Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Microsoft word - 33 models of causation - health determinants



Health Determinants
Core Body of Knowledge for the Generalist OHS Professional
OHS Body of Knowledge
Models of Causation – Health Determinants
Copyright notice and licence terms
First published in 2012 by the Safety Institute of Australia Ltd, Tullamarine, Victoria, Australia.
ISBN 978-0-9808743-1-0
This work is copyright and has been published by the Safety Institute of Australia Ltd (SIA) under the
auspices of HaSPA (Health and Safety Professionals Alliance). Except as may be expressly provided by law
and subject to the conditions prescribed in the Copyright Act 1968 (Commonwealth of Australia), or as
expressly permitted below, no part of the work may in any form or by any means (electronic, mechanical,
microcopying, digital scanning, photocopying, recording or otherwise) be reproduced, stored in a retrieval
system or transmitted without prior written permission of the SIA.
You are free to reproduce the material for reasonable personal, or in-house, non-commercial use for the
purposes of workplace health and safety as long as you attribute the work using the citation guidelines below
and do not charge fees directly or indirectly for use of the material. You must not change any part of the work
or remove any part of this copyright notice, licence terms and disclaimer below.
A further licence will be required and may be granted by the SIA for use of the materials if you wish to:
· reproduce multiple copies of the work or any part of it · charge others directly or indirectly for access to the materials · include all or part of the materials in advertising of a product or services, or in a product for sale · modify the materials in any form, or · publish the materials.
Enquiries regarding the licence or further use of the works are welcome and should be addressed to:
Registrar, Australian OHS Education Accreditation Board
Safety Institute of Australia Ltd, PO Box 2078, Gladstone Park, Victoria, Australia, 3043
Citation of the whole Body of Knowledge should be as:
HaSPA (Health and Safety Professionals Alliance).(2012). The Core Body of Knowledge for Generalist OHS Professionals. Tullamarine, VIC. Safety Institute of Australia.
Citation of individual chapters should be as, for example:
Pryor, P., Capra, M. (2012). Foundation Science. In HaSPA (Health and Safety Professionals
Alliance), The Core Body of Knowledge for Generalist OHS Professionals. Tullamarine, VIC.
Safety Institute of Australia.
Disclaimer
This material is supplied on the terms and understanding that HaSPA, the Safety Institute of
Australia Ltd and their respective employees, officers and agents, the editor, or chapter authors and
peer reviewers shall not be responsible or liable for any loss, damage, personal injury or death
suffered by any person, howsoever caused and whether or not due to negligence, arising from the
use of or reliance of any information, data or advice provided or referred to in this publication.
Before relying on the material, users should carefully make their own assessment as to its accuracy,
currency, completeness and relevance for their purposes, and should obtain any appropriate
professional advice relevant to their particular circumstances.
OHS Body of Knowledge
Models of Causation – Health Determinants

OHS Body of Knowledge
Models of Causation – Health Determinants
OHS Body of Knowledge
Models of Causation – Health Determinants
Synopsis of the OHS Body Of Knowledge
Background
A defined body of knowledge is required as a basis for professional certification and for
accreditation of education programs giving entry to a profession. The lack of such a body
of knowledge for OHS professionals was identified in reviews of OHS legislation and
OHS education in Australia. After a 2009 scoping study, WorkSafe Victoria provided
funding to support a national project to develop and implement a core body of knowledge
for generalist OHS professionals in Australia.
Development
The process of developing and structuring the main content of this document was managed
by a Technical Panel with representation from Victorian universities that teach OHS and
from the Safety Institute of Australia, which is the main professional body for generalist
OHS professionals in Australia. The Panel developed an initial conceptual framework
which was then amended in accord with feedback received from OHS tertiary-level
educators throughout Australia and the wider OHS profession. Specialist authors were
invited to contribute chapters, which were then subjected to peer review and editing. It is
anticipated that the resultant OHS Body of Knowledge will in future be regularly amended
and updated as people use it and as the evidence base expands.
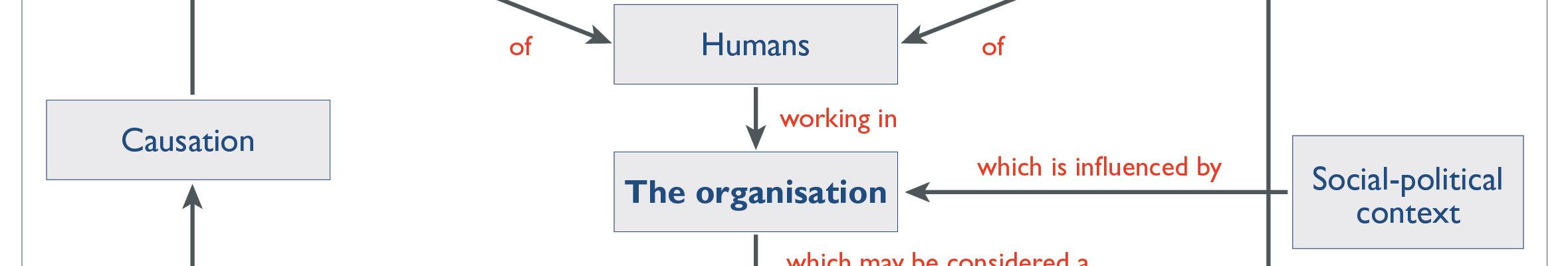
Conceptual structure
The OHS Body of Knowledge takes a ‘conceptual' approach. As concepts are abstract, the
OHS professional needs to organise the concepts into a framework in order to solve a
problem. The overall framework used to structure the OHS Body of Knowledge is that:
Work impacts on the safety and health of humans who work in organisations. Organisations are
influenced by the socio-political context. Organisations may be considered a system which may
contain hazards which must be under control to minimise risk. This can be achieved by
understanding models causation for safety and for health which will result in improvement in the
safety and health of people at work. The OHS professional applies professional practice to
influence the organisation to being about this improvement.
OHS Body of Knowledge
Models of Causation – Health Determinants
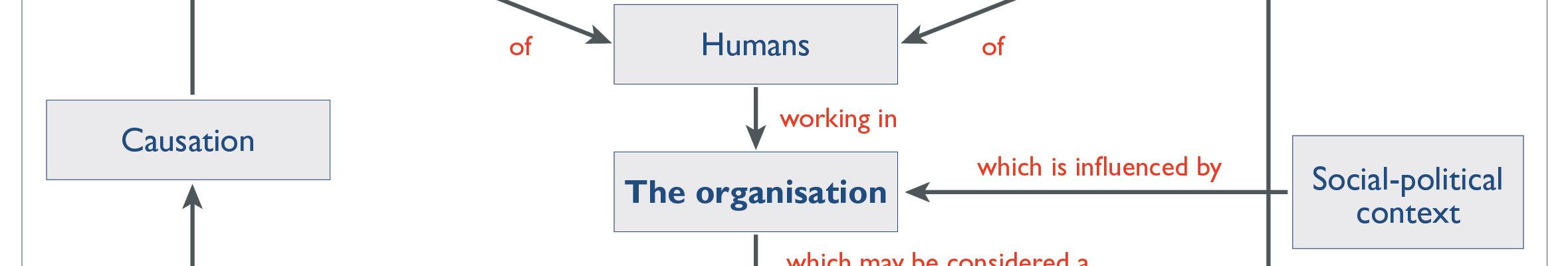
This can be represented as:
Audience
The OHS Body of Knowledge provides a basis for accreditation of OHS professional
education programs and certification of individual OHS professionals. It provides guidance
for OHS educators in course development, and for OHS professionals and professional
bodies in developing continuing professional development activities. Also, OHS
regulators, employers and recruiters may find it useful for benchmarking OHS professional
Application
Importantly, the OHS Body of Knowledge is neither a textbook nor a curriculum; rather it
describes the key concepts, core theories and related evidence that should be shared by
Australian generalist OHS professionals. This knowledge will be gained through a
combination of education and experience.
Accessing and using the OHS Body of Knowledge for generalist OHS professionals
The OHS Body of Knowledge is published electronically. Each chapter can be downloaded
separately. However users are advised to read the Introduction, which provides background
to the information in individual chapters. They should also note the copyright requirements
and the disclaimer before using or acting on the information.
OHS Body of Knowledge
Models of Causation – Health Determinants
Models of Causation: Health Determinants
Wendy Macdonald BSc(Hons)Psych, G.DipPsych, PhD, MHFESA, MICOH, FSIA, FIEA
Associate Professor, Centre for Ergonomics and Human Factors,
Faculty of Health Sciences, La Trobe University
Email: [email protected]
Wendy is a highly experienced OHS educator, researcher and consultant, and a road safety researcher. Her OHS research interests include: workplace management strategies to reduce the risk of musculoskeletal injuries and disorders; impacts of workload on occupational stress and wellbeing; issues related to workforce ageing; and OHS in industrially developing countries. She plays a leading role within the World Health Organisation (WHO) global network of Collaborating Centres in Occupational Health, of which her own Centre is a member. On behalf of the International Ergonomics Association (IEA) she is responsible for liaison between the IEA and the WHO network.
Peer reviewer
Professor Niki Ellis MBBS, AFOEM, AFPHM
Chief Executive Officer
Institute of Safety, Compensation and Recovery Research, Monash University
Core Body of
Knowledge for the
Generalist OHS
OHS Body of Knowledge
Models of Causation – Health Determinants
Core Body of Knowledge for the Generalist OHS Professional
Models of Causation: Health Determinants
Abstract
Health is a state with both negative and positive dimensions; it extends beyond the absence
of diseases and disorders to encompass personal wellbeing more generally. Its
determinants are diverse and not confined to workplace hazard exposures, so identifying
and managing the main work-related influences on health can be difficult. Models of
occupational health causation range from macro-level conceptions, which include
determinants external to the workplace but are insufficiently detailed to guide workplace
risk management, through to evidence-based models depicting the work-related causes of a
particular disease or disorder. An understanding of the latter type of causal model is
particularly important to enable effective risk management of diseases and health disorders
that have multiple and potentially interacting hazards (e.g. musculoskeletal disorders,
mental disorders, cardiovascular diseases).
Keywords
health, illness, disease, causation, work
OHS Body of Knowledge
Models of Causation – Health Determinants
Contents
Historical overview .1
Understanding the determinants of occupational health outcomes .2
‘Causation' and work-relatedness.2
Macro-level models of occupational health determinants .4
Hazard-specific diseases and disorders .6
Diseases and disorders with multiple determinants .7
Workplace benefits and determinants of positive wellbeing . 14
Implications for OHS practice . 19
Management of risk for diseases/disorders with multiple, diverse causes . 19
Management of risk from psychosocial hazards . 20
Workplace health promotion . 20
Professional roles . 21
Key authors and thinkers . 21
Acknowledgement . 22
OHS Body of Knowledge
Models of Causation – Health Determinants
OHS Body of Knowledge
Models of Causation – Health Determinants
The safety aspects of Occupational Health and Safety (OHS), concerned with prevention of
accident-related injuries, are often seen as central to the role of the generalist OHS
professional. However, contemporary OHS professional practice requires at least an equal
focus on workers' health. This chapter – one of two about models of causation1 – describes
the kinds of health-related causal models required for effective OHS risk management.
Section 2 outlines the historical contributions of various professional groups to our
understanding of occupational health determinants. Section 3 discusses the basis for
identifying observed health outcomes as ‘work-related', considers various models of
causation, and outlines the importance of positive dimensions of occupational health and their
determinants. Finally, section 4 summarises implications for OHS professional practice.
Historical overview
The history of occupational health practice dates back several thousand years (see Abrams,
2001; Gochfeld, 2005). This section briefly considers the contributions of various
professional groups to our current understanding of occupational health determinants.
Medical practitioners played a key role during the earliest years, leading during the 20th
century to development of the profession of occupational medicine (Lane & Lee, 1991).
Occupational diseases were initially attributed only to physical hazards, particularly
chemical, physical and biological exposures; the fields of industrial toxicology and
occupational hygiene emerged from this approach. Occupational epidemiology and related
sociological research also developed during the 20th century from origins traceable to the
early 18th century work of Ramazzini (2001 translation), who documented the hazards and
related health problems for more than 50 occupations in De Morbis Artificum Diatriba
(Diseases of Workers).2 More recently, epidemiologists and public health professionals have
elucidated the social determinants of health, both within and external to workplaces; for
example, the now famous WhiteHall Studies were instigated by Marmot during the 1960s and
are ongoing (see Marmot, Siegrist & Theorell, 2006).
Development of sociotechnical systems theory during the 1940s and 50s by psychologists at
the Tavistock Institute in London provided one of the first examples of a systems approach to
optimise both work performance and employee wellbeing (Trist, 1981). Concurrently, the
related field of ergonomics brought a human-centred approach to the workplace, focusing
variously on system safety and performance, and on occupational health issues (Wilson,
2000). The field of occupational health psychology emerged during the 1980s from a
1 See OHS BoK Models of Causation: Safety. 2 For detail on the historical context for occupational health see OHS BoK The Human: As a Biological System. OHS Body of Knowledge
Models of Causation - Health Determinants
confluence of industrial/organisational psychology and health psychology, with recent inputs
also from psychoneurobiology as it relates to the physiological processes underpinning
psychological wellbeing (for example see Pressman and Cohen, 2005). Professionals in this
field have highlighted the widespread impacts on occupational health of work-related
stressors, and have specialist expertise in managing workplace risks stemming from
psychosocial hazards, particularly as they relate to mental disorders and wellbeing.3
In summary, it can be seen that the field of occupational health now spans highly diverse
areas of expertise. Some implications for OHS professional practice are discussed in section
Understanding the determinants of occupational health outcomes
This section first discusses the nature of ‘causation' within an OHS context and the basis for
concluding that observed health outcomes are work-related. It then discusses the nature and
role of macro-level models of occupational health determinants. The third part identifies the
kinds of diseases/disorders which typically have just one main work-related cause, and the
fourth discusses causal models for diseases/disorders with multiple, possibly interacting
determinants. The final part of this section considers positive dimensions of health and their
determinants, since the importance of these is being increasingly recognised, consistent with
the World Health Organization definition of health as "a state of complete physical, mental
and social well-being and not merely the absence of disease or infirmity" (WHO, 1948).
‘Causation' and work-relatedness
The development and implementation of effective OHS intervention strategies requires an
understanding of the factors ‘causing' occupational health outcomes. In this context, causes
include work-related hazards and other risk factors that increase the probability and/or
severity of harm to health, as well as factors that promote positive states of health and
wellbeing.
Determining the causes of injuries is usually a more straightforward process than diagnosing
the causes of health outcomes. The most obvious reason for this difference is that with
injuries there is usually no separation in time between the injury and the harmful event that is
its immediate cause. For example, in the case of a person's contact with the cutting edge of a
machine blade, the harmful event provides a clear starting point for investigations to
determine causation and the work-relatedness of the injury is not disputed. In contrast, health
3 See OHS BoK Psychosocial Hazards and Occupational Stress OHS Body of Knowledge
Models of Causation - Health Determinants
outcomes often result from exposures to hazards4 over extended periods of time, and there
may be latency periods of many decades between the hazard exposure(s) and the
manifestation of health effects. This longer timeframe makes it less likely that the harm to
health will be identified as work-related, and increases the difficulty of identifying relevant
hazards and other risk factors in any individual case.
Work-related injuries can often be attributed to several work-related causal factors, but the
high salience of the injurious event can result in risk management focusing too narrowly on
that event. For example, efforts to control risk of injury from a machine blade often focus on
installation of a well-designed guard, but it might also be important to control factors such as
production pressures that motivate workers to save time by disabling the machine guard,
inadequate supervision, and poor safety culture more generally.5
Work-related health outcomes are different from injury outcomes in that many diseases by
their nature are indicative of their cause, whereas this is not true of injuries. The nature of
injuries suffered in an accident does not usually indicate the cause of the accident; for
example, the causes of road accidents cannot usually be deduced from the nature of injuries
suffered. In contrast, diseases such as mesiothelioma, or disorders such as noise-induced
hearing loss, by their nature indicate the main work-related cause of that health outcome –
exposure to asbestos in the first case and to excessive noise in the second. Causal
mechanisms differ widely between different health outcomes, and because of this diversity, a
variety of quite different causal models are required to support occupational health
Another important difference between causation of injuries and of health outcomes is that the
latter are usually more affected by non-work factors, and the work-relatedness of many health
problems therefore tends to be poorly documented and inadequately acknowledged.
Nevertheless, some diseases have been widely accepted as work-related (i.e. as ‘occupational' diseases) due to their hazard-specific nature and the low probability of non-work exposures to that particular hazard. Examples include diseases arising from exposure to
dust, poisonings from exposures to some hazardous substances, and infections transmitted
from farm animals to farmers, veterinarians or abattoir workers. Although noise-induced
hearing loss is widely accepted as an occupational disorder, the increasing incidence of non-
work exposures due to personal music devices may render this increasingly open to dispute.
In the case of cancers, work-relatedness is often disputed, particularly those that are both very
common and very severe in their effects so there is a lot at stake. Attempts have been made to
determine the overall proportion of cancers that are work-related, but:
4 Exposure may be defined in terms of both its nature and its extent. For the present purpose, nature of exposure refers to the type of hazard to which people are exposed; this encompasses the various types of hazard listed in the OHS BoK. Extent of exposure refers to the severity and duration of the exposure. 5 For conceptual models supporting analysis of the causation of harmful events see OHS BoK Models of Causation: Safety. OHS Body of Knowledge
Models of Causation - Health Determinants
Reliably establishing the causes of any one cancer type is very difficult because cancer proceeds from a combination of events, these events occur over a period of years or decades, and causal factors seldom fingerprint the cancer histology (Benke & Goddard, 2006, p. 485).
For any such health outcomes, a causal relationship, rather than just a statistical association,
is more likely when:
· Exposure precedes the health outcome (essential for causality, but not always easy to
establish, e.g. because cancer might start years before it manifests clinically)
· The observed association is strong · More intense or prolonged exposures are associated with more frequent or severe
outcomes (i.e. there is a dose-response relationship)
· The association between exposure and outcome is compatible with existing
knowledge of biological mechanisms
· A particular kind of exposure tends to be associated with a particular health outcome · Evidence is similar across different groups at different times (Hill, 1965; NRC&IM,
For further discussion of causation in an OHS context, see Hill (1965), or a report by the
National Research Council and Institute of Medicine, USA (2001, pp. 65–82).
Macro-level models of occupational health determinants
Macro-level models of occupational health determinants provide comprehensive coverage of
factors including, but not confined to, work-related hazards. A good example of such a model
is the World Health Organization's Healthy Workplace Model (Burton, 2010) (Figure 1).
This depicts the OHS risk-management action cycle (an eight-step continual improvement
process – Mobilize, Assemble, Assess, Prioritize, Plan, Do, Evaluate, Improve) in the context
of four overlapping sets of occupational health determinants: the psychosocial work
environment, the physical work environment, personal health resources, and linkages
between the enterprise and its wider community. Of central importance are the enterprise's
core ethics and values, supported and promoted by leadership engagement and worker
OHS Body of Knowledge
Models of Causation - Health Determinants

Figure 1: WHO Healthy Workplace Model: Avenues of Influence, Process and Core
Principles (Based on Burton, 2010, p. 3)
Sorensen et al. (as cited in Ellis)6 conceived an even ‘bigger picture' macro model that
includes four sets of external influences on occupational health that are not depicted in the
WHO model: legal, economic, political and social factors. However, the WHO model
includes more detail at the individual enterprise level.
In common with most macro models of occupational health determinants, Figure 1 includes
an element – ‘personal health resources' – representing relevant characteristics of workers. In
the Sorensen et al. model used by Ellis this is termed ‘individual health-related behaviors'; in
the systems models used by ergonomists such an element typically refers to the capacities and
limitations that affect people's ability to cope with work demands (e.g. see ‘coping resources' 6 OHS BoK Global Concept: Health (section 3) OHS Body of Knowledge
Models of Causation - Health Determinants
in Figure 4). Thus, although these models differ in the particular individual variables
identified, there is consensus that some individual-level factors should be included in the
overall conceptual framework. Examples of individual variables that may be important in the
occupational health context include:
· Personal vulnerabilities and causal factors stemming from:
o Permanent or stable factors: age, gender, physical size and strength
(anthropometrics), personality characteristics (e.g. positive/negative effect,
locus of control), health-related genetic vulnerabilities and predispositions,
chronic health problems, etc.
o Factors amenable to change within a medium timeframe: work-related
knowledge and skills, health-related behaviours (e.g. nutrition, exercise,
smoking), some health problems and injuries, job satisfaction and morale,
physical fitness, etc.
o More transitory states: fatigue, stress, mood, etc.
· Lifestyle factors (e.g. having to cope with demands from personal commitments to
family and friends; availability of personal support from non-work sources) might
also be relevant in some contexts.
Personal and lifestyle factors such as the above are often seen as exerting a major influence
on health. For example, even when someone suffers a ‘heart attack' at work, the causes are
more likely to be seen as personal and lifestyle rather than work-related factors (despite the
evidence on work-related causes of cardiovascular disease discussed in section 3.3 below). In
contrast, when someone suffers injury due to an accident at work, it is usual to look for work-
related causes, even when personal factors are also identified as contributors.
Macro-level models illustrate the wide range of both work and non-work factors that
influence occupational health. They span public health as well as occupational health
domains, providing the basis for a broad range of health protection and promotion strategies
both within and beyond the workplace. However, more narrowly focused causal models are
required to guide the detailed development of risk-management strategies at the workplace
Hazard-specific diseases and disorders
Some occupational diseases and disorders are associated with one primary work-related
hazard as opposed to a diverse range of hazards of varying importance.7 Examples of hazard-
specific health conditions are shown in Table 1, with the hazard of primary importance
shown in the right-hand column. Effects of exposures to the primary work-related hazard
7 Because of their strong association with a particular hazard, further information about the causation of such diseases or disorders is located in the relevant OHS BoK Hazard chapters. OHS Body of Knowledge
Models of Causation - Health Determinants
(plus exposures external to the workplace) interact with individual susceptibilities to increase
risk of the particular disease or disorder.
Table 1: Causal factors for a sample of diseases/disorders where there is one main
work-related hazard
Example of
Individual susceptibility
Work-related hazards –
Inherent
Acquired
causal agent(s)
· Some substance
· Excessive noise levels
hearing loss
exposures (prescribed, occupational)
· Asbestos dust
unknown, but a genetic influence is likely
· Contact with infected
· Coxiel a burneti (bacterium)
Allergic contact · Inherited or early · Continuing exposure to · e.g. nickel, chromium, epoxy dermatitis
sensitising agent
resins, latex particles,
· Co-existing irritant
· Inherited or early · Prior exposure to
· e.g. volatile isocyanates,
sensitising agent
protein dusts, Western Red
· Hyper-reactivity of the
Cedar, aluminium smelting
individual's airways
Diseases and disorders with multiple determinants
Ellis noted that "The traditional OHS model is straining as the burden of health in workplaces
shifts to illness arising from chronic disease."8 This situation is primarily due to
diseases/disorders that typically have multiple causes. These include cardiovascular diseases,
musculoskeletal disorders and mental disorders, which are three of the eight
diseases/disorders identified as warranting particular focus within Australia's National OHS Strategy 2002–2012 (Safe Work Australia, 2010a).
In 2010, the Australian Institute of Health and Welfare reported:
More than 6.1 million Australians aged 16–85 years suffer from a musculoskeletal condition at a point in time (38% of that population) and 3.2 million (20%) experience a mental disorder in a 12–month period (AIHW, 2010, p. 1).
Such evidence illustrates that both musculoskeletal and mental disorders have major impacts
on population health, beyond their more easily quantifiable costs in terms of compensation
claims. Australian workers' compensation statistics for the period 2007–08 showed that
8 OHS BoK Global Concept: Health (Abstract) OHS Body of Knowledge
Models of Causation - Health Determinants
musculoskeletal injuries and disorders were responsible for the largest proportion of serious
claims,9 followed by mental disorders.
The most common injury leading to serious claims was Sprains & strains of joints & adjacent muscles, which accounted for 43% of all serious claims. The most common diseases resulting in serious claims were Disorders of muscle, tendons & other soft tissues (6% of all serious claims), Dorsopathies – disorders of spinal vertebrae (6% of all serious claims) and Mental disorders (5% of all serious claims). (Safe Work Australia, 2010b, p. vii)
These compensation statistics create the impression that sudden-onset musculoskeletal injuries (sprains and strains) are much more common than cumulative disorders, in which case consideration of their determinants would be outside the scope of this chapter focussed
on health determinants. However, many musculoskeletal problems cannot be clearly
diagnosed as either an ‘injury' or a ‘disease/disorder' (ASCC, 2006), since it is now evident
that thresholds for acute injury are reduced by cumulative exposures, both within a work shift
and over longer time periods (e.g. Visser & van Dieen, 2006; van Dieen, 2007). The
dichotomy between acute and cumulative injury is even more questionable when information
about causation is derived from compensation claims data. Several factors combine to make it
likely that compensation claims focus largely on events immediately preceding the report,
resulting in substantial bias towards reporting an injury rather than a disease (see Macdonald
& Evans, 2006, pp. 12–15). In any case, body stressing is the reported mechanism for all
such claims categorised as diseases and most of those categorised as injuries; overall, body
stressing is the reported mechanism in 41% of all serious claims (including both injuries and
disorders). Consequently, causal models for cumulative onset musculoskeletal disorders
encompass most of the important work-related hazards for musculoskeletal injuries also
(ASCC, 2006). Risk factors specific to sprain/strain injuries where the mechanism is
falls/slips/trips are considered elsewhere.10
As noted above, mental disorders constitute the second largest category of serious claims,
following musculoskeletal disorders (Safe Work Australia, 2010c). Importantly, there is a
statistical association between these two categories of disorder:
Published studies suggest that causal pathways are more likely to be from musculoskeletal conditions to mental disorders than the reverse, although the latter can also occur…The clear association between musculoskeletal conditions and mental disorders found in this study emphasises the need for health-care providers to be aware of and provide for a multidisciplinary approach to the management of this comorbidity. (AIHW, 2010, p. 2)
Since psychosocial hazards are the primary work-related cause of mental disorders, the nature
and causation of mental disorders is the chapter on that type of hazard, by Way11.
9 "Serious claims are those lodged in the reference year and accepted by the date at which the data are extracted and involve either a death, a permanent incapacity, or a temporary incapacity requiring an absence from work of one working week or more" (Safe Work Australia, 2010b, p. 1). 10 See OHS BoK Gravitational Hazards 11 See OHS BoK Psychosocial Hazards and Occupational Stress OHS Body of Knowledge
Models of Causation - Health Determinants
The third category of disease/disorder considered here is cardiovascular. Cardiovascular
diseases are not responsible for a large proportion of compensation claims in Australia
(where they are termed ‘diseases of the circulatory system') – probably because they have
multiple causal factors unrelated to work and it is difficult to determine the contribution of
work-related hazards in individual cases since they are often asymptomatic until well
advanced. However, there is substantial research evidence that a wide range of work-related
factors – both physical and psychosocial – can contribute to risk of these diseases (Driscoll,
2006; Kim & Kang, 2010; LaMontagna et al., 2006; Landsbergis et al., 2001). According to a
2006 review for the Australian Safety and Compensation Council:
The evidence is strongest with exposure to four particular chemicals, namely carbon disulphide and, in terms of acute exposure, carbon monoxide, methylene chloride and nitroglycerin. There is also good evidence for the role of environmental tobacco smoke and psychosocial factors, particularly low job control, and considerable evidence for noise and shiftwork. Other exposures, for which the evidence is less strong, include chronic low-level exposure to carbon monoxide, methylene chloride and nitroglycerin, other chemicals, long working hours, electromagnetic fields, temperature extremes, diesel exhaust and other particulates, organic combustion products, manual work or strenuous occupations, sedentary work, and certain specific occupations. (Driscoll, 2006, pp. vi–vii)
Other reviews have placed greater emphasis on the causal role of work-related psychosocial
hazards (e.g. see LaMontagna et al., 2006, 2007). The importance of such factors was
emphasised in a report from Korea's Occupational Safety and Health Research Institute (Kim
& Kang, 2010), which found that the "triggering factors" in cases of cerebrovascular diseases
(n = 211) were job stress (20.9%), overload (32.7%), shift and night work (3.3%),
professional driving (2.4%), environmental change (1.4%), others (7.1%) and unknown
(32.2%). In cases of coronary heart disease (n = 117), the triggering factors were job stress
(22.2%), overload (44.4%), shift and night work (3.5%), professional driving (0.9%),
environmental change (0.9%), others (8.5%) and unknown (19.7%).
Where a large array of factors coalesces to produce an outcome, as for the above types of
diseases/disorders, the processes involved can be depicted in a model of causation.12 For
diseases and disorders where risk typically arises from a multiplicity of hazards, there are
models depicting the aetiology of each particular disease/disorder in terms of how exposures
to various hazards combine with other risk factors in determining risk level. To illustrate this,
the following section considers models of causation for musculoskeletal disorders.
12 See also OHS BoK Models of Causation: Safety OHS Body of Knowledge
Models of Causation - Health Determinants
3.4.1 An example: Models of causation for musculoskeletal disorders13
For health or safety outcomes arising primarily from just one type of hazard, risk can be
estimated in terms of the severity of the hazard and the extent of exposure to it. However, for
multi-hazard conditions such as musculoskeletal disorders (MSDs), risk depends on the
particular combination of hazards present. It has been shown that interactions between a
number of hazards and related factors can substantially affect MSD risk (Bernard, 1997;
Marras, 2008; NRC&IM, 2001), which means that the extent of a particular exposure, if
considered independently of other exposures, is not necessarily a good indicator of MSD risk.
Importantly, this means that MSD risk cannot be adequately assessed by separately
evaluating each potential hazard or risk factor, as is typical for hazard-focused risk
assessment. This point is discussed further below, with reference to hazards depicted in
Figures 2 to 4 show evidence-based models of MSD causation, illustrating the diverse array
of hazards that can affect MSD risk.
13 "Musculoskeletal disorders include a wide range of inflammatory and degenerative conditions affecting the muscles, tendons, ligaments, joints, peripheral nerves, and supporting blood vessels.[They include] over 100 diseases and syndromes, which are usually progressive and are associated with pain.such as ‘repetitive strain injuries', ‘occupational overuse syndrome', ‘back injury', ‘osteoarthritis', ‘backache', ‘sciatica', ‘slipped disc', ‘carpal tunnel syndrome' and others. [They] exert a substantial economic burden in health care and compensation costs, lost salaries and productivity borne not only by the employers and employees, but also by the community. As the conditions become more serious and impinge on the person's functional capacity, their work performance and productivity are also likely to decrease." (ASCC, 2006, pp. 9–10) OHS Body of Knowledge
Models of Causation - Health Determinants
Figure 2: Model of hazards and other risk factors for work-related musculoskeletal
disorders (based on NRC&IM, 2001, p. 3)
The model in Figure 2 resulted from a review of research evidence by a multidisciplinary
committee of experts on behalf of the USA National Research Council and Institute of
Medicine (2001). On the left side of the model within The Workplace there are three groups
of hazards and risk factors: ‘external loads' (biomechanical hazards),14 ‘organisational
factors', and ‘social context'; those in the latter two groups are commonly known as
psychosocial hazards.15 Hazards within all three categories interact (shown by linking arrows)
and can affect processes internal to The Person (internal biomechanical loading,16
physiological responses) and personal outcomes (discomfort, pain, impairment, disability).
Also, fatigue is recognised as a relevant factor.17 As shown on the right of the diagram,
individual factors influence all personal processes and outcomes.
Although stress is not highlighted in Figure 2, it is implicit there within ‘physiological
14 See OHS BoK Biomechanical Hazards 15 See OHS BoK Psychosocial Hazards and Occupational Stress 16 Different from the external biomechanical loading discussed in OHS BoK Biomechanical Hazards 17 See OHS BoK Psychosocial Hazards: Fatigue OHS Body of Knowledge
Models of Causation - Health Determinants
responses'. The well-documented role of stress in MSD causation is much more apparent in
Figure 3, which highlights the interacting effects of physical (mainly biomechanical) and
psychosocial hazards on MSD risk. A person's internal ‘stress response,' as shown here,
occurs when situations are experienced as stressful; it is multidimensional, with physiological
and behavioural, as well as cognitive and affective dimensions (Cox, 1978). The cognitive
and behavioural aspects of this response can directly affect safety, while the physiological
and affective aspects can have profound effects on health including, but not confined to,
MSD risk18 (e.g. Aptel & Cnockaert, 2002; Chandola et al., 2008; Macdonald & Evans, 2006;
Figure 3: A model highlighting evidence that internal processes producing cumulative
tissue damage include the multidimensional ‘stress response' as well as internal
biomechanical loads and pain sensitisation (Macdonald & Evans, 2006, p. 10)
18 See OHS BoK The Human: Basic Principles of Psychology OHS Body of Knowledge
Models of Causation - Health Determinants
Figure 4: A composite ergonomics model of work-related hazards for musculoskeletal
disorders (based on Macdonald & Evans, 2006, p. 24)
The primary purpose of the models in Figures 2 and 3 is to promote better understanding of
MSD aetiology, based on current research evidence. The model in Figure 4 is in accord with
these, but is more directly applicable to workplace risk management because it provides more
detail concerning the wide range of work-related hazards that can combine to affect risk. This
model shows that MSD risk is increased if ‘job and task demands' are hazardous or excessive
in relation to available ‘coping resources,' and that risk is also affected by ‘other
psychosocial hazards.' Job and task demands include the widely recognised hazards of
OHS Body of Knowledge
Models of Causation - Health Determinants
manual task performance, along with two other subsets – those arising from the cognitive and
emotional demands of task performance, and those arising from demands of the overall job. Coping resources are determined by workplace factors (support systems and resources; psychosocial and physical environment influences) and by the individual's own capabilities.
Importantly, it is the combination of these diverse variables that determines risk, which is
why MSD risk cannot be adequately assessed by a process that considers each hazard
separately. For example, a particular posture might be rated as low risk if considered alone,
but for workers who are chronically fatigued and/or stressed due to long working hours, tight
production schedules with few rest breaks, and supervisors perceived as unsupportive, the
risk might be considerably higher.
Figure 4 shows various pathways leading from ‘Hazardous workplace and personal
conditions' to the occurrence of musculoskeletal injuries and disorders. In the case of sudden
onset sprains and strains (which are classified as injuries rather than diseases/disorders), there
is a direct link from excessive force and/or adverse posture to injury. However, our focus
here is on the aetiology of cumulative disorders, and for these, the pathway to injury is via
ongoing ‘hazardous personal states' where risk is increased by the kind of internal
physiological and biomechanical processes indicated in Figure 2 and detailed in Figure 3.
The above models (Figures 2–4) clearly show that managing ‘manual handling' hazards is not synonymous with managing MSD risk. In light of this, it is unfortunate that MSDs are often referred to in Australia as ‘manual handling injuries', since that terminology supports
the erroneous assumption that biomechanical hazards are the only important cause of
musculoskeletal problems. Clearly, a much wider range of hazards and risk factors including
some related to work organisation, job design and the workplace environment (psychosocial
as well as physical) must be managed. In particular, it is important to include management of
fatigue and stress, since internal physiological and biomechanical dimensions of these are
linked to MSD risk.
As outlined above, MSD risk management requires a holistic multidimensional approach that
is founded on evidence-based models of causation and takes account of the particular combination of hazards present in a given situation. Further, there is evidence that:
…a combination of several kinds of interventions (multidisciplinary approach) including organisational, technical and personal/individual measures is better than single measures.[and that] a participative approach which includes the workers in the process of change has a positive effect on the success of an intervention (EASHW, 2008, pp. 7–8).
Workplace benefits and determinants of positive wellbeing
The focus of conventional OHS practice has been to prevent harm to workers as reflected in
the disease/disorder causal models reviewed in section 3.4. However, there is increasing
recognition of the importance of achieving good health and wellbeing rather than just
OHS Body of Knowledge
Models of Causation - Health Determinants
avoiding disease. This section considers the workplace benefits of good health and wellbeing,
including their potential role in decreasing occupational disease risk. It finishes with an
outline of key workplace determinants.
Various notions of wellbeing (e.g. happiness and wellness, and more work-specific concepts
such as morale and job satisfaction) have been developed by researchers and applied in
workplace settings. Concepts vary according to whether they concern fairly stable individual
personality dimensions or ‘traits,' or more transient ‘states.' In an OHS context, personal
states are of primary interest as these are most affected by workplace and job conditions.
Such concepts also vary according to their emphasis on affective versus cognitive
dimensions. For example, ‘job satisfaction' is cognitively oriented because it implies some
personal evaluation of the job, although it is also influenced by people's enjoyment of their
job so it has an affective dimension also. ‘Morale' signifies a positive affective state oriented
towards engagement with and commitment to job performance; it is linked to concepts such
as ‘vitality' and ‘vigour' (Ryan & Frederick, 1997). Hart and Cooper (2001) identified three
dimensions of occupational wellbeing: morale (positive affect), psychological distress
(negative affect), and job satisfaction (conceived as predominantly cognitive). Warr
(2007a,b) also distinguished three dimensions within wellbeing, which he now refers to as ‘happiness'.
A principal axis runs from feeling bad to feeling good, and two others (distinguished in terms of degree of activation as well as pleasure) extend from negative feelings of anxiety to experiences of happiness as tranquil contentment, and from states of depression to happiness as energised pleasure (Warr, 2007b, p. 726).
Good health and wellbeing clearly have intrinsic value, particularly to the individuals
concerned. From an employer perspective, high vitality and morale also are beneficial
because of their links to good work performance. Importantly in this OHS context, high
levels of job satisfaction have been linked to lower duration of sickness absence (Marmot et
al., 1995). Wegge, Schmidt, Parkes and van Dick (2007) concluded that the frequency of
people ‘taking a sickie' and the time lost due to these absences are affected by an interaction
between job satisfaction and job involvement,19 such that high job satisfaction greatly
decreases the negative impact on sickness absence of low job involvement. In other words,
low levels of psychological wellbeing are manifest in various ‘illness behaviours',20 including
more frequent and longer sickness absence. Such absences could therefore serve as one
19 ‘Job involvement' refers to the extent to which an individual identifies with the job. 20 According to Mechanic (1986, p. 1): "Illness behaviour.involves the manner in which individuals monitor their bodies, define and interpret their symptoms, take remedial action, and utilize sources of help.It also is concerned with how people monitor and respond to symptoms and symptom change over the course of an illness and how this affects behaviour, remedial actions taken, and response to treatment. The different perceptions, evaluations and responses to illness have, at times, a dramatic impact on the extent to which symptoms interfere with usual life routines, chronicity, attainment of appropriate care and cooperation of the patient in treatment. Variables affecting illness behaviour usually come into play well before any medical scrutiny and treatment."
OHS Body of Knowledge
Models of Causation - Health Determinants
indicator of the success or otherwise of OHS risk management.
Looking beyond absenteeism to sickness itself, it is well established that negative states such
as stress are linked to poor health.21 Is there also evidence that positive states are beneficial to
health? Based on a large meta-analysis of research reporting associations between job
satisfaction and various measures of health, Faragher, Cass and Cooper (2005) found that
high job satisfaction was strongly associated with good mental health (correlations with
burnout, self-esteem, depression, and anxiety ranged from 0.478 to 0.420). Correlations
between job satisfaction and physical health were smaller, but still highly significant
statistically. The authors concluded that:
The wellbeing of employees—and in particular their mental health—may be compromised if their work is causing them to experience high levels of dissatisfaction. Thus, the extent to which individuals feel satisfied with their work becomes an important (mental) health issue. (Faragher, Cass & Cooper, 2005, p. 111)
Pressman and Cohen (2005) analysed evidence concerning the role of positive affect in the
aetiology of physical diseases and disorders. Their review included research on the
functioning of the cardiovascular, endocrine and immune systems – systems that appear to
mediate the effects of positive affect on health as reported above. They concluded that
positive affect can reduce disease risk via multiple pathways, shown in Figure 5.
21 See OHS BoK Psychosocial Hazards and Occupational Stress
OHS Body of Knowledge
Models of Causation - Health Determinants
ANS = autonomic nervous system HPA = hypothalamic–pituitary–adrenal axis
Figure 5: A ‘stress buffering' model of behavioural and biological mechanisms by which
positive emotions can reduce disease risk (Pressman & Cohen, 2005, p. 959)
Figure 6 presents a simple model of health, its determinants and its OHS impacts. Various
types of work and non-work environmental factors are depicted as influencing health, along
with individual factors, which reflects the more detailed causal models presented above.
Health itself is enclosed within the blue rectangle; it can be seen that this encompasses both
positive and negative personal states, consistent with the widely accepted WHO definition of
health (WHO, 1948). However, these personal states are also among the determinants of
diseases and disorders, which are also part of ‘health'; that is, some aspects of ‘health' (these
personal states) are shown to be determinants of some other aspects of health
(diseases/disorders).
OHS Body of Knowledge
Models of Causation - Health Determinants
Figure 6: A model of health, its various work-related and other determinants, and OHS
impacts.
Figure 6 also identifies some determinants of sickness absence. Such absences may be due to
particular diseases and disorders, some of which are work-related, and/or they may be a
manifestation of illness behaviours linked to states such as low morale and high stress, as
discussed above.22 Distinguishing absence from work due to a specific disease/disorder from
absence representing illness behaviour is particularly difficult in the case of both
musculoskeletal and mental disorders (Australia's two largest ‘occupational disease'
compensation claims categories). In both these types of disorder, the influence of personal
states as depicted in Figure 6 can be centrally important; consequently, an understanding of
how best to manage these personal states is important for OHS professionals.
What then are the main work-related determinants of these personal states, which can
influence health both positively and negatively? Causes of stress and fatigue are considered
elsewhere.23 What about the determinants of positive states such as morale and job
22 Ellis has highlighted the potential importance of illness behaviours, pointing out: "An underlying disease can be detected in only about half of presentations to general practitioners" (OHS BoK Global Concept: Health, section 2.3). 23 OHS BoK Psychosocial Hazards and Occupational Stress; OHS BoK Psychosocial Hazards: Fatigue. OHS Body of Knowledge
Models of Causation - Health Determinants
satisfaction? Warr (2007b) concluded that the main workplace determinants of wellbeing, or
· Opportunity for personal control – discretion, decision latitude, participation, etc. · Opportunity for skill use and acquisition – a setting's potential for applying and
developing expertise and knowledge
· Externally generated goals – ranging across job demands, underload and overload,
task identity, role conflict, required emotional labour and work-home conflict
· Variety – in job content and location · Environmental clarity – including role clarity, task feedback and low future ambiguity · Contact with others –both quantity and quality · Availability of money – the opportunity to receive income at a certain level · Physical security – including working conditions, degree of hazard, etc. · Valued social position – in terms of the significance of a task or role · Supportive supervision – the extent to which one's concerns are taken into
· Career outlook – encompassing job security and the opportunity to gain promotion or
shift to other roles
· Equity – both within the organisation and in that organisation's relations with society
(Warr, 2007b, p. 727).
Comparison of the above factors with those identified as psychosocial hazards or stressors24
shows a high degree of overlap, but the importance of each factor as a determinant of
wellbeing is likely to vary depending on the particular context and the state or aspect of
wellbeing that is of interest.
Implications for OHS practice
Management of risk for diseases/disorders with multiple, diverse causes
The conventional approach to OHS risk management has been to focus on hazard
management – identifying hazards, assessing risk from each identified hazard, and taking any
necessary steps to control risk from each hazard separately. For health-related risks, this
approach works well for hazard-specific diseases and disorders of the kind discussed in
However, a more holistic approach to risk management is required to achieve effective
control of risk for diseases and disorders for which risk is determined by multiple, diverse
hazards, such as musculoskeletal disorders and mental disorders. To manage such health risks
effectively, the management process needs to be guided by an appropriate model of
24 See OHS BoK Psychosocial Hazards and Occupational Stress. OHS Body of Knowledge
Models of Causation - Health Determinants
causation. Such models identify the multiple causal pathways between the relevant set of
hazards and the particular type of health outcome, so that risk management can be based on
assessment of risk from the combined effects of the hazards identified as most relevant in the
particular situation, taking account of the hazards' additive and possibly interacting effects.
Worker participation in this holistic approach to risk management is likely to be beneficial, if
Management of risk from psychosocial hazards
Occupational health is of course influenced by the presence or absence of diseases and
disorders. Health is also directly influenced by psychological states such as stress, ‘vitality'
and morale (shown in Figure 6), which in turn are influenced by a wide range of work-related
psychosocial hazards. It is therefore essential that OHS risk management deals effectively
with risk from this kind of hazard. The importance of this is particularly clear in countries
such as Australia, where the most expensive compensation claims are for diseases/disorders
where risk is strongly influenced by psychosocial hazards. A participative, holistic approach
is required to manage risk from psychosocial hazards and to promote positive aspects of
health and wellbeing.25
Workplace health promotion
Ellis (2001) proposed a model of OHS risk management that encompasses health promotion
as well as harm prevention. Based on current knowledge of the occupational health benefits
of positive psychological states and the increasing importance of a sustainably healthy
workforce in the context of population ageing, there are strong argument for incorporating
health promotion strategies within OHS risk management programs. This viewpoint is
evident in the WHO Healthy Workplace Model (Figure 1).
The concept of health promotion originated in the public health domain, and workplace
health promotion strategies are sometimes simply public health promotion strategies
implemented within a workplace setting (e.g. WHO, 2011). However, boundaries between
occupational and public health are becoming increasingly blurred due to changes in the way
we work,26 and there is:
.a growing appreciation that there are multiple determinants of workers' health.[and] workforce health promotion initiatives have moved toward a more comprehensive approach, which acknowledges the combined influence of personal, environmental, organizational, community and societal factors on employee well-being (WHO, 2011).
25 OHS BoK Psychosocial Hazards and Occupational Stress. 26 See OHS BoK Global Concept: Work OHS Body of Knowledge
Models of Causation - Health Determinants
Professional roles
The body of scientific evidence concerning the nature and determinants of occupational
health spans a wide variety of disciplines, as outlined in section 2. This diversity is reflected
in the fragmented nature of current OHS professional practice, where specialist groups
include occupational hygienists, occupational ergonomists, occupational physicians,
occupational health nurses, occupational health psychologists, occupational rehabilitation
professionals, and so on. Consequently, the task of defining a core body of occupational
health knowledge and associated professional competencies for generalist OHS professionals
presents a considerable challenge.
In light of the major differences in causation between different types of diseases/disorders, no
OHS professional can be expected to have a high level of expertise in managing all types of
risk to occupational health. Indeed, it seems likely that most generalist OHS professionals
will have some degree of specialist expertise also, probably reflecting existing areas of
specialist OHS professional practice. In this situation there are likely to be ongoing ethical
dilemmas and debate concerning what constitutes an adequate level of competence or
expertise for a particular work role.
Arguably the most important element of professional competency might be a good
understanding of the limitations of one's own knowledge and competencies. This will only be
achievable if generalist OHS professionals are familiar with a comprehensive range of causal
models of occupational health determinants relevant to their field of practice. On this basis
they will be able to analyse and understand a particular problem or situation sufficiently to
recognise if/when they need to enlist specialist support, consistent with the model of
professional practice.27
This chapter has described models of occupational health determinants and their roles in
supporting effective OHS risk management. An understanding of such models was shown to
be particularly important for the effective management of diseases/disorders where risk is
affected by multiple hazards, some of which can interact. Such health conditions include
musculoskeletal disorders, mental disorders, and cardiovascular disease. The importance of
positive wellbeing for occupational health was also described.
Key authors and thinkers
Tom Cox, Austin Bradford Hill, Michael Marmot, William Marras, Bernadino Ramazzini,
27 See OHS BoK Model of OHS Practice OHS Body of Knowledge
Models of Causation - Health Determinants
Thanks to Dr David Goddard, Department of Epidemiology and Preventive Medicine,
Monash University, for his invaluable contributions to this chapter.
References
Abrams, H. K. (2001). A short history of occupational health. Journal of Public Health
Policy, 22(1), 34–80.
AIHW (Australian Institute of Health and Welfare). (2010). When musculoskeletal
conditions and mental disorders occur together. AIHW Bulletin, 80 (Cat. no. AUS 129). Canberra, ACT: AIHW. Retrieved May 2011 from http://www.aihw.gov.au/publication-detail/?id=6442468392
Aptel, M., & Cnockaert, J. C. (2002). Stress and work-related musculoskeletal disorders of
the upper extremities. Trade Union Technical Bureau (TUTB) Newsletter, 19–20, 50–56. Retrieved May 2011 from http://hesa.etui-rehs.org/uk/newsletter/files/Newsletter-20.pdf
ASCC (Australian Safety and Compensation Council). (2006). Work-related Musculoskeletal
Disease in Australia. Canberra, ACT: Commonwealth of Australia. Retrieved May 2011 from http://www.safeworkaustralia.gov.au/AboutSafeWorkAustralia/WhatWeDo/Publications/Documents/119/WorkRelatedMusculoskeltalDisorders_2006Australia_2006_ArchivePDF.pdf
Benke, G., & Goddard, D. (2006). Estimation of occupational cancer in Australia still needs
local exposure data. Australian & New Zealand Journal of Public Health, 30(5), 485–486.
Bernard, B. P. (Ed.). (1997). Musculoskeletal disorders (MSDs) and workplace factors.
Cincinnati, OH: National Institute for Occupational Safety and Health.
Burton, J. (2010). WHO Healthy Workplace Framework and Model: Background and
Supporting Literature and Practice. Geneva: WHO. Retrieved May 2011 from http://www.who.int/occupational_health/healthy_workplace_framework.pdf
Chandola, T., Britton, A., Brunner, E., Hemingway, H., Malik, M., Kumari, M., Badrick, E.,
Kivimaki, M., & Marmot, M. (2008). Work stress and coronary heart disease: What are the mechanisms? European Heart Journal, 29(5), 640–648.
Cox, T. (1978). Stress. London: Macmillan.
Driscoll, T. (2006). Work-related Cardio-vascular Disease in Australia Canberra, ACT:
Australian Safety and Compensation Council. Retrieved May 2011 from http://www.safeworkaustralia.gov.au/AboutSafeWorkAustralia/WhatWeDo/Publications/Documents/116/WorkRelatedCardiovascularDisease_2006Australia_2006_ArchivePDF.pdf
EASHW (European Agency for Safety and Health at Work). (2008). Work-related
OHS Body of Knowledge
Models of Causation - Health Determinants
Musculoskeletal Disorders: Prevention Report. Luxembourg: Office for Official Publications of the European Communities, EASHW. Retrieved May 2011 from http://osha.europa.eu/en/publications/reports/en_TE8107132ENC.pdf
Ellis, N. (2001). Work and health: Management in Australia and New Zealand. Melbourne,
VIC: Oxford University Press.
Faragher, E. B., Cass, M., & Cooper, C. L. (2005). The relationship between job satisfaction
and health: A meta-analysis. Occupational & Environmental Medicine, 62(2), 105–112.
Gochfeld, M. (2005). Chronologic history of occupational medicine. Journal of Occupational
& Environmental Medicine, 47(2), 96–114.
Hart, P. M., & Cooper, C. L. (2001). Occupational stress: Toward a more integrated
framework. In N. Anderson, D. S. Ones, H. K. Sinangil & C. Viswesvaran (Eds.), Handbook of industrial, work and organizational psychology, Volume 2, organizational psychology (2nd ed.) (pp. 93–114). London, UK: Sage.
Hill, A. B. (1965). The environment and disease: Association or causation? Proceedings of
the Royal Society of Medicine, 58, 295–300.
Kim, D-S., & Kang, S-K. (2010). Work-related cerebro-cardiovascular diseases in Korea.
Journal of Korean Medical Science, 25(Suppl.), S105–S111.
LaMontagne, A. D., Keegel, T., Louie, A. M., Ostry, A., & Landsbergis, P. A. (2007). A
systematic review of the job-stress intervention evaluation literature, 1990–2005. International Journal of Occupational & Environmental Health, 13(3), 268–280.
LaMontagne, A. D., Louie, A., Keegel, T., Ostry, A., & Shaw, A. (2006). Workplace Stress
in Victoria: Developing a Systems Approach (Report to the Victorian Health Promotion Foundation). Carlton South, VIC: Victorian Health Promotion Foundation. Retrieved May 2011 from http://www.vichealth.vic.gov.au/workplacestress
Landsbergis, P. A., Schnall, P. L., Belkic, K. L., Baker, D., Schwartz, J., & Pickering, T. G.
(2001). Work stressors and cardiovascular disease. Work, 17(3), 191–208.
Lane, R. E., & Lee, W. R. (1991). The development of training in occupational medicine in
the United Kingdom. Environmental & Occupational Health, 19(2), 247–255.
Macdonald, W., & Evans, O. (2006). Research on the Prevention of Work-related
Musculoskeletal Disorders. Stage 1 – Literature Review. Canberra, ACT: Australian Safety & Compensation Council,. Retrieved May 2011 from http://www.safeworkaustralia.gov.au/ABOUTSAFEWORKAUSTRALIA/WHATWEDO/PUBLICATIONS/Pages/RR200606ResearchOnPreventionOfWRMusculoskeletalDisorders.aspx
Marmot, M., Feeney, A., Shipley, M., North, F., & Syme, S. L. (1995). Sickness absence as a
measure of health status and functioning: From the UK Whitehall II study. Journal of Epidemiology & Community Health, 49(2), 124–130.
Marmot, M., Siegrist J., & Theorell, T. (2006). Health and the psychosocial environment at
OHS Body of Knowledge
Models of Causation - Health Determinants
work. In M. Marmot & R. G. Wilkinson (Eds.), Social determinants of health (2nd ed.). Oxford: Oxford University Press.
Marras, W. S. (2008). The working back: A systems view. Hoboken, NJ: John Wiley & Sons.
Mechanic, D. (1986). The concept of illness behaviour: Culture, situation, and personal
predisposition. Psychological Medicine, 16(1), 1–7.
NRC&IM (National Research Council and Institute of Medicine). (2001). Musculoskeletal
disorders and the workplace: Low back and upper extremities (Methodological issues and approaches, pp. 65–81). Washington, DC: National Academy Press. Retrieved May 2011 from http://www.nap.edu/openbook.php?record_id=10032&page=R2
Pressman, S. D., & Cohen, S. (2005). Does positive affect influence health? Psychological
Bulletin, 131(6), 925–971.
Ramazzini, B. (2001). De morbis artificum diatriba [Diseases of workers]. American Journal
of Public Health, 91(9), 1380–1382.
Ryan, R. M., & Frederick, C. M. (1997). On energy, personality, and health: Subjective
vitality as a dynamic reflection of well-being. Journal of Personality, 65(3), 529–565.
Safe Work Australia. (2010a). National OHS Strategy 2001–2012. Canberra, ACT:
Commonwealth of Australia. Retrieved May 2011 from http://www.safeworkaustralia.gov.au/AboutSafeWorkAustralia/WhatWeDo/Publications/Documents/230/NationalOHSStrategy_2002-2012.pdf
Safe Work Australia. (2010b). Compendium of Workers' Compensation Statistics Australia
2007–08. Barton, ACT: Safe Work Australia.
Safe Work Australia. (2010c). Occupational Disease Indicators 2010. Barton, ACT:
Commonwealth of Australia. Retrieved May 2011 from http://www.safeworkaustralia.gov.au/ABOUTSAFEWORKAUSTRALIA/WHATWEDO/PUBLICATIONS/Pages/RP201005OccupationalDiseaseIndicators2010.aspx
Trist, E. (1981). Occasional Paper 2: The evolution of socio-technical systems: A conceptual
framework and an action research project Ontario Ontario Ministry of Labour
van Dieen, J. H. (2007). Injury models in observational and experimental research. (Keynote
presentation) In Proceedings of the Sixth International Scientific Conference on Prevention of Work-Related Musculoskeletal Disorders: PREMUS 2007. Boston, USA.
Visser, B., & van Dieen, J. H. (2006). Pathophysiology of upper extremity muscle disorders.
Journal of Electromyography & Kinesiology, 16(1), 1–16.
Warr, P. (2007a). Work, happiness, and unhappiness. Mahwah, NJ: Erlbaum.
Warr, P. (2007b). Searching for happiness at work. Psychologist, 20(12), 726–729.
Warren, N. (2001). Work stress and musculoskeletal disorder etiology: The relative roles of
psychosocial and physical risk factors. Work, 17(3), 221–234.
OHS Body of Knowledge
Models of Causation - Health Determinants
Wegge, J., Schmidt, K-H., Parkes, C., & van Dick, R. (2007). ‘Taking a sickie': Job
satisfaction and job involvement as interactive predictors of absenteeism in a public organization. Journal of Occupational & Organizational Psychology, 80(1), 77–89.
Wilson, J.R. (2000). Fundamentals of ergonomics in theory and practice. Applied
Ergonomics, 31, 557-567.
WHO (World Health Organization). (1948). Constitution of the World Health Organization.
Retrieved March 10, 2011, from http://www.who.int/governance/eb/constitution/en/index.html
WHO (World Health Organization). (2011). Workplace health promotion. Retrieved May
2011 from http://www.who.int/occupational_health/topics/workplace/en/
OHS Body of Knowledge
Models of Causation - Health Determinants
Source: http://www.ohsbok.org.au/wp-content/uploads/2013/12/33-Models-of-causation-Health-determinants.pdf
Hindawi Publishing CorporationBioMed Research InternationalVolume 2014, Article ID 121396, 7 pages Clinical StudyAlga Ecklonia bicyclis, Tribulus terrestris, and GlucosamineOligosaccharide Improve Erectile Function, Sexual Quality ofLife, and Ejaculation Function in Patients with ModerateMild-Moderate Erectile Dysfunction: A Prospective,Randomized, Placebo-Controlled, Single-Blinded Study
NATIONAL LIFE SCIENCES P2 VERSION 1 (NEW CONTENT) FOR FULL-TIME CANDIDATES NOVEMBER 2011 MARKS: 150 This memorandum consists of 11 pages. Copyright reserved Please turn over Life Sciences/P2 (Version 1) (Full-time) DBE/November 2011 NSC – Memorandum PRINCIPLES RELATED TO MARKING LIFE SCIENCES 2011