apply topicaltreatments and the side effects of the topicalcorticosteroids4, 5, 6. Thirty to 60% of patients who werefgfgfg
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Table 1. The Magnitude of SASSAD score reduction for Group A and B
% of reduction at
Visit 2 (p value) baseline (p value)
49.5* (0.003)
35.2 (0.054)
67.3* (<0.001)
34 (0.043)
46.6 (0.03)
64.8* (0.002)
Table 2. The Magnitude of Symptom Improvement using Visual Analog Score
baseline (p value)
51.9* (0.007)
45.8* (0.007)
43.3* (0.009)
58.1* (0.007)
* Significant (p<0.01)
Figure 1. Global Physician Assessment on the severity of Atopic Eczema using
Six Area, Six Sign Atopic Dermatitis severity Score (SASSAD)
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Figure 2. Comparison of Mean Reduction of Itch between Group A and B
Figure 3. Comparison of Mean Reduction of Sleep Disturbances between Group
A and B
Figure 4. Comparison of Mean Reduction of Irritability between Group A and B
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
prescribed topical corticosteroid were not aware of the
demonstration was given to them (Table 1). Besides
potency and resulted in either over or under usage of the
improvement in the disease severity, we also found that
topical application5,7. Following repeated education and
there was improvement in the patients' symptoms of itch,
demonstration of topical therapies by a specialist
sleep disturbances and irritability.
dermatology nurse, there was a 65% reduction in theseverity of the eczema (SASSAD severity score) after 3
The main limitation of this study is the small sample size.
The disease severity of Group A appeared to be milder thanGroup B at baseline. We felt that this randomization bias
We had excluded patients from entry into this study if they
was due to the small number of subjects in the study. In
have had any previous consultation with any dermatology
addition, the magnitude of symptom improvement of itch
centre, in order to provide a population who had not been
and irritability in Group B after education and
exposed to a dermatologist or specialist dermatology nurse
demonstration were not statistically significant as compared
in the past. At the first visit, which reflected the usual
to Group A (Table 2). This, again, could be due to the small
dermatology clinic consultation, majority of patients
sample size.
claimed they received neither explanation nordemonstration on how to apply topical medications from
At the end of the study, we noted that the key to the
the doctors or dispensers at the pharmacy. After
successful management of atopic eczema is to spend time to
questioning, not all of them understood completely the
listen and to explain the nature of disease and how to use
correct use of topical medications. It is not possible to
topical therapies and dressings. In addition to explanation,
determine whether the lack of knowledge was due to failure
practical demonstrations on how to apply topical
of the healthcare providers in educating the patients/parents
medications and dressings should be given to the patients or
or because they had forgotten what they had been told.
parents. Patients or parents should also be given written
Either way, one can conclude that at the end of a
instructions and information to reinforce the therapies
consultation, appropriate medications were given to the
which have been explained and demonstrated. The quality
patients but the information on the disease and proper
of topical medications' labels could also be improved with
usage of medications were not delivered to the patients.
the cooperation of the pharmacy department.
Our intervention included recruitment of a trained
dermatology nurse to explain regarding the disease and to
We found a positive effect of explanation and
demonstrate to the patients and/or parents on how to apply
demonstration of topical therapy on the clinical response of
the topical medications. The patients were taught on the
atopic eczema as evidenced by a significant reduction of
correct time, frequency, sites of applications, duration of use
disease severity score (SASSAD) as well as improvement in
and the potency of the topical corticosteroid prescribed.
itch, sleep disturbances and irritability. This study reinforcesthe importance of having a trained dermatology nurse to
As reinforcement, all the topical medications were labeled
explain and demonstrate on proper usage of topical
with multi-languages cartoon labels and patient
applications in the management of atopic eczema. We
information leaflets on atopic eczema available in 3
suggest that all dermatology clinics utilize the services of
languages were also given to the patients. We also spent
these nurses especially in cases when the doctors themselves
some time answering to any queries from patients/parents.
cannot afford to spend more time with the patients due totheir busy schedule. Failure to explain on how to use topical
There was an improvement in the disease severity in Group
applications may lead to patient dissatisfaction, poor
A as evidenced by a significant reduction of SASSAD score
compliance and lack of treatment efficacy.
when proper education and demonstration on how to applytopical treatments were given during the first visit as
compared to Group B, where the consultation was done in
We thank the QAP committee of Ipoh Hospital in
the usual manner but without further education or
supporting this study and all the staff of the Department of
demonstration. This significant reduction was reproducible
Dermatology, especially staff nurse Kong Siew Hong, for
in Group B at the third visit when similar education and
their cooperation and commitment.
Appendix 1. The Six Area, Six Sign Atopic Dermatitis (SASSAD) severity score
Six Signs: Erythema, Exudation, Excoriation, Dryness, Cracking, and Lichenification
Six Sites: Arms; Hands; Legs; Feet; Head & neck; and trunk
Grade of severity (Range of score: 0-108)
The sign cannot be detected with certainty even after careful inspection
The sign is certainly present but requires careful inspection to see it
The sign is immediately apparent
The sign is very prominent
Malaysian Journal Of Dermatology Jurnal Dermatologi Malaysia
Basak PY, Ozturk M, Baysal V. Assessment of information and education about topical corticosteroids in dermatology outpatient departments: experience from Turkey. J Eur Acad
Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis.
Dermatol Venerol 2003;17: 652-658
Acta Derm Venereol (Stockh) 1980; Suppl 92: 44-47.
Beattie PE, Lewis-Jones MS Parental knowledge of topical
Berth-Jones J. Six area, six sign atopic dermatitis (SASSAD)
therapies in the treatment of childhood atopic dermatitis. Clin
severity score: a simple system for monitoring disease activity
Exp Dermatol 2003; 28: 549-553.
in atopic dermatitis. Br J Dermatol 1996; 135: 25-30.
Charman C.R., Morris A.D., Williams H.C. Topical corticosteroid
Broberg A, Kalimo K, Lindblad B et al. Parental education in the
phobia in patients with atopic eczema. Br J Dermatol 2000; 142:
treatment of Childhood atopic eczema. Acta Derm Venereol
(Stockh) 1990;70: 496-9.
Cork MJ, Britton J, Butler L et al. Comparison of parent knowledge, therapy utilization and severity of atopic eczema before and after explanation and demonstration of topical therapies by a specialist dermatology nurse. Br J Dermatol 2003;149: 582-589.
Source: http://www.dermatology.org.my/pdf/journal%202007B.pdf
Florida State College at Jacksonville Assessment Data by Section 2011-2012 Academic Success Center Student Learning Outcomes/Objectives SLO 2: Effective Advising Services The Academic Success Centers effectively provide advising services for developmental students seeking academic and personal assistance at each campus and center.
Journal of Engineering and Technology DEVELOPMENT OF SIMVASTATIN PRODUCTION BY MONASCUS PURPUREUS IN SOLID-STATE FERMENTATION USING AGRICULTURAL PRODUCT Faculty of Chemical and Natural Resources Engineering, Universiti Malaysia Pahang, 25000, Kuantan, Pahang, Malaysia ABSTRACT Monascuspurpureus is a non-pathogenic fungus that can produce statin called simvastatin, which can lower blood cholesterol level. The objectives of this research were to explore the potential of agricultural product on simvastatin and identify the optimal condition of simvastatin production in solid-state fermentation by Monascuspurpureus FTC 5356. The local agricultural products used were banana, guava, pumpkin, coconut meat, corn and papaya. Initially, the local agricultural products were ground and the initial moisture content of the agricultural products was fixed at 50% and pH 6. The mixtures were then incubated at 30°C for 11 days. Later, variety conditions of initial moisture content and nitrogen supplementation were introduced and examined on the simvastatin. Further experimental work was carried out using Central Composite Design (CCD) of Response Surface Methodology (RSM), with two factors of initial moisture content and nitrogen source. The results suggested that, among the agricultural products tested; only corn powder was able to produce simvastatin. The optimal condition for simvastatin production on corn was at 50% initial moisture content with supplementation of 0.2% nitrogen source.