Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Heartjnl214031 6.14
Controversies in the cardiovascular management oftype 2 diabetes
Lionel H Opie,1 Derek M Yellon,2 Bernard J Gersh3
1Hatter Cardiovascular Research
low-density lipoprotein cholesterol (LDL-C) from
Institute, Department of
In patients with type 2 diabetes mellitus, intense control
about 3.1 mmo/l (118 mg/dl) to 1.94 mmol/l
Medicine, Faculty of Health
of blood pressure, lipids and glucose, aiming at
(72 mg/dl), and decreased major cardiovascular
Sciences, University of Cape
theoretically ideal values, is bought at a cost. Intense
events, including stroke reduction, by 48%. In the
Town, Observatory, Cape Town,South Africa
blood pressure control has renal complications. Intense
diabetic subgroup of a subsequent large meta-
2The Hatter Cardiovascular
lipid control, thus far, has worked for reduction of
analysis, decreasing LDL-C by 1 mmol/l (about
Institute, University College
low-density lipoprotein-cholesterol, paradoxically at the
40 mg/dl) reduced the calculated major vascular
London Hospital and Medical
cost of a small increase in new diabetes. Intense control
events by 21% irrespective of the starting value.3
School, London, UK3Mayo Clinic College of
of glycaemia generally requires insulin added to oral
Overall, these observations suggest, but do not
Medicine, Division of
agents, which is consistently accompanied by weight
prove, that the higher the statin dose and the lower
Cardiovascular Diseases, Mayo
gain, while increased hypoglycaemia has a long-term risk
the LDL-C value, the better the outcome. There
Clinic, Rochester, Minnesota,
of cerebral damage. Intense glycaemic control has not
still is need for a prospective study in patients with
consistently reduced mortality, whereas a strategy
DM2 at relatively low cardiovascular risk to
Correspondence to
based on tight control of lipids and blood pressure with
confirm the benefit of further decreasing LDL-C.4
Professor Derek M Yellon, The
modestly tight glucose control has succeeded. Looking
Hatter Cardiovascular Institute,
to the future, incretin mimetics may come to the fore as
New side effects, including diabetes, evoked by
University College London
prime agents because they can reduce weight and
Hospital and Medical School, 67Chenies Mews, London WC1E
glycaemia with little significant hypoglycaemia, thereby
Besides the well-known statin-related side effects
6HX, UK;
[email protected]
making tight glucose control easier to achieve.
such as myalgia and altered liver function, tworecently identified problems are increased cataract
Accepted 11 October 2010
formation and acute renal failure.5 According toa newly proposed algorithm, using data obtainedon over 2 million patients soon after the onset of
statin treatment, three of these side effects
In regard to risk factors for the development of
(moderate to severe myalgia, liver dysfunction and
cardiovascular disease in patients with type 2
cataracts) could be predicted with reasonable
diabetes (DM2), the fundamental message was
accuracy.5 The number needed to harm for acute
delivered by the large and ongoing United Kingdom
renal failure were 434 over 5 years to cause one
Prospective Diabetes Study (UKPDS). The major
additional case. For myopathy the number needed
factor was the ratio of total cholesterol to high-
to harm was 259, for liver dysfunction it was 136
density lipoprotein cholesterol (HDL-C), which
and for cataract only 33. The rather rare renal side
accounted for 45% of the risk.1 Next came the
effects, thus far not well recognised, include acute
significance of systolic blood pressure (SBP),
renal failure besides increased proteinuria, and
accounting for 33% of the risk while last was the
could not be predicted. Simvastatin was by far the
glycosylated haemoglobin (HbA1c) at 22%. We will
most frequently prescribed drug followed by ator-
review controversies, starting with those that are
vastatin. The unexpected advent of new diabetes as
more modest in relation to lipid control and BP
a side effect still makes statin treatment desirable
management, followed by major controversies in
for all with DM2, while watching for an increasing
relation to glycaemic control. An intuitively logical
HbA1c level.4 6 However, in view of the persisting
hypothesis would be that the more normal each of
residual cardiovascular risk despite statin treat-
these three factors is, the better the clinical
ment, would additional co-therapy with fibrates
outcome (figure 1). Yet some recent studies have
give added benefit?
cast doubt on the simplicity of the direct straightline type of relationship and rather argue for
Fibrates give modest benefits beyond statins
a trough or U-shaped curve with a dip which could
High blood triglyceride levels are an independent
be the optimal range.
risk factor for coronary heart disease, albeit not forstroke.7 Fenofibrate, the peroxisome proliferator-
LIPID CONTROL: EXTENDING BEYOND STATINS?
activated receptor (PPAR) a agonist, when added
Present evidence supports the use of statin treat-
to pre-existing statin treatment in DM2 decreased
ment in all patients with DM2. The crucial study
the triglyceride values and slowed retinopathy
was the Collaborative Atorvastatin Diabetes Study
progression.8 In the larger FIELD study over 5 years
(CARDS) study, in which the entry criteria were
on 9795 people with DM2, fenofibrate similarly
DM2 and at least one other cardiovascular risk
reduced triglyceride levels.9 Coronary revascularisa-
factor such as hypertension, smoking or diabetic
tion rates fell by 21% (p¼0.003) with less albu-
complications (retinopathy or maculopathy, micro-
minuria progression and less severe retinopathy. The
or macroalbuminuria).2 Atorvastatin reduced the
costs were pulmonary embolism, and a consistent
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
Lipids: SummaryAt present, intense LDL-C lowering by a statin remains thecornerstone of lipid-lowering treatment despite newly reportedside effects. To reduce triglyceride levels and/or to delay reti-nopathy, the best evidence is for fenofibrate added to statins.
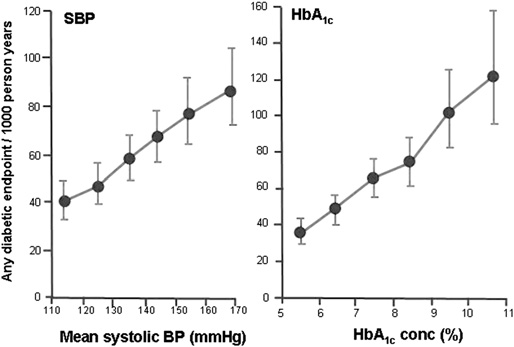
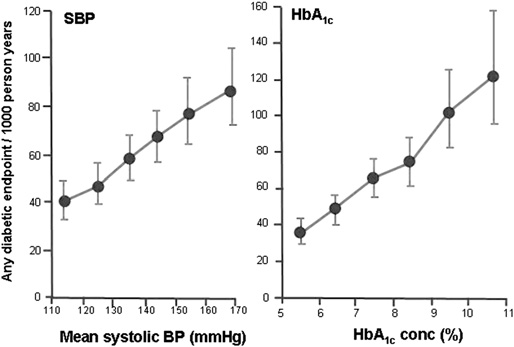
BLOOD PRESSURE CONTROL: HOW LOW TO GO?The controversy: What is the ideal systolic BP in DM2?In an observational cohort study from the UKPDS series,suggesting an optimal SBP of about 110e120 mm Hg, as the SBPfell from >160 mm Hg to <120 mm Hg, there were lineardecreases in MI, stroke and microvascular disease.17 The conclu-sion was that for each 10 mm Hg reduction in blood pressurethere was a 12% decrease in mortality. The lower, the better itseemed (figure 1). However, subsequent trial data did not supportthese predictions.18e20 There are plausible reasons for the devia-
Population studies yield a near-straight line relationship
tion from the straight line shown in figure 1. In the UKPDS
between any diabetic end point and, on the left, the mean systolic blood
observational study (see left panel in Table 1 of reference17) the
pressure (SBP) and, on the right, the glycated haemoglobin (HbA1c)
participants were younger with a lower body mass index, and the
level. However, these observational data appear not to be based on
diabetes was newly diagnosed versus 10 years in ACCORD.
prospective trial information, with which they conflict. Figures modifiedwith permission from the
These factors could differentiate the two studies. and account for
British Medical Journal, on the left for systolic
blood pressure (Adler AI, et al. BMJ 2003;321:412) and on the right for
the straight-line relationship in figure 1. From the ACCORD
the HbA1c level (Stratton IM, et al. BMJ 2000;321:405).
study,19 the main conclusion to draw must be that a SBP target
<120 mm Hg in patients with DM2 is not justified by theevidence. For ADVANCE, the initial mean BP was 145/81mm
and puzzling reversible increase in plasma creatinine of
Hg, which decreased by 5.6/2.2 mm Hg to a mean of 139/
10e12 mmol/l.9 Overall, fibrates may be indicated with statins if
79mm Hg,18 almost exactly where ACCORD started from (139/
the lipid profile in DM2 demonstrates an increased triglyceride
76 mm Hg). That difference may explain why renal outcomes
level, with the aim of delaying retinopathy. The largest database
were improved as the BP fell in ADVANCE and the BP fall was
is for fenofibrate. However, the benefits of exercise and weight
well tolerated.21
loss on both triglyceride levels and cardiovascular events shouldnot be forgotten.
Practical policy for BP controlInitial data came from UKPDS 38, wherein a mean BP of
Bezafibrate, a combined PPARa and PPARg agonist
154/97 mm Hg to 144/82 mm Hg over a mean of 8.4 years
This combination of PPARa and PPARg agonist effects is
reduced all diabetes-related end points by 24%.22 More current
attractive because the added g agonism activates glucose
studies argue for a SBP <140 mm Hg in DM2, within the band
metabolism to reduce plasma glucose concentrations, while the
component increases HDL-C.10 In non-diabetic patients with
e140 mm Hg,20 as also found in ADVANCE.18 ACCORD
does not support <120 mm Hg.19 In hypertensive patients with
coronary artery disease (CAD) bezafibrate reduced new DM2 by
diabetes and CAD, INVEST does not support <130 mm Hg.20
30% over 6.2 years.10 However, these data antedated the wide-
Thus the major studies do not support the linear relation
spread use of statins and ACE inhibitors and need to be
between BP and any diabetic end point as suggested by the
confirmed in the current era.
UKPDS observational study in figure 1. There were few patientsin ACCORD with previous stroke, so our recommendations of
Increasing HDL-C, niacin and thiazolidinediones
HDL-C is often low in DM2 and its normal vasoprotective
e140 mm Hg cannot be applied directly to this
group. Furthermore, much depends on clinical judgement
effects are impaired.11 Nicotinic acid (niacin) would logically be
applied to the individual patient. For example, in selected
the preferred treatment but is poorly tolerated. The recently
patients, the BP aim could even be 125 mm Hg if it were easy
introduced long-acting formulation (Niaspan) elevates HDL-C
to achieve without multiple drugs. In summary, in BP control
in DM2 and increases the endothelial-protective effects.11
there is conflict between the idealised observational data that
Thiazolidinediones, also called the ‘glitazones', are drugs that
predict a straight-line relationship between decreases in BP and
activate the PPARg transcriptional system thereby promoting the
CV disease (figure 1),17 and the practical reality of controlled
metabolism of glucose, while having indirect PPARa stimulating
therapeutic trials.
properties thereby reducing both glycaemia and triglycerides,while increasing HDL-C.12 Rosiglitazone and pioglitazone bothincreased total LDL-C but to a greater extent with rosiglitazone,
GLYCAEMIC CONTROL: GLUCOTOXICITY VERSUS LIPOTOXICITY
which increased LDL-C particle concentration, whereas pioglita-
Optimal glycaemic control is correctly stressed by major
zone reduced it.13 Pioglitazone increased total HDL-C particle
diabetes societies, while often emphasising HbA1c levels of
concentration and size, whereas rosiglitazone decreased them;
<7.0% or, sometimes, <6.5%. Supporting this view is the
nonetheless both increased HDL-C cholesterol. Experimentally,
apparent straight-line relationship between HbA1c and any
pioglitazone reduced infarct size.14 Overall, these observations
diabetic end point in DM2 (figure 1) and the concept of an
might help to explain why rosiglitazone but not pioglitazone
optimal HbA1c of about 3.9e5.59% as found in 260 361 people
monotherapy has been associated with increased myocardial
with no known diabetes.23 Logically, reversal of the abnormali-
infarction (MI) in some but not all studies.15 16 (See later for
ties of glucose metabolism found in DM2 should be the key to
thiazolidinediones and heart failure (HF).)
improving prognosis. However, an equally fundamental problem
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
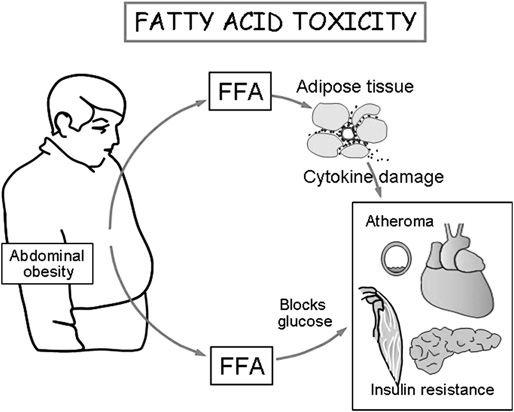
might lie in the increased circulating levels of potentially toxicfree fatty acids (FFAs), released from abdominal fat to promoteinsulin resistance.24 The result is decreased uptake of glucose bybody tissues including muscle and liver, which explains thehyperglycaemia of DM2.
The glucoseefatty acid cycle and fatty acid toxicityIn a classic article in 1963, Randle et al described the glucoseefatty acid cycle, whereby an alternating interaction betweenglucose and FFA metabolism could explain metabolic abnor-malities in obesity and diabetes.25 In hearts perfused with FFAsand glucose, glucose oxidation is inhibited,26 because glycolysisis blocked, while increased levels of glucose and insulin inhibitthe release of FFAs from adipose cells.25 These mechanismsexplain why glucose is the dominant fuel of the heart in thepostprandial phase and FFA uptake dominates in fasting as theblood glucose falls Experimentally, glucose and/or insulin werecardioprotective27 and, conversely, high levels of FFAs harmfulto the heart.28
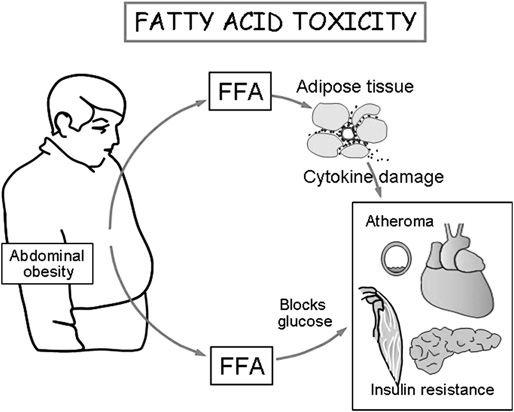
Adipose tissue mediates cytokine damage. Proposed role of
free fatty acid (FFA) in promoting cytokine-induced organ damage. For
Experimentally, high circulating FFA levels oppose the vaso-
data, see Shoelson SE, et al. J Clin Invest 2006;116:1793. Copyright LH
dilatory and protective role of the anti-atherogenic endothelial
nitric oxide (NO) molecule.29 Marked FFA elevation causesmitochondrial uncoupling and oxygen wasting, and cytokine-
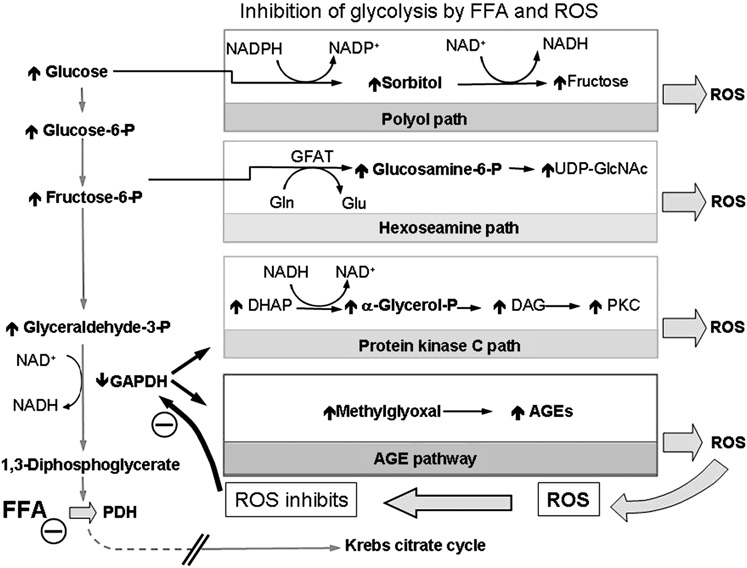
reactive oxygen species33 (figure 3). However, these experiments
induced organ damage.30 31 (figure 2) However, in DM2 there has
typically use external glucose values of 10e33 mmol/l
only been limited proof of FFA toxicity with increased muscle
glucose,34e41 all well above the limits of acceptable care in DM2.
lipid in biopsies from the vastus lateralis muscle.32 Logically, FFAcontrol should be a prime aim in DM2. The limitation is that
measuring circulating FFA levels remains a specialised procedure,
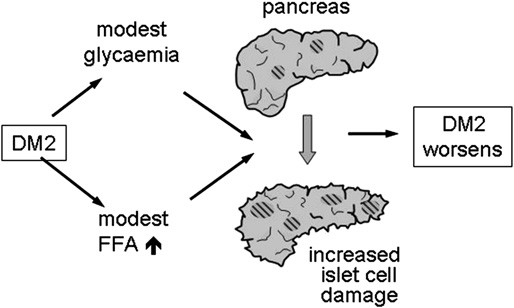
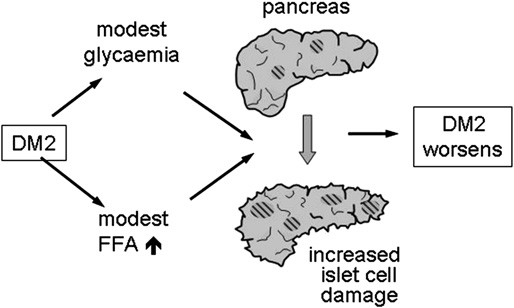
Taegtmeyer's group has emphasised the logical concept of
hence not a feasible target in controlling DM2.
combined glucotoxicity and lipotoxicity,33 34 whereby modestglycaemia and modest lipaemia adversely combine to increase
pancreatic damage (figure 4). The glycaemia may, through an
There is no doubt that experimentally high external glucose
unknown mechanism, downregulate PPARa activity, thereby
concentrations potentially promote tissue damage by stimu-
decreasing fatty acid oxidation and promoting the accumulation
lating the various glycolytic-dependent pathological paths, acti-
within the heart of damaging fatty acid derivatives such as
vated by blocked glycolysis, that lead to increased formation of
ceramide.33 Conversely increased circulating FFAs inhibit glucose
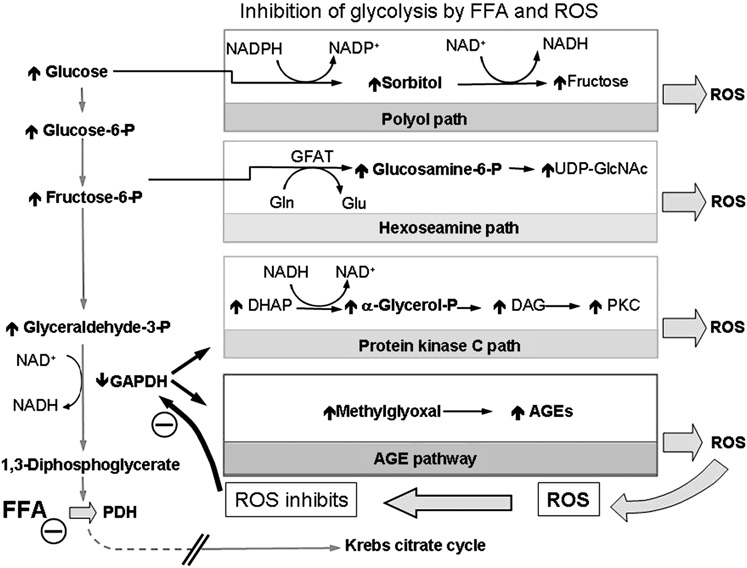
Proposed role of inhibition of
glycolysis in glucolipotoxicity.
Concurrent metabolism of elevatedblood levels of free fatty acids (FFAs) indiabetes mellitus type 2 inhibits cardiacglycolysis chiefly at the level ofpyruvate dehydrogenase (PDH),resulting in the accumulation ofglycolytic intermediates.25 The concepthere proposed is that further metabolicchanges induced by these accumulatedproducts of inhibited glycolysis increasethe formation of reactive oxygenspecies (ROS) at multiple levels,including feedback inhibition ofglycolysis at the level of glyceraldehydephosphate dehydrogenase (GAPDH),thereby promoting a vicious circle.
AGEs, advanced glycation end products.
Modified with permission fromBrownlee M. Nature 2001;414:813.
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
hypoglycaemic death was actually lower in the arm receivingintense treatment than in the standard treatment arm. Thusthere could have been another ill-defined mechanism of death. Forexample, a post hoc and non-prespecified analysis of ACCORDhypothesises that there were systemic factors associated withpersisting HbA1C values $7, such as serious associated medical orsocial or cognitive problems beyond DM2.51 This elegant conceptneeds further testing by prospective studies.
Benefit versus harm of tight controlThere is no crucial clinical evidence that tight control of presetaims, such as HbA1c of 7.0% or even lower, gives a clear-cutbenefit to those with established DM2. Thus the predictedstraight-line relation between the HbA1C and all diabeticoutcomes, shown in figure 1, is not supported by several major
Proposed mechanism whereby modest glucolipotoxicity can
studies.52 Tight control might be more beneficial in the very
promote pancreatic damage and increase the severity of diabetes
early management of recently diagnosed DM2 as suggested by
mellitus type 2 (DM2). FFAs, free fatty acids. Copyright LH Opie, 2010.
UKPDS 3353 but requires prospective randomised testing, as isnow planned. Tight control in four major trials, ACCORD,49
oxidation at the level of entry of pyruvate into the Krebs cycle
UKPDS 33,53 VADT54 and ADVANCE,55 found large increases in
thus leading to accumulation of glycolytic intermediates that in
the relative risks of severe hypoglycaemic episodes and weight
turn promote the formation of advanced glycation end products
gain. All-cause and cardiovascular mortality only improved in
and reactive oxygen species (figure 3). In clinical practice, studies
one of the four studies; there were no changes in stroke,
in patients with DM2 show that agents such as incretins and
amputation or other peripheral vascular events, and none in
pioglitazone control both glycaemia and FFA levels with
neuropathy, progress to macular oedema, visual deterioration or
decreased oxidative stress42 and improved muscle fat metabo-
blindness; and only a borderline benefit for renal mortality or
lism,32 thereby extending the control DM2 beyond blood FFA
renal replacement as found in the other studies.52 However, non-
and glucose levels.
fatal MI was less and the risk of MI fell by 15%.56 By contrast,metformin clearly improved clinical outcome without severe
HYPOGLYCAEMIC REACTIONS DURING TIGHT GLUCOSE
hypoglycaemia and weight gain.52 57
At present, we have found no convincing evidence in clinical
Adverse side effects of antidiabetic drugs
practice that allows extrapolation directly from modest
The perils of hypoglycaemia and weight gain are self-evident. In
increases in the blood HbA1c or glucose values to metabolic
general, the possible long-term cerebral complications of hypo-
harm for patients with DM2. Rather, a very large real-life
glycaemia43 have not been carefully studied. The overall
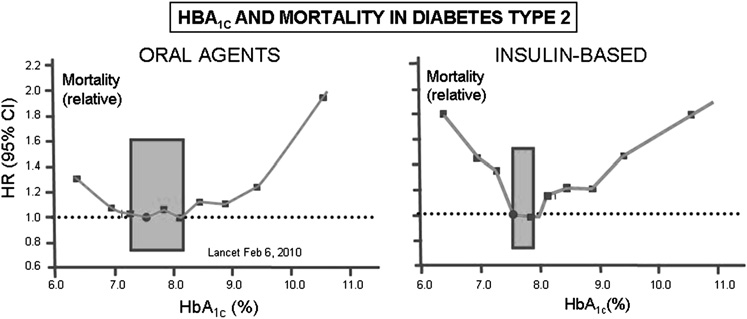
observational general practice study suggests a range of optimal
improved control of DM2 may promote longevity,44 45 but at
HbA1c values somewhere between 7.5% and 8.9% for non-
the possible price of the greater potential threat of serious
insulin treatments and a tighter band for insulin-based treat-
cognitive loss since function of the brain is a glucose-requiring
ments between 7.5% and 8%.58 Overall, HbA1c 7.5% was the
organ.46 Thus the brain may be vulnerable to repetitive hypo-
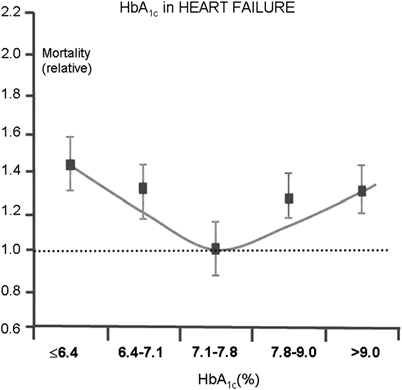
value that optimally reduced mortality (figure 5). Furthermore
glycaemic attacks. In elderly patients with DM2, multiple
a similar U-shaped pattern was found in a study on patients
episodes of hypoglycaemia had a graded risk for dementia after
with DM2 and HF in a USA teaching hospital (figure 6).
27 years of follow-up, the HR for three episodes versus none
Overall, the aim should be to select treatment combinations
being 1.94 (CI 1.42 to 2.64).43 It would be contradictory and
that reduce MI, hypoglycaemia and glycaemia and weight gain.
catastrophic if achieving an HbA1c of <7.0% came at the cost of
On available evidence, we would commend the multifactorial
impaired brain function.
approach (next section).
There are striking differences in the incidences of serious
hypoglycaemia, generally linked to insulin use, in major trials.
MULTIFACTORIAL APPROACH
The ADVANCE study achieved a low HbA1c of 6.5% with the
The STENO-2 study
use of cardioprotective gliclazide,47 with added insulin in about
This trial showed the benefits of multifactorial intervention.42
half.18 The fall of HbA1c during intensified treatment was slow,
After a mean of 7.8 years of intensive treatment, the SBP fell
taking several months, suggesting careful and unhurried clinical
from 147 mm Hg to 130 mm Hg. LDL-C and triglyceride values
observation, which may explain why hypoglycaemia was
dropped to within the goals in most patients. Fasting lipid goals
uncommon. The controlled randomised trial, UKPDS 34, found
were: cholesterol level <4.5 mmol/l (175 mg/dl) and triglyceride
that metformin, giving a mean HbA1c of 7.4%, substantially
level <1.7 mmol/l (150 mg/dl). Nonetheless, there were signifi-
reduced mortality and caused less weight gain and less hypo-
cant reductions in both microvascular and macrovascular
glycaemia than sulphonylurea treatment or insulin.48 By
complications, including nephropathy (p¼0.003), retinopathy
contrast, in ACCORD the rate of fall of HbA1c was much more
(p¼0.02) and autonomic neuropathy (p¼0.002), with an abso-
rapid and the incidence of hypoglycaemia much higher.49
lute 20% reduction in cardiovascular disease and a relativereduction of 53% (HR¼0.47, CI 0.24 to 0.73; p¼0.008). With the
Implications of hypoglycaemic reactions during tight control
multifactorial approach in STENO-2, unexpected benefits
In a retrospective analysis of the ACCORD study,50 the associa-
became apparent at the end of a further prolonged follow-up
tion between severe hypoglycaemia and mortality was examined.
However, the unexpected finding was that, taking all those with
Strikingly, attempts at glycaemic control were unable to reach
at least one episode of hypoglycaemia in ACCORD, the risk of
the aim of <6.5% HbA1c, achieved in only 15% of patients
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
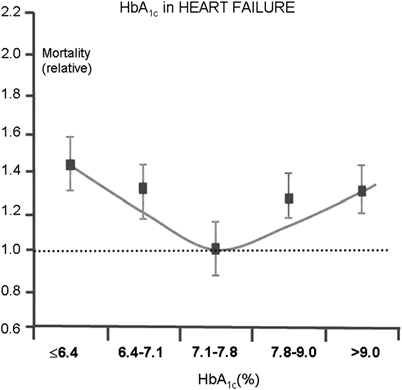
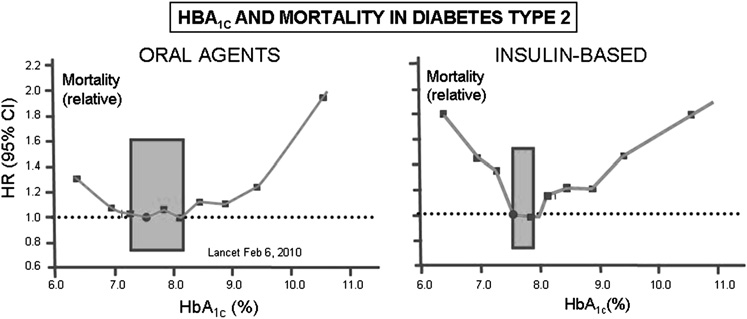
Relative mortality and
glycated haemoglobin (HbA1c) levels intype 2 diabetes in a large UnitedKingdom general practice observationalstudy.58 Note the narrow protectiveband of HbA1c values with use of oralantiglycaemic agents (left) and insulin(right). On the left are the results withoral agents, suggesting a relatively flatplateau of optimal HbA1c levelsbetween approximately 7.3 and 8.2%.
On the right are the data forinsulin-based treatment, suggestinga smaller plateau of optimal benefit,round about 7.5e8% HbA1c. ‘Safe'zones are designated by the shadedareas. Figure modified with the permission ofThe Lancet from Currie et al. Lancet 2010;375:481e9.
receiving intensive treatment. The actual mean values for the
Increased HF with thiazolidinediones
HbA1c in the intensive group were 8.4% initially and 7.9% at the
A series of meta-analyses 61e63 has confirmed a higher incidence
end of the intervention study, reaching 7.7% at the end of
of cardiac complications, such as congestive heart failure or MI.
follow-up. These values give no support for the concept that the
In ADOPT rosiglitazone was associated with more cardiovas-
ideal HbA1c of 6.5 or 7.0% had to be achieved to obtain major
cular events, specifically HF, and bone fractures than glyburide.64
outcome benefit. Rather the benefit of triple therapy by
Hence the boxed warning in the USA package insert which
a reasonable degree of glycaemic control, with reasonably tight
states that thiazolidinediones are not recommended in any
SBP control to 130 mm Hg and tight lipid control was associated
symptomatic HF.
with the long-term reduced mortality.
Comparing pioglitazone with rosiglitazone, the latter is
associated with a 25% increase in the risk of HF and 14%
DIABETES AND HEART FAILURE
increased mortality according to an influential study emanating
Heart failure is a common comorbidity in DM2. Mechanistically,
from the American Federal Drug Agency.65 As this detailed study
insulin resistance promotes progression of HF.59 In the large UK
was of 227 571 Medicare patients aged $65 years, there seems to
General Practice Research Database, standard anti-HF drugs
be no compelling reason for the use of rosiglitazone by cardiol-
reduced mortality. By contrast, metformin was the only anti-
ogists taking care of elderly patients with DM2. Note that the
glycaemic agent associated with decreased mortality (OR¼0.72;
majority of patients were above 70 years old, while 90% had
CI 0.59 to 0.90).60 The thiazolidinediones were seldom used in
hypertension and 37% cardiovascular diseases before thiazolidi-
general practice, and are the only class of antidiabetic agents
nedione treatment. By contrast, another recent study found
with adverse data for HF.
equal event rates with the two thiazolidinediones in 36 628people of mean age 54 years with full healthcare, of whom <4%had had previous cardiovascular events.66 Thus one feasibleproposal is that pioglitazone has the edge for safety data in anelderly population, whereas both drugs have equal effects whengiven to relatively healthy middle-aged populations. In middle-aged people with DM2 and a normal ejection fraction (60%),pioglitazone improved diastolic dysfunction while increasingwhole-body insulin sensitivity and myocardial glucose uptake.67
Paradoxical myocardial beneficial effects of rosiglitazonerelevant to HFEven when HF is precipitated by pioglitazone, mortality andmorbidity are not increased.68 The simplest explanation for thisapparent paradox may be that there is only fluid retention andnot congestive HF.69 There are two PPARg-independent cardiaceffects of pioglitazone. First, pioglitazone experimentally atten-uates angiotensin-induced cardiac fibrosis by inhibiting myocar-dial macrophage infiltration, thereby lessening cardiac fibrosis,which is one the causes of left ventricular (LV) dysfunction.70Second, pioglitazone may beneficially lessen the accumulation of
Relation between initial HbA1c and 2-year mortality, studied
harmful saturated FFAs in the myocardium.32 67
in 5815 patients with heart failure in an Veterans Affair USA academiccentre. Proportion of diabetic patients who had died by 2 years of
Other antidiabetic drugs and HF
follow-up in relation to initial HbA1c values. Calculated from data infigure1 of Aguilar D,
Metformin, beneficial in the UK General Practice study55 and
et al. J Am Coll Cardiol 2009;54:422e8; for
limitations of study, see Weinrauch LA and Lewis EF. J Am Coll Cardiol
experimentally,71 needs direct prospective comparative studies
to prove its anti-HF benefits.
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
Ranolazine, currently available in the USA and Europe,
coronary artery bypass grafting (CABG) or percutaneous coro-
improves the diabetic status of patients with acute coronary
nary intervention (PCI) versus medical treatment with regard to
syndrome.72 Experimentally, when combined with enalapril or
death and MI.
metoprolol, it slows the progression of HF.73 By Na+/Ca+
We emphasise that randomisation occurred after angiography
exchange inhibition, ranolazine improves diastolic function in
and that these were stable patients with mild to moderate
myocardium taken from failing human hearts.74 These effects of
symptoms, or patients who were asymptomatic with positive
ranolazine warrant prospective trials in patients with DM2 with
stress tests, but nonetheless with an event rate as high as 20% at
diastolic HF.
4 years. In cost-conscious situations, cardiologists often firstemploy clinical assessment and a variety of stress tests, whichprovide a different entry point. A trial of a strategy of inter-
DIABETIC CARDIOMYOPATHY
vention versus medical treatment in patients enrolled at the
The existence of this previously controversial entity, diabetic
time of stress testing is currently in the design phase (Marron D,
cardiomyopathy, has been put beyond reasonable doubt by
Williams D and Hichman J; personal communication).
recent laboratory and clinical studies.69 75 76 Diabetic cardio-myopathy was originally described as a specific diabetes-relatedform of myocardial dysfunction often starting as diastolic
Coronary revascularisation in patients at higher risk but with
dysfunction.77 Excess storage of myocardial triglyceride (cardiac
steatosis) in association with diastolic abnormalities precedes LV
Outcomes with both PCI and CABG are substantially less useful
systolic dysfunction.76 This is yet another complication of
among diabetic than non-diabetic patients. The general princi-
excess FFA supply in diabetes, so that the logical preventive
ples of glycaemic control hold for management of diabetic
treatment could include early use of incretins or pioglitazone.
patients undergoing PCI, for whom an added hazard is an
Preclinical diabetic cardiomyopathy has now also been proposed
increased risk of restenosis.88 Multiple randomised controlled
as the combination of diabetes and echocardiographic diastolic
trials have demonstrated no difference in death or MI between
dysfunction in the absence of prior hypertension or ischaemic
CABG and PCI with the exception of diabetics entered into the
heart disease.78 On follow-up, previous diastolic dysfunction
BARI-2D trial, in which mortality was lower in patients treated
was associated with a lower event-free survival, 54% versus 87%
with CABG than for those undergoing percutaneous trans-
in controls (p¼0.001). Overall, diabetic cardiomyopathy still
luminal coronary angioplasty.86 89
warrants further therapeutic study and clarification.
Our proposed explanation is that clinical judgement and
doctor preference resulted in higher-risk patients being treatedsurgically. In the BARI-2D trial, those patients with more
DM2 AND CORONARY HEART DISEASE
complex anatomy were more likely to undergo CABG, which
DM2 and coronary artery disease
was associated with a reduction in non-fatal MI in comparison
Here there is little controversy. The Euro Heart Survey found
with medical treatment. Likewise in the SYNTAX trial of
that of patients with acute CAD, 36% had abnormal oral glucose
patients with three-vessel disease, including left main CAD,
tolerance tests (OGTT) and 22% newly detected diabetes.79
there was a clear benefit from CABG with a lower mortality and
In those with stable CAD, the percentages were 37% and
a markedly lower rate of repeat revascularisation among patients
14%. These glucose abnormalities detected by the OGTT
with the most extensive and complex anatomical coronary
were more closely linked to CAD than were fasting plasma
disease.90 Thus both these trials deliver a clear message: in
glucose or HbA1c.80 The practical difficulties in carrying out
patients requiring intervention, the clinically ‘sicker' patients
routine OGTT then led to a gluco-metabolic index based on
with 3 vessel disease and more complex anatomical disease as
fasting plasma glucose, HDL-C and age to stratify the risks of
often found in diabetic subjects, are best served with CABG. The
further cardiovascular events in patients with CAD.81 The
other lesson to be learnt is that many patients with stable
overall message is that the diagnosis of CAD carries with it an
disease and mild to moderate symptoms can be managed
obligation to search for underlying DM2. Furthermore, there is
medically. The trial that needs to be done, now in the planning
no question that those with DM2 and CAD must have glucose-
phase, is to compare revascularisation with medical treatment in
lowering treatment.82 Do all those with DM2 and no symptoms
patients with stable disease and mild symptoms but severe
of CAD need screening by myocardial perfusion imaging? The
‘ischaemia' on stress testing.
answer is ‘no', with the important caveat that this was a trial oflower-risk patients with specific inclusion and exclusion criteria.83
With so much changing, can we be dogmatic?This question applies to all of the controversies raised, perhaps
Intervention in stable coronary artery disease
especially to the tightness of glycaemic control. There are many
Acute coronary syndrome and hyperglycaemia in acute MI have
unresolved problems, all of which are currently in evolution:
recently been reviewed,84 85 so that we are focusing on stable
(a) the impact of primary and secondary prevention trials
CAD. As is the case with views on non-diabetic subjects, the
including very early glycaemic control; (b) the impact of ongoing
management of patients with stable mild to moderate angina or
trials of new surgical and percutaneous techniques; (c) the
who are asymptomatic with positive stress tests remains
selection of patients for coronary intervention; (d) new chal-
a source of controversy and vigorous, often polarised, debate.
lenges introduced by the risks and benefits of such intervention
The 5-year outcomes of the recent trial, Bypass Angioplasty
in an increasingly older population with multiple comorbidities
Revascularization Investigation in type 2 Diabetes (BARI-2D)
and (e) the longer-term cardiovascular consequences and impact
on 2368 patients with type 2 diabetes undergoing coronary
of the diabetes pandemic.
angiography, support the conclusions of an earlier trial onpredominantly non-diabetic patients (33.5% diabetics).86 87These studies strongly suggest that in angiographically selected
FUTURE CONTROVERSY: INCRETINS TO THE RESCUE?
patients with chronic stable angina and preserved LV function
Tight glycaemic control may bring in its wake complexity of
there is no overall benefit from coronary revascularisation with
treatment, hypoglycaemia, weight gain and increased costs, all
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
for benefits that may be certain. Is it now time for ‘an evidence-
Acknowledgements The stimulus to this article was the 2010 meeting on
based about-face' as argued in a provocative article from the
Cardiology and Diabetes at the Limits in Cape Town, South Africa. However, theviews here expressed are those of the authors.
Mayo Clinic?52 We would agree. It is increasingly realised thathypoglycaemia is the major downside of tighter control that
Competing interests None to declare.
offsets a relatively small cardiovascular mortality reduction.56
Provenance and peer review Not commissioned; externally peer reviewed.
Thus it would be logical to turn to agents such as the incretinswhich, in general, avoid hypoglycaemia and lead to loss rather
than gain of weight and may directly protect the pancreas by
Stevens RJ, Kothari V, Adler AI, et al. The UKPDS risk engine: a model for the risk of
lessening apoptosis.91 Incretin mimetics, which are glucagon-like
coronary heart disease in Type II diabetes (UKPDS 56). Clin Sci (Lond)
peptide-1 receptor agonists, include exenatide and liraglutide,
while incretin enhancers such as sitagliptin and vildagliptin are
Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention ofcardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative
inhibitors of the enzyme dipetidylpeptidase-4 that degrades
Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled
glucagon-like peptide-1. In obese patients with DM2, exenatide
trial. Lancet 2004;364:685e96.
once weekly added to metformin over 26 weeks gave better
Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-loweringtreatment: prospective meta-analysis of data from 90,056 participants in 14
control of glycaemia without any major hypoglycaemia and
randomised trials of statins. Lancet 2005;366:1267e78.
with greater weight loss than with either sitagliptin or piogli-
Hippisley-Cox J, Coupland C. Individualising the risks of statins in men and women
tazone.92 The proportion of patients reaching a target HbA1c of
in England and Wales: population-based cohort study. Heart 2010;96:939e47.
<7% from an initial mean of 8.5% was nearly 60%, significantly
Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular eventsin men and women with elevated C-reactive protein. N Engl J Med
more than with sitagliptin or pioglitazone.92 The downside
was a greater incidence of nausea (24% with exenatide, 10%
Sattar N, Preiss D, Murray HM, et al. Statins and risk of incident diabetes:
with sitagliptin and only 5% with pioglitazone). Nonetheless,
a collaborative meta-analysis of randomised statin trials. Lancet 2010;375:735e42.
Patel A, Barzi F, Jamrozik K, et al. Serum triglycerides as a risk factor for
quality-of-life scores were equally high with exenatide and
cardiovascular diseases in the Asia-Pacific region. Circulation 2004;110:2678e86.
sitagliptin and better than with pioglitazone.
Ginsberg HN, Elam MB, Lovato LC, et al; ACCORD Study Group. Effects of
Larger and longer outcome studies on a wider groups of
combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 2010;362:1563e74.
patients are now required to assess whether in metformin-
Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy oncardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study):
resistant patients with DM2, the incretins will supplant stan-
randomised controlled trial. Lancet 2005;366:1849e61.
dard sulphonylureas and minimise the need for insulin, and,
Tenenbaum A, Motro M, Fisman EZ, et al. Peroxisome proliferator-activated
hopefully, have cytoprotective properties that go beyond glucose
receptor ligand bezafibrate for prevention of type 2 diabetes mellitus in patients withcoronary artery disease. Circulation 2004;109:2197
control.93 But that is a controversy that remains to be settled.
Sorrentino SA, Besler C, Rohrer L, et al. Endothelial-vasoprotective effects ofhigh-density lipoprotein are impaired in patients with type 2 diabetes mellitus but are
A FLEXIBLE POLICY TO PREVENT CARDIOVASCULAR DISEASE?
improved after extended-release niacin therapy. Circulation 2010;121:110e22.
Erdmann E, Dormandy JA, Charbonnel B, et al. The effect of pioglitazone on
Currently, there are voices, including ours, arguing for a policy of
recurrent myocardial infarction in 2,445 patients with type 2 diabetes and previous
flexible goals, bearing in mind that the three ACCORD studies
myocardial infarction: results from the PROactive (PROactive 05) Study. J Am Coll
for tight BP control (SBP <130 mm Hg),19 for tight glycaemic
control (HbA1c 6.5%, rather than 7.5% in the standard group),49
Deeg MA, Buse JB, Goldberg RB, et al. Pioglitazone and rosiglitazone have differenteffects on serum lipoprotein particle concentrations and sizes in patients with type 2
and for augmented lipid control in the combination lipid treat-
diabetes and dyslipidemia. Diabetes Care 2007;30:2458e64.
ment study,8 have all made a single pointdnamely, that it is not
Wynne AM, Mocanu MM, Yellon DM. Pioglitazone mimics preconditioning in the
a simple case of ‘the lower the better', but rather a case of
isolated perfused rat heart: a role for the prosurvival kinases PI3K and P42/44MAPK.
J Cardiovasc Pharmacol 2005;46:817
applying flexible goals.52 94 95
Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and
The recurrent problem of excess hypoglycaemia during tight
death from cardiovascular causes. N Engl J Med 2007;356:2457e71.
control is one of the clues to a certain liberalisation. For example,
Lipscombe LL, Gomes T, Levesque LE, et al. Thiazolidinediones and cardiovascular
in a physicians' statement of the American Diabetes Association
outcomes in older patients with diabetes. Jama 2007;298:2634e43.
Adler AI, Stratton IM, Neil HAW, et al; On behalf of the UK Prospective Diabetes
and a scientific statement of the American College of Cardiology
Study Group. Association of systolic blood pressure with macrovascular and
and the American Heart Association,96 despite regarding an
microvascular complications of type 2 diabetes (UKPDS 36): prospective
HbA1c level of $7% as ‘a call to action', this is immediately
observational study. BMJ 2000;321:412e19.
Patel A, MacMahon S, Chalmers J, et al. Effects of a fixed combination of
mollified: ‘this goal is not appropriate, or practical, for some
perindopril and indapamide on macrovascular and microvascular outcomes in
patients and clinical judgement based on the potential benefits
patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled
and risks of a more intensified regimen needs to be applied for
trial. Lancet 2007;370:829e40.
Cushman WC, Evans GW, Byington RP, et al; The ACCORD Study Group. Effects of
every patient'. As more directly put by Nilsson: ‘We learn from
intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med
the completed ACCORD study that flexible goals should prob-
ably be applied to the control of hyperglycaemia, blood pressure
Cooper-DeHoff RM, Gong Y, Handberg EM, et al; Tight blood pressure control and
and dyslipidaemia in patients with DM2, taking into account
cardiovascular outcomes among hypertensive patients with diabetes and coronaryartery disease. Jama 2010;304:61
individual clinical factors of importance.'94
de Galan BE, Perkovic V, Ninomiya T, et al. Lowering blood pressure reduces renal
In agreement with the principles of the UKDPS,1 relatively
events in type 2 diabetes. J Am Soc Nephrol 2009;20:883e92.
tight control of blood lipids and BP remain the two major
UKPDS 38; UK Prospective Diabetes Study Group. Tight blood pressure control andrisk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38.
risk factors to control in DM2. Control of glycaemia comes
Br Med J 1998;317:703e13.
third, yet also remains crucial. Glycaemic control should not be
Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose
bought at the cost of treatment-induced weight gain and
concentration, and risk of vascular disease: a collaborative meta-analysis of 102
hypoglycaemia, the latter with risk of long-term cerebral
prospective studies. Lancet 2010;375:2215e22.
Opie LH. Metabolic syndrome. Circulation 2007;115:e32e5.
complications. The incretins can contribute to glycaemic control
Randle PJ, Garland PB, Hales CN, et al. The glucose fatty acid cycle: its role in insulin
with little hypoglycaemia, yet achieving weight loss. The
sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1963:785e9.
substantial controversies in these areas will, hopefully, lead to
Shipp J, Opie LH, Challoner DR. Fatty acid and glucose metabolism in the perfusedheart. Nature 1961;189:1018
more future collaborative studies between cardiologists and
de Leiris J, Opie LH, Lubbe WF. Effects of free fatty acid and glucose on enzyme
release in experimental myocardial infarction. Nature 1975;253:746e7.
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
Opie LH. Effect of fatty acids on contractility and rhythm of the heart. Nature
Singh S, Loke YK, Furberg CD. Long-term risk of cardiovascular events with
rosiglitazone: a meta-analysis. Jama 2007;29:1189e95.
Imrie H, Abbas A, Kearney M. Insulin resistance, lipotoxicity and endothelial
Lago RM, Singh PP, Nesto RW. Congestive heart failure and cardiovascular death in
dysfunction. Biochim Biophys Acta 2010;1801:320e6.
patients with prediabetes and type 2 diabetes given thiazolidinediones:
Opie LH, Knuuti J. The adrenergic-fatty acid load in heart failure. J Am Coll Cardiol
a meta-analysis of randomised clinical trials. Lancet 2007;370:1129e36.
Nissen SE, Wolski K. Rosiglitazone revisited: an updated meta-analysis of risk for
Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest
myocardial infarction and cardiovascular mortality. Arch Intern Med Published Online
First: 28 Jun 2010.
Bajaj M, Baig R, Suraamornkul S, et al. Effects of pioglitazone on intramyocellular fat
Zinman B, Haffner SM, Herman WH, et al. Effect of rosiglitazone, metformin, and
metabolism in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab
glyburide on bone biomarkers in patients with type 2 diabetes. J Clin Endocrinol
Young ME, McNulty P, Taegtmeyer H. Adaptation and maladaptation of the heart in
Graham D, Ouellet-Hellstrom R, Macurdy T, et al. Risk of acute myocardial
diabetes: Part II: potential mechanisms. Circulation 2002;105:1861e70.
infarction, stroke, heart failure, and death in elderly Medicare patients treated with
Robertson RP. Chronic oxidative stress as a central mechanism for glucose toxicity
rosiglitazone or pioglitazone. JAMA 2010;304:411e18.
in pancreatic islet beta cells in diabetes. J Biol Chem 2004;279:42351e4.
Wertz DA, Chang CL, Sarawate CA, et al. Risk of cardiovascular events and
Nishikawa T, Edelstein D, Du XL, et al. Normalizing mitochondrial superoxide
all-cause mortality in patients treated with thiazolidinediones in a managed-care
production blocks three pathways of hyperglycaemic damage. Nature
population. Circ Cardiovasc Qual Outcomes Published Online First: 24 Aug 2010.
Tang WH, Cheng WT, Kravtsov GM, et al. Cardiac contractile dysfunction during
van der Meer RW, Rijzewijk LJ, de Jong HW, et al. Pioglitazone improves cardiac
acute hyperglycemia due to impairment of SERCA by polyol pathway mediated
function and alters myocardial substrate metabolism without affecting cardiac
oxidative stress. Am J Physiol Cell Physiol 2010;299:C643e53.
triglyceride accumulation and high-energy phosphate metabolism in patients with
Olson LK, Redmon JB, Towle HC, et al. Chronic exposure of HIT cells to high glucose
well-controlled type 2 diabetes mellitus. Circulation 2009;119:2069e77.
concentrations paradoxically decreases insulin gene transcription and alters binding
Erdmann E, Charbonnel B, Wilcox RG, et al. Pioglitazone use and heart failure in
of insulin gene regulatory protein. J Clin Invest 1993;92:514e19.
patients with type 2 diabetes and preexisting cardiovascular disease: data from the
Sugiyama Y, Murao K, Imachi H, et al. Calcium/calmodulin-dependent protein kinase
PROactive study (PROactive 08). Diabetes Care 2007;30:2773e8.
IV involvement in the pathophysiology of glucotoxicity in rat pancreatic beta-cells.
Basu A, Jensen MD, McCann F, et al. Effects of pioglitazone versus glipizide on body
Metabolism Published Online First: 26 Apr 2010. http://www.metabolismjournal.com.
fat distribution, body water content, and hemodynamics in type 2 diabetes. Diabetes
El-Assaad W, Joly E, Barbeau A, et al. Glucolipotoxicity alters lipid partitioning and
causes mitochondrial dysfunction, cholesterol, and ceramide deposition and reactive
Caglayan E, Stauber B, Collins AR, et al. Differential roles of cardiomyocyte and
oxygen species production in INS832/13 ss-cells. Endocrinology 2010;151:3061e73.
macrophage peroxisome proliferator-activated receptor gamma in cardiac fibrosis.
Monnier L, Mas E, Ginet C, et al. Activation of oxidative stress by acute glucose
fluctuations compared with sustained chronic hyperglycemia in patients with type 2
Shah DD, Fonarow GC, Horwich TB. Metformin therapy and outcomes in patients
diabetes. Jama 2006;295:1681e7.
with advanced systolic heart failure and diabetes. J Card Fail 2010;16:200e6.
Marfella R, Esposito K, Giunta R, et al. Circulating adhesion molecules in humans:
Chisholm JW, Goldfine AB, Dhalla AK, et al. Effect of ranolazine on A1C and glucose
role of hyperglycemia and hyperinsulinemia. Circulation 2000;101:2247e51.
levels in hyperglycemic patients with non-ST elevation acute coronary syndrome.
Bunck MC, Corner A, Eliasson B, et al. One-year treatment with exenatide vs.
Diabetes Care 2010;33:1163e8.
Insulin Glargine: Effects on postprandial glycemia, lipid profiles, and oxidative stress.
Rastogi S, Sharov VG, Mishra S, et al. Ranolazine combined with enalapril or
metoprolol prevents progressive LV dysfunction and remodeling in dogs with
Whitmer RA, Karter AJ, Yaffe K, et al. Hypoglycemic episodes and risk of dementia
moderate heart failure. Am J Physiol Heart Circ Physiol 2008;295:H2149e55.
in older patients with type 2 diabetes mellitus. JAMA 2009;301:1565e72.
Sossalla S, Wagner S, Rasenack EC, et al. Ranolazine improves diastolic dysfunction
Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose
in isolated myocardium from failing human heartserole of late sodium current and
control in type 2 diabetes. N Engl J Med 2008;359:1577e89.
intracellular ion accumulation. J Mol Cell Cardiol 2008;45:32e43.
Gaede P, Lund-Andersen H, Parving HH, et al. Effect of a multifactorial intervention
Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation
on mortality in type 2 diabetes. N Engl J Med 2008;358:580e91.
Suh SW, Hamby AM, Swanson RA. Hypoglycemia, brain energetics, and
McGavock JM, Lingvay I, Zib I, et al. Cardiac steatosis in diabetes mellitus:
hypoglycemic neuronal death. Glia 2007;55:1280e6.
a 1H-magnetic resonance spectroscopy study. Circulation 2007;116:1170e5.
Maddock HL, Siedlecka SM, Yellon DM. Myocardial protection from either
Solang L, Malmberg K, Ryden L. Diabetes mellitus and congestive heart failure.
ischaemic preconditioning or nicorandil is not blocked by gliclazide. Cardiovasc Drugs
Further knowledge needed. Eur Heart J 1999;20:789e95.
Kiencke S, Handschin R, von Dahlen R, et al. Pre-clinical diabetic cardiomyopathy:
UKPDS 34; UK Prospective Diabetes Study Group. Effect of intensive blood-glucose
prevalence, screening, and outcome. Eur J Heart Fail 2010.
control with metformin on complications in overweight patients with type 2 diabetes.
Bartnik M, Ryden L, Ferrari R, et al. The prevalence of abnormal glucose regulation
in patients with coronary artery disease across Europe. The Euro Heart Survey on
Gerstein HC, Miller ME, Byington RP, et al. The action to control cardiovascular risk
diabetes and the heart. Eur Heart J 2004;25:1880e90.
in diabetes study group. Effects of intensive glucose lowering in type 2 diabetes.
Ryden L, Standl E, Bartnik M, et al. Guidelines on diabetes, pre-diabetes, and
N Engl J Med 2008;358:2545e59.
cardiovascular diseases: executive summary. The Task Force on Diabetes and
Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic,
Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the
severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological
European Association for the Study of Diabetes (EASD). Eur Heart J
analysis of the ACCORD study. Bmj 2010;340:b4909.
Riddle MC, Ambrosius WT, Brillon DJ, et al. Epidemiologic relationships between
Anselmino M, Malmberg K, Ryden L, et al. A gluco-metabolic risk index with
A1C and all-cause mortality during a median 3.4-year follow-up of glycemic
cardiovascular risk stratification potential in patients with coronary artery disease.
treatment in the ACCORD trial. Diabetes Care 2010;33:983e90.
Diab Vasc Dis Res 2009;6:62e70.
Montori VM, Fernandez-Balsells M. Glycemic control in type 2 diabetes: time for an
Anselmino M, Ohrvik J, Malmberg K, et al. Glucose lowering treatment in patients
evidence-based about-face? Ann Intern Med 2009;150:803e8.
with coronary artery disease is prognostically important not only in established but
UKPDS 33; UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose
also in newly detected diabetes mellitus: a report from the Euro Heart Survey on
control with sulphonylureas or insulin compared with conventional treatment and risk
Diabetes and the Heart. Eur Heart J 2008;29:177e84.
of complications in patients with type 2 diabetes. Lancet 1998;352:837e53.
Young LH, Wackers FJ, Chyun DA, et al. Cardiac outcomes after screening for
Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular
asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD
complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129e39.
study: a randomized controlled trial. Jama 2009;301:1547e55.
Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and
De Caterina R, Madonna R, Sourij H, et al. Glycaemic control in acute coronary
vascular outcomes in patients with type 2 diabetes. N Engl J Med
syndromes: prognostic value and therapeutic options. Eur Heart J
Turnbull FM, Abraira C, Anderson RJ, et al. Intensive glucose control and
Opie LH. Metabolic management of acute myocardial infarction comes to the fore
macrovascular outcomes in type 2 diabetes. Diabetologia 2009;52:2288e98.
and extends beyond control of hyperglycemia. Circulation 2008;117:2172e7.
Kelly TN, Bazzano LA, Fonseca VA, et al. Systematic review: glucose control and
Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2
cardiovascular disease in type 2 diabetes. Ann Intern Med 2009;151:394e403.
diabetes and coronary artery disease. N Engl J Med 2009;360:2503e15.
Currie CJ, Peters JR, Tynan A, et al. Survival as a function of HbA(1c) in people with
Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI
type 2 diabetes: a retrospective cohort study. Lancet 2010;375:481e9.
for stable coronary disease. N Engl J Med 2007;356:1503e16.
Ashrafian H, Frenneaux MP, Opie LH. Metabolic mechanisms in heart failure.
Hage C, Norhammar A, Grip L, et al. Glycaemic control and restenosis after
percutaneous coronary interventions in patients with diabetes mellitus: a report from
MacDonald MR, Eurich DT, Majumdar SR, et al. Treatment of type 2 diabetes and
the Insulin Diabetes Angioplasty study. Diab Vasc Dis Res 2009;6:71e9.
outcomes in patients with heart failure: a nested case-control study from the U.K.
Kim LJ, King SB 3rd, Kent K, et al. Factors related to the selection of surgical versus
General Practice Research Database. Diabetes Care 2010;33:1213e18.
percutaneous revascularization in diabetic patients with multivessel coronary artery
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
disease in the BARI 2D (Bypass Angioplasty Revascularization Investigation in Type 2
Hausenloy DJ, Yellon DM. GLP-1 therapy: beyond glucose control. Circ Heart Fail
Diabetes) trial. JACC Cardiovasc Interv 2009;2:384e92.
Banning AP, Westaby S, Morice MC, et al. Diabetic and nondiabetic patients with
Nilsson PM. ACCORD and risk-factor control in type 2 diabetes. N Engl J Med
left main and/or 3-vessel coronary artery disease: comparison of outcomes with
cardiac surgery and paclitaxel-eluting stents. J Am Coll Cardiol 2010;55:1067e75.
Yudkin JS, Richter B, Gale EA. Intensified glucose lowering in type 2 diabetes: time
Farilla L, Bulotta A, Hirshberg B, et al. Glucagon-like peptide 1 inhibits cell apoptosis
for a reappraisal. Diabetologia 2010.
and improves glucose responsiveness of freshly isolated human islets. Endocrinology
Skyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control and the
prevention of cardiovascular events: implications of the ACCORD, ADVANCE,
Pratley RE, Nauck M, Bailey T, et al. Liraglutide versus sitagliptin for patients
and VA Diabetes Trials: a position statement of the American Diabetes
with type 2 diabetes who did not have adequate glycaemic control with
Association and a Scientific Statement of the American College of Cardiology
metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet
Foundation and the American Heart Association. J Am Coll Cardiol
Heart 2011;97:6e14. doi:10.1136/hrt.2010.214031
Controversies in the cardiovascular
management of type 2 diabetes
Lionel H Opie, Derek M Yellon and Bernard J Gersh
2011 97: 6-14 originally published online November 23, 2010
Updated information and services can be found at:
These include:
This article cites 90 articles, 38 of which can be accessed free at:
Article cited in:
Receive free email alerts when new articles cite this article. Sign up in
the box at the top right corner of the online article.
To request permissions go to:
To order reprints go to:
To subscribe to BMJ go to:
Source: https://m.askmedical.com.sg/content/dam/medical-services/malaysia/129-medicalinformationportal-com/bmj-news/Diabetes/heartjnl214031.pdf
Int. J. Mol. Sci. 2011, 12, 3648-3704; doi:10.3390/ijms12063648 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 Micro Electromechanical Systems (MEMS) Based Microfluidic Devices for Biomedical Applications Muhammad Waseem Ashraf *, Shahzadi Tayyaba and Nitin Afzulpurkar
Volume 88 Number 862 June 2006 The right to the truthin international law:fact or fiction? Yasmin Naqvi*Yasmin Naqvi is a Ph.D. candidate in International Law at the Graduate Institute of International Studies, Geneva. She holds a DES in International Law (Graduate Institute of International Studies) and a BA/LLB with honours (University of Tasmania) AbstractThe right to the truth has emerged as a legal concept at the national, regional andinternational levels, and relates to the obligation of the state to provide information tovictims or to their families or even society as a whole about the circumstancessurrounding serious violations of human rights. This article unpacks the notion of theright to the truth and tests the normative strength of the concept against the practice ofstates and international bodies. It also considers some of the practical implications ofturning ‘‘truth'' into a legal right, particularly from the criminal law perspective.