Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Doi:10.1016/s0140-6736(12)60030-0
Cervical pessary in pregnant women with a short cervix
(PECEP): an open-label randomised controlled trial
Maria Goya, Laia Pratcorona, Carme Merced, Carlota Rodó, Leonor Valle, Azahar Romero, Miquel Juan, Alberto Rodríguez, Begoña Muñoz, Belén Santacruz, Juan Carlos Bello-Muñoz, Elisa Llurba, Teresa Higueras, Luis Cabero*, Elena Carreras*, on behalf of the Pesario Cervical para Evitar Prematuridad (PECEP) Trial Group
Summary
Background Most previous studies of the use of cervical pessaries were either retrospective or case controlled and their Published
Online
results showed that this intervention might be a preventive strategy for women at risk of preterm birth; no randomised DOI:10.1016/S0140-
controlled trials have been undertaken. We therefore undertook a randomised, controlled trial to investigate whether the 6736(12)60030-0
insertion of a cervical pessary in women with a short cervix identifi ed by use of routine transvaginal scanning at See
Online/Comment
20–23 weeks of gestation reduces the rate of early preterm delivery.
Methods The Pesario Cervical para Evitar Prematuridad (PECEP) trial was undertaken in fi ve hospitals in Spain. *Contributed equally
Pregnant women (aged 18–43 years) with a cervical length of 25 mm or less were randomly assigned according to a Maternal Fetal Medicine Unit,
Department of Obstetrics,
computer-generated allocation sequence by use of central telephone in a 1:1 ratio to the cervical pessary or expectant
Hospital Universitari Vall
management (without a cervical pessary) group. Because of the nature of the intervention, this study was not masked. d'Hebron, Universitat
The primary outcome was spontaneous delivery before 34 weeks of gestation. Analysis was by intention to treat. This Autonoma de Barcelona,
study is registered with ClinicalTrials.gov, number NCT00706264.
Barcelona, Spain (M Goya MD,
L Pratcorona MD, C Merced MD,
C Rodó MD, J C Bello-Muñoz MD,
Findings 385 pregnant women with a short cervix were assigned to the pessary (n=192) and expectant management E Llurba PhD, T Higueras MD,
groups (n=193), and 190 were analysed in each group. Spontaneous delivery before 34 weeks of gestation was signifi cantly E Carreras PhD, L Cabero PhD)
;
less frequent in the pessary group than in the expectant management group (12 [6%] vs 51 [27%], odds ratio 0·18, Maternal and Child Health and
Development Network (SAMID),
95% CI 0·08–0·37; p<0·0001). No serious adverse eff ects associated with the use of a cervical pessary were reported.
Instituto Salud Carlos III, Madrid,
Spain (M Goya, E Llurba,
Interpretation Cervical pessary use could prevent preterm birth in a population of appropriately selected at-risk E Carreras, L Cabero)
; Centre for
women previously screened for cervical length assessment at the midtrimester scan.
Biomedical Research on Rare
Diseases (CIBERER), Instituto
Salud Carlos III, Madrid, Spain
Funding Instituto Carlos III.
(E Llurba)
; Maternal Fetal
Medicine Unit, Department of
the reported studies were either retrospective or case
Obstetrics, Hospital
Universitario Materno Infantil
Spontaneous preterm birth, which arises in roughly controlled and the results showed that a cervical pessary
de Canarias, Las Palmas de Gran
5–13% of pregnancies, is the leading cause of perinatal can be used as a preventive strategy for patients at risk of
Canaria, Canary Islands, Spain
morbidity and mortality.1–4 However, the rates have not preterm birth.10 No randomised controlled trials have (L Valle PhD, A Romero MD)
;
changed much over the past 10 years. Improvements in been undertaken. We therefore assessed the eff ect of
Maternal Fetal Medicine Unit,
Department of Obstetrics,
neonatal care have increased survival rates in very cervical pessary on the spontaneous early preterm birth
Hospital Son Llatzer, Balearic
premature infants. Never theless, a major reduction in rate in asymptomatic women.
Islands, Spain (M Juan MD)
;
rates of mortality and morbidity in premature babies
Maternal Fetal Medicine Unit,
Department of Obstetrics,
will only be achieved with increased precision in the
Methods
Institut Universitari Dexeus,
identifi cation of women at risk of spontaneous preterm
Participants and trial design
Barcelona, Spain
birth and through the develop
ment of an eff ective A prospective, open-label, randomised clinical trial (A Rodríguez MD)
; Maternal Fetal
prevention for this complication.
was undertaken in fi ve hospitals in Spain. Pregnant
Medicine Unit, Department of
Obstetrics, Hospital Sant Joan de
A strategy for the prevention of spontaneous preterm women (aged 18–43 years) with singleton pregnancies who
Reus, Reus, Tarragona, Spain
births in which therapeutic intervention is restricted to were undergoing routine second trimester ultra sonography (B Muñoz MD)
; and Maternal
women with a previous preterm birth is likely to have a at 18–22 weeks of gestation were given the option of
Fetal Medicine Unit,
small eff ect on the overall rate of prematurity since only
transvaginal ultrasonographic measurement of cervical
Department of Obstetrics,
Hospital de Fuenlabrada,
about 10% of spontaneous preterm births arise in length as a predictor of spontaneous preterm birth.11
Madrid, Spain (B Santacruz MD)
women with such a history.5 Ultrasonographic measure-
Cervical length was measured according to the criteria of
Correspondence to:
ment of cervical length at 20–23 weeks of gestation can the Fetal Medicine Foundation.12 Women with a cervical Dr Elena Carreras, Maternal Fetal
increase the identifi cation of women at risk of either length of 25 mm or less were invited to take part in the Medicine Unit, Department of
singleton or twin pregnancies.6–8 Asymptomatic women Pesario Cervical para Evitar Prematuridad (PECEP) trial. Obstetrics, Hospital Universitari
Vall d'Hebron, Universitat
with a short cervical length (≤25 mm) are at increased Exclusion criteria were major fetal abnormalities, painful
Autonoma de Barcelona,
risk of spontaneous early preterm delivery.
regular uterine contractions, active vaginal bleeding, Passeig de la Vall d'Hebron,
Cervical pessary is a silicone device that has been used ruptured membranes, placenta praevia, and a history of 119-129, 08036 Barcelona, Spain
in the past 50 years to prevent preterm birth.9 Most of cone biopsy or cervical cerclage in situ.
www.thelancet.com
Published online April 3, 2012 DOI:10.1016/S0140-6736(12)60030-0

Gestational age was judged from the menstrual history
the scans had received extensive training and passed a
and confi rmed by measurement of fetal crown-rump practical examination administered by an expert to length at a fi rst trimester scan, which was done routinely
demonstrate their competence in cervical assessment. All
in all participating hospitals.
the images of the cases included in the trial were reviewed
Trial coordinators regularly undertook quality control of
centrally. All cases of preterm birth were reviewed and
screening, data handling, and verifi cation of adher ence to
discussed centrally. Dr Arabin, Witten, Germany, very
protocols at the diff erent centres. Obstetricians who did kindly provided, free of charge, advice, recommendations,
and suggestions for the use of cervical pessaries in pregnant women. The central team then instructed the
other centres about the use of the pessary (fi gure 1).
The ethics committees for all participating hospitals
approved the protocol.
Randomisation and masking
After written informed consent was obtained from women,
they were randomly allocated to the cervical pessary group
Figure 1: Photograph of the silicone cervical pessary
or expectant management group in a 1:1 ratio. The
(A) Inner diameter. (B) Outer diameter. (C) Lateral view.
randomisation sequence was computer generated by the Statistics Unit of the Vall d'Hebron Hospital Research Institute, Barcelona, Spain, with variable block sizes of two and four, stratifi ed for centre and parity, and implemented by use of central telephone. The recruiters or the trial coordinator did not have access to the randomisation sequence. The allocation code was disclosed after the
patient's initials were confi rmed. This study was open label because of the nature of the intervention.
Interventions
Cervical and vaginal swabs were taken from all patients
for bacteriological analysis. If visual evidence existed of infection, appropriate treatment was given and insertion of the pessary was delayed by 1 week. Vaginal examination
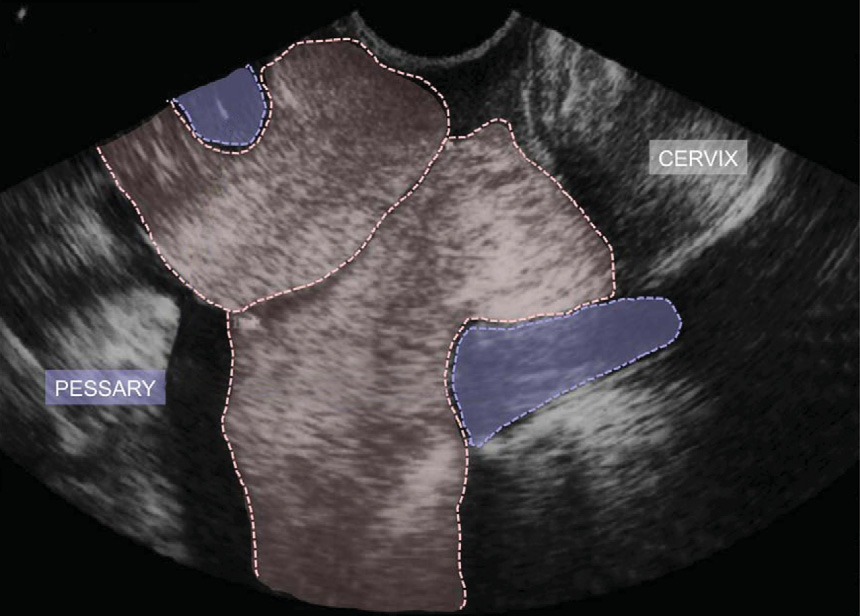
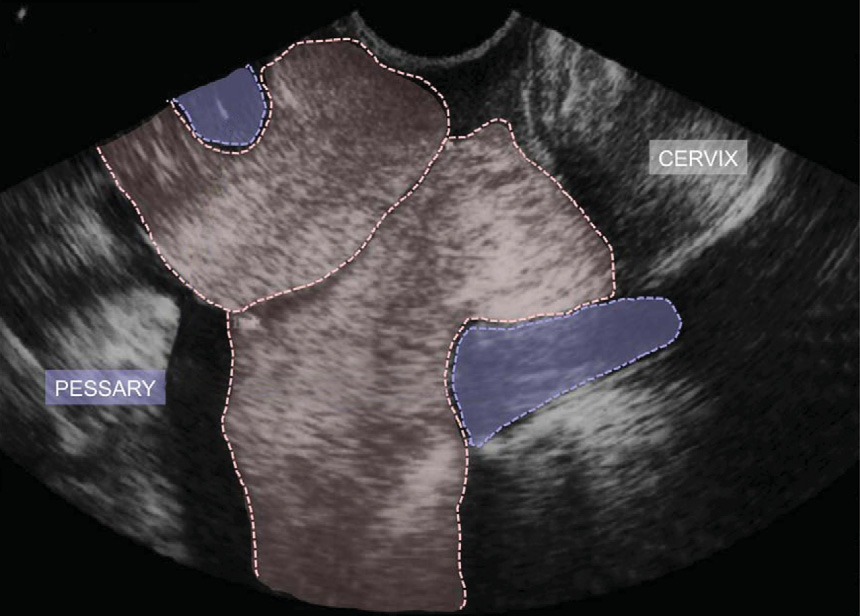
Figure 2: Cervical pessary
was done to detect cervical dilation or visible membranes.
The smaller diameter of the pessary is fi tted around the cervix and the larger
The pessary was not removed if there was evidence of
diameter faces the pelvic fl oor, thus rotating the cervix to the posterior vaginal wall and correcting the cervical angle.
bacterial infection after device insertion; however, appro-priate antibiotic treatment was given. Patients allocated to the pessary group had the device inserted and were given detailed instructions about its subsequent manage-ment. Special emphasis was placed on the need to report any adverse symptoms immediately.
We used cervical pessaries certifi
Conformity (CE0482, MED/CERT ISO 9003/EN 46003; Dr Arabin, lower larger diameter 70 mm, height 30 mm, and upper smaller diameter 32 mm) during the study.
Both groups were seen by the clinical team of the trial
at each centre every month until delivery. Transabdominal ultrasonography was done for fetal biometries and wellbeing, clinical questionnaire was administered for
confi rmation of correct device placement in the pessary group (fi gure 2), vaginal swab was taken for study of bacteriological infection, and transvaginal ultra
graphy was done to measure cervical length (fi gure 3).
The pessary was removed during the 37th week of
gestation. Indications for pessary removal before this time were active vaginal bleeding, risk of preterm labour with persistent contractions despite tocolysis, or severe
Figure 3: Ultrasound visualisation of cervical length in women using a cervical pessary13
patient discomfort.
www.thelancet.com Published online April 3, 2012 DOI:10.1016/S0140-6736(12)60030-0
Patients whose pessaries were removed (even on the
same day of insertion) remained in the trial because of
18 235 eligible women
the intention-to-treat principle.
6360 declined to participate
Statistical analysis
The primary outcome was spontaneous preterm birth
before 34 weeks (238 days) of gestation. Secondary out-comes are shown in the appendix. Chorioamnionitis was
See Online for appendix
defi ned as infl ammation of the chorion and amnion by
11 149 did not meetinclusion criteria
histopathological assessment after delivery.
10 568 cervix >25 mm
Calculation of sample size was based on a reduction in
351 fetal abnormalities126 contractions
the incidence of spontaneous delivery before 34 weeks
from 28% in the expectant management group to 14% in the pessary group, with a power of 80%. To detect this
726 cervix ≤25 mm
diff erence at a signifi cance level of 5%, we needed to recruit 380 patients with cervical length of 25 mm or less. If the prevalence of cervical length of 25 mm or less is
341 declined to participate
8%, a total of 4750 women would need to be scanned to identify 380 cases of short cervix.
385 randomly assigned
Statistical analysis was based on the intention-to-treat
principle. The mean and SD summarised baseline data for the pessary and expectant management groups.
Comparisons between groups were made with the
Mann-Whitney U test. Univariate comparisons of dichotomous data were done with Fisher's exact test. The p values for all hypotheses were two sided, and
2 lost to follow-up
3 lost to follow-up
p values of less than 0·05 were judged to be signifi cant. The risk of spontaneous preterm birth before 34 weeks
was quantifi ed by use of the odds ratio and 95% CI.
Multivariate analysis was done by use of logistic
regression.14 The risk of spontaneous preterm birth Figure 4: Trial profi le
from randomisation until 34 weeks was assessed with
Kaplan-Meier analysis,15 in which gestational age was
the timescale, spontaneous delivery was the event, and
Cervical
Expectant
elective deliveries were censored. For purposes of this
management
analysis, all pregnancies were judged to be no longer at
risk at the start of the 34th week. SPPS software package (version 16.0) was used for all statistical analyses.
Maternal age (years)
Interim analyses were done every 6 months.
Body-mass index (kg/m²)
The trial is registered with ClinicalTrials.gov, number
Obstetrical history
Parous with no previous preterm births
Role of the funding source
Parous with at least one previous
The sponsor of the study had no role in study design,
Cigarette smoking during pregnancy
data gathering, data analysis, data interpretation, or
Ethnic origin (self reported)
writing of the report. The investigators had full access to all the data in the study and had fi nal responsibility for
the decision to submit for publication.
Gestational age at randomisation (weeks)
The PECEP trial was undertaken from June, 2007, to
Cervical length at randomisation (mm)
June, 2010. During the study period, 18 235 women with
Funnelling at randomisation (yes)
singleton pregnancies were invited to have transvaginal
Sludge at randomisation (yes)
ultrasonographic measure
ment of cervical length
Data are number (%) or mean (SD).
during the second trimester scan; 11
written informed consent (fi gure 4). Median cervical
Table 1: Baseline characteristics of participants in the cervical pessary
and expectant management groups
length was 34 mm (range 3–68) and 25 mm or less in
www.thelancet.com Published online April 3, 2012 DOI:10.1016/S0140-6736(12)60030-0
726 (6%) women. 385 (53%) women with a short cervix
Cervical
Expectant
Odds ratio
agreed to participate in the trial. They were randomly
pessary group management
assigned to the pessary or expectant management group (fi gure 4).
Pregnancy outcome
Table 1 shows the baseline characteristics. No cervical
Spontaneous delivery before 28 weeks
0·23 (0·06–0·74)
dilation or visible membranes were noted, although four
Spontaneous delivery before 34 weeks
0·18 (0·08–0·37) <0·0001
(2%) of 190 patients had a very short cervix (≤5 mm) in
Any delivery before 34 weeks
0·21 (0·10–0·40) <0·0001
the pessary group (minimum cervical length of 4 mm)
Spontaneous delivery before 37 weeks
0·19 (0·12–0·30) <0·0001
versus six (3%) of 190 in the expectant manage
Gestational age at delivery (weeks)
group (minimum cervical length 3 mm).
Tocolytic treatment
0·23 (0·16–0·35) <0·0001
The primary outcome rate—spontaneous birth before
Corticosteroid treatment for fetal
0·41 (0·26–0·64) <0·0001
34 weeks of gestation—was signifi cantly higher in the
expectant management group (table 2). Four women (two
0·82 (0·20–3·32)
in each group) had medically indicated preterm deliveries.
Pregnancy bleeding
0·77 (0·24–2·38)
The cumulative percentage of patients who did not give
Premature preterm rupture of
0·16 (0·03–0·58)
birth spontaneously before 34 weeks was signifi cantly
Caesarean delivery
higher in the pessary group than in the expectant
manage ment group (fi gure 5). The risk of spontaneous
Vaginal discharge
preterm birth before 34 weeks of gestation did not vary
Pessary repositioning without removal
signifi cantly with respect to maternal age, body-mass index, ethnic origin, obstetrical history, or cervical length
Pessary withdrawal
at the time of randomisation (odds ratio adjusted for
Perinatal outcome
maternal age, body-mass index, ethnic origin, obstetrical
history, and cervical length at the time of randomisation
25·8, 95% CI 7·7–87·1). No diff erence was noted in terms
Birthweight less than 1500 g
0·31 (0·13–0·72)
of bacterial vaginosis between groups at the time of
Birthweight less than 2500 g
0·23 (0·12–0·43) <0·0001
randomisation (pessary group 45 [24%] of 190 vs expectant
management group 47 [25%] of 190).
Necrotising entercolitis
Need for tocolysis was higher in the expectant manage-
ment group (table 2). The most frequently administered
Respiratory distress syndrome
0·20 (0·06–0·55)
tocolytic drug was atosiban, given for 48 h; more patients
in the expectant management group also required more
Treatment for sepsis
0·24 (0·04–0·90)
than one cycle of tocolysis. The need for corticosteroid
Composite adverse outcomes
0·14 (0·04–0·39) <0·0001
treat ment for fetal maturation (two doses of betamethasone
Data are number (%) or mean (SD), unless otherwise indicated. *p value close to zero, odds ratio tends towards infi nity.
12 mg per day, intramuscularly, for 2 days) was greater in
†Grade 2 in all infants.
the expectant management group (table 2). No diff erences were noted in terms of chorioamnionitis (table 2).
Table 2: Primary and secondary outcomes in the cervical pessary and expectant management groups
Signifi cant diff
erences were noted in secondary
outcomes between groups (table 2). The pessary group
Cervical pessary groupExpectant management group
Hazard ratio 0·50 (95% CI 0·41–0·62); p=0·0002
Duration of pregnancy (days)
Number at risk
Expectant management group
Cervical pessary group
Figure 5: Kaplan-Meier plot of the probability of continued pregnancy without delivery in the cervical pessary and expectant management groups
www.thelancet.com Published online April 3, 2012 DOI:10.1016/S0140-6736(12)60030-0
had signifi cant reductions in the rate of birthweight less than 2500 g, respiratory distress syndrome, treat-
Panel: Research in context
ment for sepsis, and composite adverse outcomes. No
diff erences were noted in neonatal mortality rates.
We searched PubMed and our professional networks using
Additionally, no diff erences were noted in terms of
the search terms "cervical pessary" and "preterm birth" for all
iatrogenic delivery rate (any delivery rate excluding
publications related to use of cervical pessaries for the
spontaneous delivery rate was two in each group). Rate of
prevention of preterm birth and reviewed all research studies
premature preterm rupture of membranes was higher in
in which preventive interventions for preterm birth were
the expectant management group (table 2). No major
assessed. Results of non-randomised trials showed benefi ts
adverse events were reported in the pessary group
of cervical pessaries in prevention of preterm birth16,17 and
(table 2). However, all women in the pessary group had
well designed randomised controlled trials to confi rm or
vaginal discharge after placement of the pessary and
refute the benefi t of cervical pessaries were identifi ed in a
some of these women required pessary repositioning
Cochrane review.18
without removal and one patient needed removal and replacement of the pessary (table 2). According to the
results of the maternal satisfaction questionnaire,16 pain
The Pesario Cervical para Evitar Prematuridad (PECEP) trial is
during pessary insertion was ranked as a mean of
the fi rst randomised study of the use of cervical pessary for
4 (scale 0–10) and pain during removal as 7 (0–10); and
prevention of preterm birth. Our results confi rm the benefi t
181 (95%) of 190 patients recommended this intervention
of pessary use in pregnant women with a short cervix. In the
to other people.
context of the published reports, our results provide
Data for pregnancy outcome were also obtained from
evidence that the use of a cervical pessary is an eff ective
11 518 (97%) of 11 875 women in whom cervical length was
intervention for prevention of preterm birth. Clinicians
originally measured; 227 (2%) of 11 518 women had a
should consider using a cervical pessary in asymptomatic
spontaneous preterm birth before 34 weeks. 152 (21%;
pregnant women with cervical lengths of 25 mm or less who
12 in pessary group, 51 in expectant management group,
are at high risk of preterm birth at 20–23 weeks of gestation,
and 89 declined to participate) of 726 women with a
but should take appropriate steps to ensure adverse eff ects
cervical length of 25 mm or less and 75 (<1%) of 10 792 with
are kept to a minimum.
a length greater than 25 mm delivered preterm.
patients than in other studies were included in our study,
The rate of spontaneous birth before 34 weeks of the results matched those of previous studies—a low rate gestation was lower in the pessary group. So far, this of birth at less than 34 weeks of gestation (6%) in the study is the fi rst multicentre, randomised trial of the use
pessary group compared with the expectant management
of a cervical pessary for prevention of preterm birth. group (27%).
However, the potential benefi ts of this device have been
The two groups were well balanced at baseline, which
tested successfully in the past—Arabin and colleagues16
suggests that the pessary could have potential value as a
reported a preterm birth rate before 34 weeks of zero treatment for women at high risk of preterm birth, could when they inserted pessaries into women with short be benefi cial in pregnant women with a short cervix cervical lengths at 22 weeks compared with nearly 50% irrespective of their obstetrical history, and might reduce in a matched control group (panel). Despite the limitation
the risk of preterm birth in nulliparous women. The
of not being a randomised trial, the results were suf-
increase in gestational age at birth in nulliparous women
fi ciently promising to warrant further study.
matched the results of a preliminary report by Arabin
Sieroszewski and colleagues17 described a case series of
and colleagues.16
54 pregnant women. Insertion of a pessary in those with
Interim analysis was done every 6 months. However,
cervical lengths between 15 mm and 30 mm resulted in no conditions for stopping the trial were noted by the an incidence of preterm birth before 29 weeks of 1·9% external data monitoring group.
and a birth-at-term rate of 83·3%. The results of our
We selected the 25 mm cutoff based on the fi fth centile
study are strengthened by the recruitment of nearly in the Spanish population19 and its relation with a 15 000 pregnant women after a midtrimester anomaly substantially increased risk of preterm birth, which has scan. These patients were asked to have a cervical length
been extensively documented.20 Previously, the preterm
assessment, permitting us to detect about 6% of this birth rate for this group was roughly 30%.21 The results of population of women at increased risk of preterm birth. a recent meta-analysis confi rm that 25 mm is the best The women who agreed to participate were randomly cutoff for prediction of preterm birth before 35 weeks.22 assigned centrally at the Vall d'Hebron Hospital, and Our results were better than we had expected.
the follow-up and pessary insertion techniques were
Measurement of cervical length, as a screening test, is
thoroughly controlled. Use of this model conferred used because of its fairly low cost, short learning curve, further support to our fi ndings since, although more and tolerability in patients.23 Additionally, placement of
www.thelancet.com Published online April 3, 2012 DOI:10.1016/S0140-6736(12)60030-0
a pessary is an aff ordable procedure, non-invasive, and We have planned a long-term follow-up of the infants easy to insert and remove when required;16 also, we until the age of 2 years to detect and compare develop-described a new technique for measuring cervical length
mental impairments in the two groups.
in pregnant women inserted with a pessary.13 Further-
Historically, eff orts to reduce prematurity have been
more, assessment of some of our secondary outcomes frustrating. Even the use of pessaries has been showed that severe adverse symptoms were very low in questioned in the past, but the Cochrane reviewers the treatment group. However, patients did have a slight
agree that there is a paucity of well designed trials in
increase (daily occurrence) in white, inodorous, vaginal this respect.18 Finding a safe, economical way (38 euros discharge. Furthermore, 15% of these patients could per pessary) of reducing the incidence of preterm birth feel the pessary inside the vagina after weeks without in the world and reducing the burden of prematurity any symptoms. For this reason, patients should be and its sequelae is a worthwhile goal. Our results open advised to see their doctor if they have any abnormal the door to further research into the use of this device symptoms such as feeling the pessary in the vagina. and give us hope of fi nding a way to substantially reduce Only one case of pessary with drawal was reported in the
the incidence of prematurity and its consequences
entire group and tolerability was not an issue, even in worldwide. Further trials, with much larger samples this case. Our satisfaction questionnaire showed that and the possible commitment of a large number of patients had more pain during pessary removal than centres in several countries, are not only needed but during insertion; however, most recommended this also warranted.24intervention to others. No severe bleeding was reported
In conclusion, the cervical pessary is an aff ordable,
in the pessary group compared with the expectant safe, and reliable alternative for prevention of preterm management group.
birth in a population of appropriately selected at-risk
The mechanism of action of cervical pessaries pregnant women who have been screened for cervical
remains to be clarifi ed. Theoretically, the eff ect relies length assessment at the midtrimester scan.
on their mechanical ability to bend the cervix backwards,
not only slightly elongating it but also changing the MG was the principal investigator at Hospital Vall d'Hebron and wrote uterocervical angle, which not only strengthens the the fi rst drafts of the protocol and report, and is the guarantor for the cervical canal but also diminishes the contact of intact report. LP, CM, and CR contributed to study design and data gathering
at Vall d'Hebron Hospital. LV was the principal investigator at the
membranes with the vagina, somehow preserving Hospital Materno-Infantil de Canarias. ARom contributed to the study its integrity. The suggestion that some physical design and data gathering at this hospital. MJ was the principal intervention, such as a pessary, reduces preterm birth investigator at the Hospital Son Llatzer. ARod was the principal by the change in the uterocervical angle has little investigator at the Institut Universitari Dexeus. BM was the principal
investigator at the Hospital Sant Joan. BS was the principal
biological plausibility. The precise mechanism by investigator at the Hospital de Fuenlabrada. JCBM was the trial which a pessary confers a benefi t is not known, but it statistician. EL was a member of the investigating group at the might support the immunological barrier between Hospital Vall d'Hebron. TH was the cervical assessment coordinator.
EC was the trial coordinator and had the initial idea for the study. LC
the chorioamnion-extraovular space and the vaginal was the chairman and was responsible for the overall supervision of
microbiological fl ora as cerclage has been postulated to
the trial management. All authors reviewed and approved the fi nal
do. Further studies are needed to clarify the mechanism
version of the report.
of action of this device.
PECEP Trial Group
This trial was an open-label study and this could be a Data monitoring committee: Zarko Alfi revic (Liverpool Women's Hospital,
limitation. Although masking was impossible because of
Liverpool, UK), Richard Cooke (Liverpool Women's Hospital, Liverpool, UK), Dave Wright (University of Plymouth, Plymouth, UK).
the nature of the intervention, the use of a pessary might
Trial management group: Silvia Arévalo, Mayte Aviles, Inés Calero,
have aff ected medical decision making.
Nazaret Campo, Manuel Casellas, Marina Folch, Itziar García,
The results of our study did show a signifi cant reduction Francesc Perez, Mª Angeles Sanchez, Juan Sagalá, Anna Suy (Hospital
in the rate of neonatal morbidity. However, the trial was Vall d'Hebron, Barcelona, Spain); Miguel Barber, Jose A Garcia,
Margarita Medina (Hospital Universitario Materno-Infantil de Canarias,
not designed to assess the rate of neonatal morbidity or Canary Islands, Spain); Josep R Pascual, Montserrat Inglés, Pere Cavallé
mortality as a primary outcome. For this reason, the (Hospital Sant Joan, Reus, Spain); Carmina Comas (Institut Universitari eff ect size should be considered. Further studies are Dexeus); Maria Teulón, Rosario del Moral, Mónica Menéndez, needed to confi rm this fi nding. The fi ndings of our trial Silvia Mateos, Amparo Gimeno, Ana Belén Garrido, Ana Alfonso
(Hospital Universitario de Fuenlabrada, Spain).
are based on only about 50% of patients who could have Data analysis group: Santiago Pérez-Hoyos, Juan C Bello, Augusto Sao
taken part in the trial and might have been due to this (Hospital Vall d'Hebron, Barcelona, Spain).
being the fi rst time routine cervical length measurement
Confl icts of interest
had been done transvaginally at the hospitals. However, a
We declare that we have no confl icts of interest. We also declare that we
randomised trial was undertaken with balanced groups. have no confl icts of interest with Dr Arabin.
To use pessaries in the general population, two concepts Acknowledgments
must be taken into account—extensive competence in This study was supported by a grant (Fondo de Investigaciones
cervical assessment is required and strict instructions to Sanitarias number 071086) from the Instituto Carlos III, Madrid, Spain.
We thank Christine O'Hara and Steve Brown for their help with the
see a doctor should be given to patients with a pessary.
www.thelancet.com Published online April 3, 2012 DOI:10.1016/S0140-6736(12)60030-0
English version of this report; all the physicians who recruited
11 Heath VCF, Southall TR, Souka AP, Elisseou A, Nicolaides KH.
individuals for the PECEP trial throughout the country, especially
Cervical length at 23 weeks of gestation: prediction of spontaneous
Ricardo Rubio (Hospital del Mar, Barcelona, Spain), Angels Vives
preterm delivery. Ultrasound Obstet Gynecol 1998; 12: 312–17.
(Hospital de Terrasa, Spain), Celia Barrionuevo, Armando Hernandez,
12 To MS, Skentou C, Chan C, Zagaliki A, Nicolaides KH.
Guillermo Landini, Gustavo Legaz, Romina Castagno, Laura Perdomo,
Cervical assessment at the routine 23-week scan: standardizing
and Guillem Cabero (Hospital Quirón, Barcelona, Spain); participants
techniques. Ultrasound Obstet Gynecol 2001; 17: 217–19.
who agreed to take part in the study; people who sat on the multiple
13 Goya M, Pratcorona L, Higueras T, Perez-Hoyos S, Carreras E,
review committees that helped to refi ne the study protocol, especially
Cabero L. Sonographic cervical length measurement in pregnant
Kypros Nicolaides who worked with us on the complex consent issues;
women with a cervical pessary. Ultrasound Obstet Gynecol 2011;
38: 205–09.
and the Clara-Angela-Foundation for developing and manufacturing the cervical pessaries used in this trial.
14 Hosmer DW Jr, Lemeshow S. Applied logistic regression, 2nd edn.
New York: John Wiley, 2000.
15 Hosmer DWLS. Applied survival analysis: regression modeling
Iams JD, Romero R, Culhane JF, Goldenberg RL. Primary,
of time to event data. New York: John Wiley, 1999.
secondary, and tertiary interventions to reduce the morbidity
16 Arabin B, Halbesma JR, Vork F, Hübener M, van Eyck J. Is treatment
and mortality of preterm birth. Lancet 2008; 371: 164–75.
with vaginal pessaries an option in patients with a sonographically
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology
detected short cervix? J Perinat Med 2003; 31: 122–33.
and causes of preterm birth. Lancet 2008; 371: 75–84.
17 Sieroszewski P, Jasiński A, Perenc M, Banach R, Oszukowski P.
Draper ES, Manktelow B, Field DJ, James D. Prediction of survival
The Arabin pessary for the treatment of threatened mid-trimester
for preterm births by weight and gestational age: retrospective
miscarriage or premature labour and miscarriage: a case series.
population based study. BMJ 1999; 319: 1093–97.
J Matern Fetal Neonatal Med 2009; 22: 469–72.
Koppe JG, Verloove-Vanhorick PSP, Ilsen A. Long-term outcome.
18 Abdel-Aleem H, Shaaban OM, Abdel-Aleem MA. Cervical pessary
In: Kurjak A, ed. Textbook of perinatal medicine, 1st edn. Nashville,
for preventing preterm birth. Cochrane Database Syst Rev 2010;
TN: Parthenon Publishing, 1998: 1362–74.
9: CD007873.
Mercer BM, Goldenberg RL, Moawad AH, et al, and the National
19 Crispi F, Llurba E, Pedrero E, et al. Gestational age-dependent
Institute of Child Health and Human Development Maternal-Fetal
normal values of ultrasonographic measurement of cervical length
Medicine Units Network. The preterm prediction study: eff ect of
in the Spanish population. Prog Obstet Gynecol 2004; 47: 264–71.
gestational age and cause of preterm birth on subsequent obstetric
20 Honest H, Forbes CA, Durée KH, et al. Screening to prevent
outcome. Am J Obstet Gynecol 1999; 181: 1216–21.
spontaneous preterm birth: systematic reviews of accuracy and
Iams JD, Goldenberg RL, Meis PJ, et al, and the National Institute
eff ectiveness literature with economic modelling.
of Child Health and Human Development Maternal Fetal Medicine
Health Technol Assess 2009; 13: 1–627.
Unit Network. The length of the cervix and the risk of spontaneous
21 Celik E, To M, Gajewska K, Smith GCS, Nicolaides KH, and the Fetal
premature delivery. N Engl J Med 1996; 334: 567–72.
Medicine Foundation Second Trimester Screening Group. Cervical
To MS, Fonseca EB, Molina FS, Cacho AM, Nicolaides KH.
length and obstetric history predict spontaneous preterm birth:
Maternal characteristics and cervical length in the prediction of
development and validation of a model to provide individualized risk
spontaneous early preterm delivery in twins. Am J Obstet Gynecol
assessment. Ultrasound Obstet Gynecol 2008; 31: 549–54.
2006; 194: 1360–65.
22 Domin CM, Smith EJ, Terplan M. Transvaginal ultrasonographic
To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH.
measurement of cervical length as a predictor of preterm birth:
Prediction of patient-specifi c risk of early preterm delivery using
a systematic review with meta-analysis. Ultrasound Q 2010; 26: 241–48.
maternal history and sonographic measurement of cervical length:
23 Werner EF, Han CS, Pettker CM, et al. Universal cervical-length
a population-based study. Ultrasound Obstet Gynecol 2006;
screening to prevent preterm birth: a cost-eff ectiveness analysis.
Ultrasound Obstet Gynecol 2011; 38: 32–37.
Cross RG. Treatment of habitual abortion due to cervical
24 Hegeman MA, Bekedam DJ, Bloemenkamp KW, et al. Pessaries in
incompetence. Lancet 1959; 2: 127.
multiple pregnancy as a prevention of preterm birth: the ProTwin
10 Newcomer J. Pessaries for the treatment of incompetent cervix
Trial. BMC Pregnancy Childbirth 2009; 9: 44.
and premature delivery. Obstet Gynecol Surv 2000; 55: 443–48.
www.thelancet.com Published online April 3, 2012 DOI:10.1016/S0140-6736(12)60030-0
Source: http://pessary.info.pl/attached/pessary%20Lancet.pdf
DefenDers unDer Promoting sexual and reProductive rights amnesty International is a global movement of more than 7 million people who campaign for a world where human rights are enjoyed by all. Our vision is for every person to enjoy all the rights enshrined in the universal Declaration of Human rights and other international human rights standards.
Caring for People with Dementia and A Step-by-Step Evidence-Based Approach Visit igec.uiowa.edu for more information and references This approach begins with evaluation and treatment of common causes of behaviors, then uses nondrug approaches to management. Antipsychotics are reserved for severe cases due to potential side