Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Pii: s0002-9149(01)02329-3
An Update on Carotid Ultrasound
Measurement of Intima-Media Thickness
Jacques D. Barth, MD, PhD
Coronary atherosclerosis is a chronic, multifactorial dis-
tomatic period. Several techniques for assessing arterial
ease process. Some individuals with atherosclerosis re-
health are available, including quantitative intima-
ceive treatment in the form of mechanical or pharmaco-
media thickness (QIMT) measurement by carotid ultra-
logic interventions after an acute event has occurred.
sound. QIMT is a safe, validated, and portable method
Others receive treatment in the form of risk factor– based
that may prove highly useful in screening for atheroscle-
systemic intervention, the effectiveness of which is as-
rosis and in providing a surrogate measure for response
sessed by its ability to prevent an acute event. Surrogate
to disease interventions. 䊚
2002 by Excerpta Medica,
endpoints in the study of atherosclerosis interventions
are needed to better define disease course and disease
Am J Cardiol 2002;89(suppl):32B–39B
response to interventions during the prolonged asymp-
Complications of atherosclerosis occur suddenly, unlikely, particularly in the case of systemic therapy
but they are a very long time and asymptomatic in
that must be administered for prolonged durations. For
the making. Most health professionals in the field
example, -blocker therapy may reduce blood pres-
agree on how atherosclerosis develops. A normal
sure but may also adversely affect lipid metabolism.
healthy endothelium is exposed to a variety of dam-
Such potential effects go unrecognized if the effect of
aging factors. Eventually, the healthy tissue is injured
treatment is assessed as effect on the risk factor rather
and endothelial dysfunction results. If the damage
than on the disease process itself—that is, if measures
persists, raised lesions in the vessel wall and athero-
of the effects of treatment on the disease process itself
sclerotic plaques develop, carrying the risk of plaque
are not available or are not used. Similarly, assessing
vulnerability and rupture.1,2 Familiarity with the
response to treatment (and putative effect on disease
course of disease is vital in determining how to de-
course), by assessing response of the risk factor tar-
velop and use surrogate markers in clinical trials,
geted by treatment, fails to take into account the
because different markers may be more appropriate at
different degrees to which different risk factors may
different stages of cardiovascular disease (Figure 1).3
contribute to disease course at different stages of the
The notion that we do not need such markers and can
disease. Most recognized risk factors do not exhibit a
rely instead on observation of symptomatic disease to
linear relation with disease progression. As shown in
trigger treatment or to evaluate effectiveness of treat-
Figure 2, the relation of major reversible risk factors
ment is based on a number of incorrect assumptions
to risk of progression varies, indicating that the time
about the disease process. One assumption is that
point at which the risk factor is assessed is important
acute treatment of a disease event constitutes treat-
in determining the impact of the risk factor. Figure 2A
ment of the disease; this assumption appears to be
shows the linear relation between smoking and pro-
coupled with the assumption that reversal of disease is
gression of disease. Figure 2B shows the relation
still an option after an acute event has occurred. Acute
between serum cholesterol and risk of progression. A
events are almost always treatable, and treatment may
threshold value needs to be exceeded before excess
prevent damage to the heart or vessels. However, it is
levels contribute exponentially to progression, reflect-
well known that in ⱖ25% of patients with coronary
ing the physiologic requirement for cholesterol and
artery disease, their first symptom of disease is sudden
reminding us that there is some limit to the dictum of
cardiac death. The likelihood of reversibility is also
"the lower the better." Figure 2C displays the famous
thrown into question because about 40% of cardiac
"J curve" association of hypertension and risk, and
patients have normal blood pressure and/or normal
Figure 2D shows the "inverse S curve" association of
blood cholesterol levels.
lack of exercise with disease progression.
It also seems to be tacitly assumed that intervention
Some individuals with normal cholesterol levels
based on a single risk factor has a neutral effect on the
have major coronary events. Others with very high
many other potential factors involved in disease pro-
cholesterol levels do not have coronary events. With
gression or in protection from disease—some 250
regard to the latter, consider a recent report of
potential factors by recent count.4 This seems highly
Sijbrands et al,5 who assessed 200 years of a Dutchfamilial hypercholesterolemia pedigree and found
From the Southern California Prevention and Research Center, Encino,
that, although the family members were hypercholes-
California, USA.
terolemic, 40% of them had a normal life span. Instead
Address for reprints: Jacques D. Barth, MD, PhD, Southern Cali-
of using different risk-factor measurements, a triage
fornia Prevention and Research Center (SPARC), 16550 Ventura Bou-levard, Suite #212, Encino, California 91436. E-mail: jbarth@
using quantitative intima-media thickness (QIMT) as
surrogate endpoint would help disease management.
2002 by Excerpta Medica, Inc.
0002-9149/02/$ – see front matter
All rights reserved.
FIGURE 1. Sequence of events leading to adverse outcomes in coronary artery disease if cardiovascular risk factors persist, and pro-
posed technique for assessing disease or response at disease stage. FMD ⴝ
flow-mediated dilation (via IMTHeartScan; Ultrascan
Health Technologies, Salt Lake City, UT); IMT ⴝ
intima-media thickness; IVUS ⴝ
intravascular ultrasonography; MI ⴝ
myocardial in-
farction. (Reprinted with permission from Am J Cardiol.3)
After all, the disease itself should be treated and not a
method that uses ultrasound images and permits quan-
risk factor for the disease. It would appear that the
titative measurements. As with intravascular ultra-
precise mechanism of disease course in such individ-
sonography, QIMT provides a direct assessment of
uals is better determined by a surrogate marker of the
disease. It is suitable for use in all stages of athero-
disease itself than by evaluation of a risk factor, and
sclerotic disease, permitting both diagnosis and fol-
that management of disease, as assessed by such a
low-up evaluation of disease. Specific advantages of
marker, may be preferable to management of the risk
QIMT are: (1) portability, (2) the existence of a large
factor for disease.
reference database, and (3) relatively low cost. The
A surrogate endpoint is a biomarker intended to
large database (⬎26,000 individuals) of Prevention
substitute for a clinical endpoint in a clinical trial.
Concepts, Inc. (PCI, West Los Angeles, CA), with a
Surrogate markers have some inherent limitations. For
long-term follow-up period (ⱕ10 years) of different
example, response, as determined using the surrogate
populations and ethnic groups, makes a reliable out-
marker, may not translate into clinical benefit or sur-
come prediction for cardiovascular and cerebrovascu-
vival benefit and may not be intervention dependent.
lar complications a reality. QIMT findings correlate
Nevertheless, the wait for clinical endpoints, such as
with (1) cardiac and cerebrovascular outcome; (2)
revascularizations, angina, and acute myocardial in-
absolute and relative risk, as assessed by cardiovas-
farction in the prolonged asymptomatic phase of dis-
cular risk factors; and (3) change in risk during disease
ease, can be as long as a decade.6 Development of
management.7–11 The technique has now been used as
surrogate markers allows us to establish prevention
the sole surrogate endpoint in the additional approval
measures during this time frame, and it is hoped that
process of a number of lipid-modifying compounds.
these measurements will provide us a safe, noninva-
Data from the 10-year follow-up study of the Ath-
sive, and reproducible method for assessing the pro-
erosclerosis Risk in Communities (ARIC) study indi-
gression and change of the disease.
cate that the findings, made by imaging the far wall of
Several noninvasive vascular imaging procedures
the common carotid artery, correlate well with all
have been developed as potential surrogate measures
major risk factors.12 This confirms our earlier finding
of disease. It is important to determine whether such
during the Cholesterol Lowering Atherosclerosis
techniques can provide a useful surrogate endpoint to
Study (CLAS) that carotid IMT 1 cm below the bulb
identify high-risk subjects. The focus of this report is
was reproducible and showed a remarkable correlation
on carotid ultrasound measurement of intima-media
with cardiovascular events during 10 years of fol-
thickness (IMT).
low-up study.8,9 A striking finding of that early re-
QIMT is a safe, standardized, and validated
search was that there was no discrepancy over time
A SYMPOSIUM: DOCUMENTING REGRESSION OF ATHEROSCLEROSIS
FIGURE 2. Relation between level of risk factor and risk of progression of disease events for smoking (A), serum cholesterol (B), sys-
tolic blood pressure (C), and lack of exercise (D).
between direction of disease in coronary arteries on
the finding that only the assessment of the far wall of
angiography and on imaging of the carotid IMT; with
the common carotid artery shows significant correla-
hindsight, we appreciate that we had already identified
tion with coronary artery changes. An explanation can
those patients who would benefit from lipid lowering
be found by considering the rheology in the carotid
with a combination of colestipol and niacin after an
tree (Figure 4)16; laminar flow indicative of general-
intervention of only 6 months (Figure 3).13 Data from
ized atherosclerosis is present only proximal to the
the Monitored Atherosclerosis Regression Study
bulb. The coronary arteries also adhere to the laws of
(MARS) confirmed these findings in patients receiv-
physics and therefore have a similar impact on
ing statin therapy.14 Subsequently, in the Pravastatin,
changes in blood flow. These findings are of particular
Lipids, and Atherosclerosis in the Carotid Arteries
interest, because image acquisition of 12 points is a
(PLAC II) study, Byington et al15 confirmed that the
much more time-consuming process than image ac-
part of the carotid tree that most reliably indicated the
quisition of 1 reliable area, and the analyses of these
efficacy of lipid lowering in the coronary tree was the
points cannot always be done by other groups with a
far wall of the common carotid artery. In this study, no
computerized system. In addition, we should realize
other imaging point, not even the aggregate of 12
that plaque formation in the bulb is more dependent on
different points, was significantly correlated with pro-
different risk factors than those for coronary artery
gression or regression of disease. Other studies that
disease. Risk factors for the development of cardio-
we have conducted with different lipid-lowering
vascular plaque formation seems to be different than
agents (eg, rosuvastatin) provide further support for
thickness of the IMT.17
34B THE AMERICAN JOURNAL OF CARDIOLOGY姞
FEBRUARY 21, 2002
FIGURE 3. Change in carotid intima-media thickness during 48 months of treatment with colestipol/niacin (solid circles) or placebo
(open circles) in the Cholesterol Lowering Atherosclerosis Study (CLAS). (Adapted with permission from Arterioscler Thromb.13)
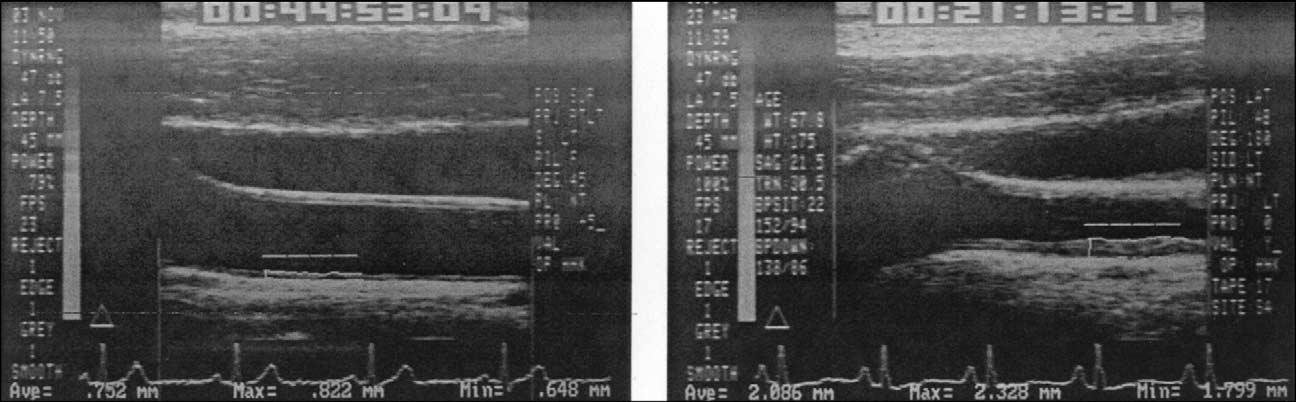
Figure 5 shows 2 examples of digitized images of
the left does not have these major reversible risk
the common carotid artery in 2 patients matched for
factors. It is notable that the near wall of the common
age, sex, and ethnicity. The patient on the right has
carotid artery is difficult to assess, because the focus
hypercholesterolemia and hypertension; the patient on
can be on only 1 part of the picture.
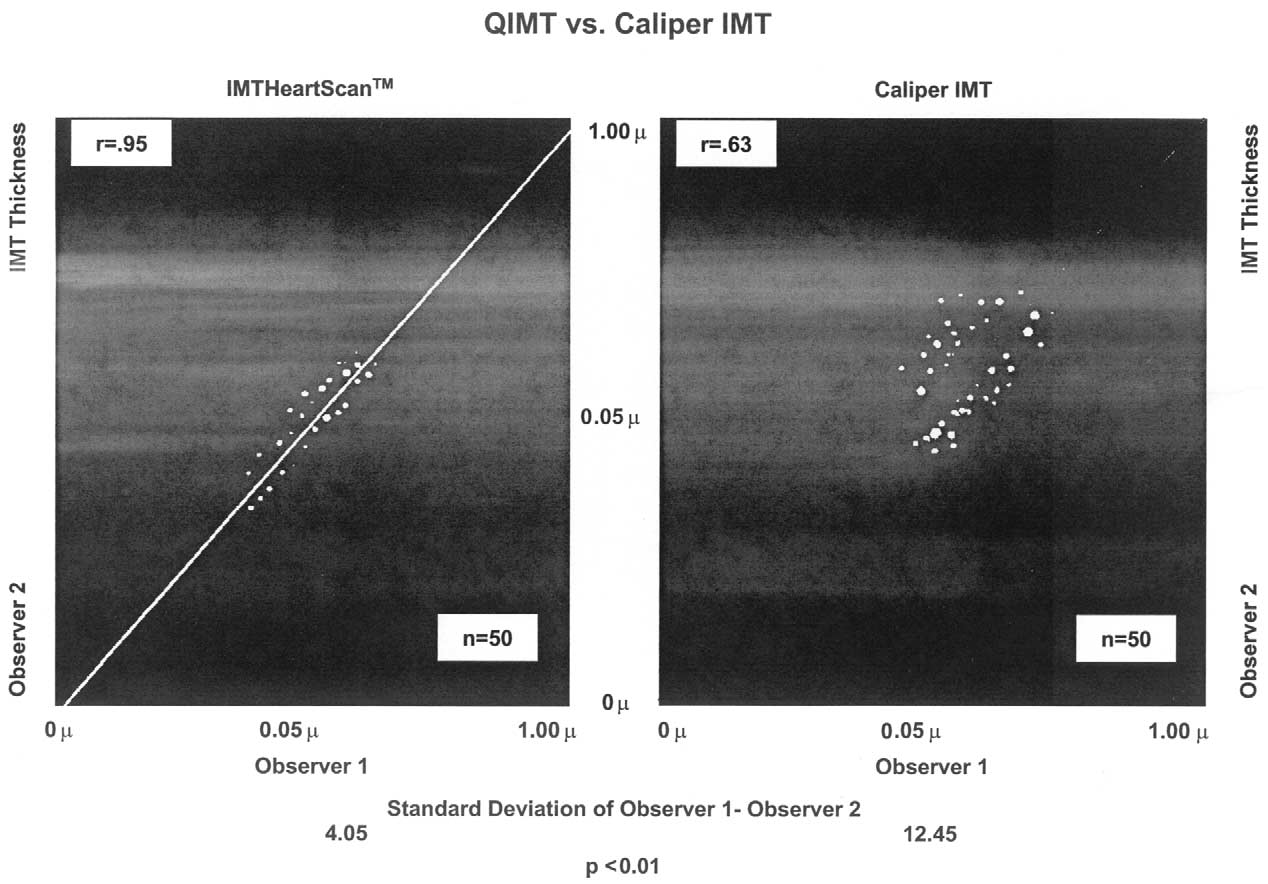
The availability of our large QIMT database has
enabled us to establish that the measurement of the farwall of the common carotid artery alone is the mostreliable and reproducible measurement for predictingcoronary disease. In addition, our comparisons ofmanual and quantitative assessments have made itclear that a computerized contour detection techniqueis far more reproducible and accurate than caliper ormanual assessment (Figure 6). We found that accord-ing to standardized measures, the computer programwas 4 times more accurate than the caliper IMT, andrepeated caliper measurements were within the normalvariation of the technique.
The predictive value of QIMT has been established
in a number of populations. Smoking, blood pressure,and low socioeconomic status are each correlated withcarotid IMT.18–20 Lakka et al18 found that blood pres-sure was significantly correlated with carotid IMT.
Postprandial blood sugar correlates with IMT in indi-viduals without diabetes, as does duration of diseasein patients with diabetes.21,22 In addition, Hanefeld etal21 established that plasma blood sugar level is anindependent risk factor for increased carotid IMT inindividuals without diabetes. The impact of troglita-zone on IMT was found to be dramatic in diabetespatients.23 Both Diez-Roux et al24 and Salonen et al25found that smoking and secondary smoking had apotent effect on progression of carotid atherosclerosis.
FIGURE 4. Depiction of the carotid artery showing the region of
Nevertheless, the predictive accuracy of QIMT varies
flow separation with formation of secondary vortices. Although
among different cultures,26 with Woo et al27 warning
flow remains laminar and mainly unidirectional in the high-shear
that it is sometimes difficult to extrapolate findings
flow-divider area, a very low-shear area is present on the lateral
among individuals with different ethnic backgrounds.
wall of the internal carotid artery. This area is where plaques
are most likely to form and where blood flow accelerates with
Baldassarre et al28 investigated the use of IMT to
each cardiac cycle. (Adapted with permission from Stroke.16)
manage risk factors in the clinical setting, supporting
A SYMPOSIUM: DOCUMENTING REGRESSION OF ATHEROSCLEROSIS
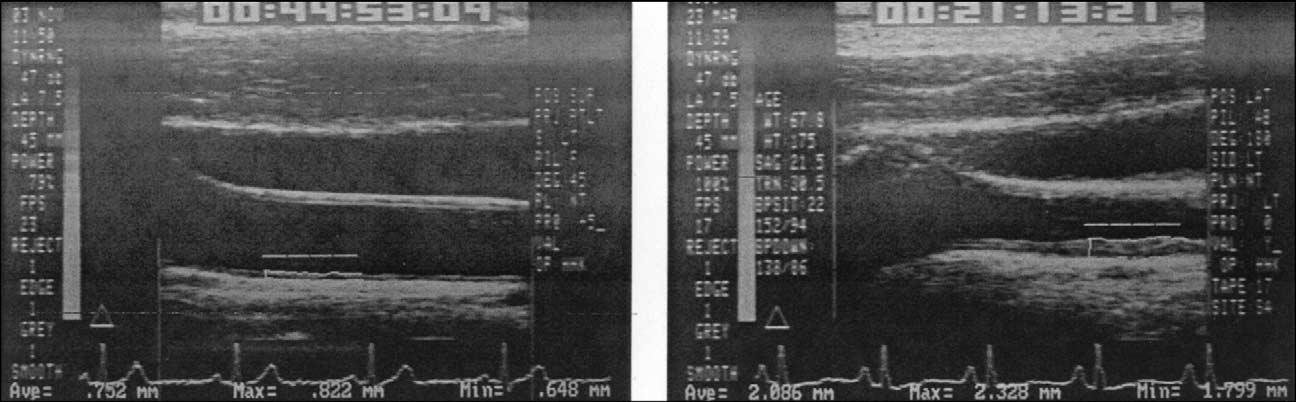
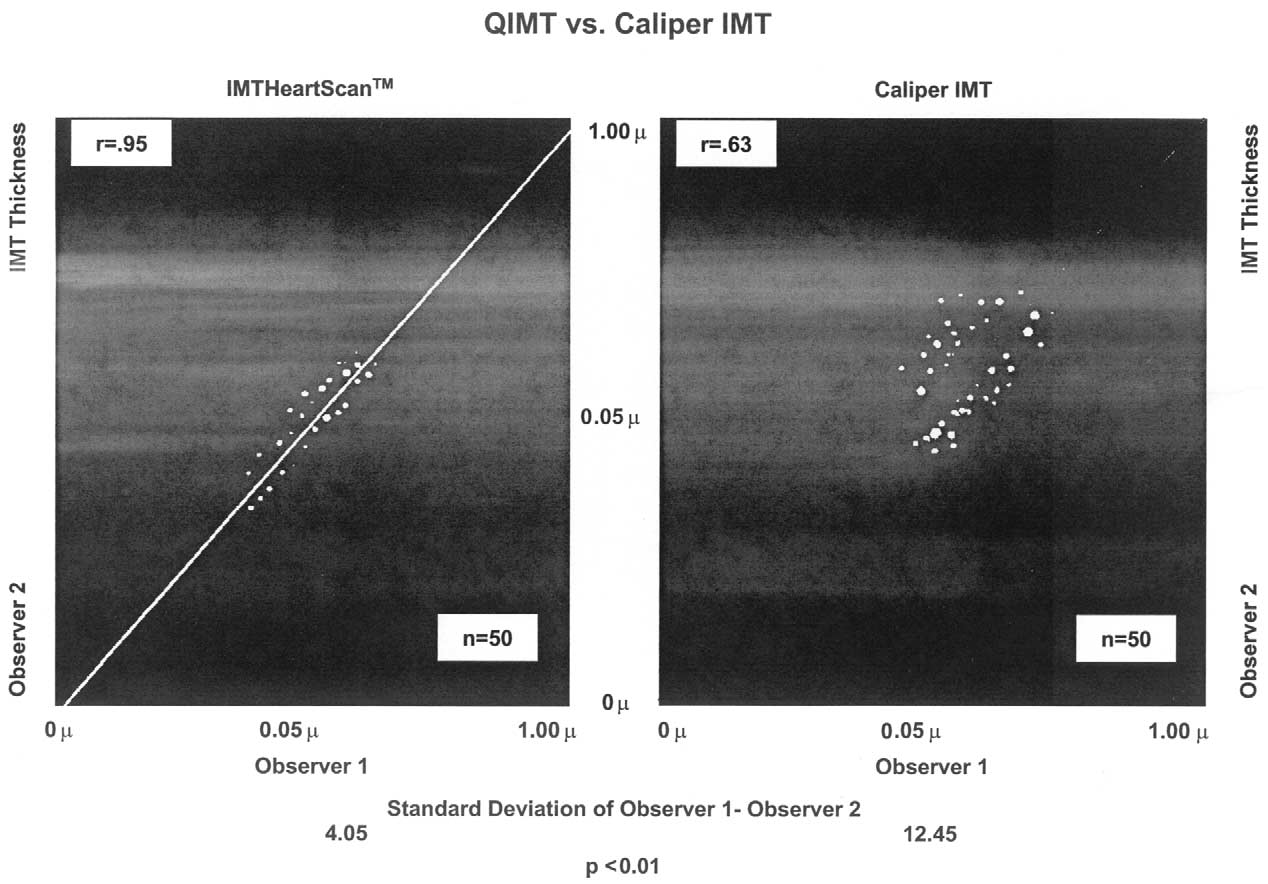
FIGURE 5. Digitized images of the common carotid artery (on the right side of each picture) and the bulb (on the left side of each pic-
ture). The far wall of the common carotid is visible in both pictures, as is the jugular vein, which is located above and parallel to the
common carotid artery. The 1-cm ruler in the middle of the artery indicates where analyses were done. The picture on the right
shows the thickened value in a patient with some hypertension and hypercholesterolemia, whereas the picture on the left shows the
value for a patient matched by age, sex, and ethnicity but without hypercholesterolemia and hypertension. Note the fussy boundaries
in the near wall above the ruler. (Pictures using the Arterial Imaging Software [ARTIS] postprocessing software system, courtesy of
Prevention Concepts, Inc., West Los Angeles, CA).
FIGURE 6. Quantitative intima-media thickening (QIMT; IMTHeartScan, Ultrascan Health Technologies, Salt Lake City, UT) versus cali-
per intima-media thickening. Comparison of absolute laser-measured carotid intima-media thickness (IMT) by user-pointed caliper
method with 2 operators (right) and the same measurement by the same 2 experienced operators using QIMT with a computerized
edge contour measurement technique (left). (Reprinted with permission from Am J Cardiol.3)
our experience of using IMT as a triage point for
olemic, and 14% had a carotid atherosclerotic lesion.30
further risk-factor management. IMT also predicts
This rate of atherosclerosis is consistent with the rate
plaque formation in men and women, independently
of 17% found by Tuzcu et al31 in intravascular ultra-
of baseline plaque.29 Indeed, a study we performed in
sound transplant studies in a young population. More-
13- to 17-year-old high school students showed that
over, providing these young individuals with a cus-
10% were hypertensive, 15% were hypercholester-
tomized image of their carotid artery led many to
36B THE AMERICAN JOURNAL OF CARDIOLOGY姞
FEBRUARY 21, 2002
make lifestyle changes, including weight loss, diet
characterization. Use of magnetic resonance imaging
improvement, and cessation of smoking,30 consistent
may be feasible in the near future in a clinical setting,
with other findings we have obtained in a large, pa-
but the costs of this procedure prohibit its routine
tient group.32 In this latter group, IMT decreased over
clinical use at this time. In addition, magnetic reso-
time in the patients given a customized picture of their
nance imaging is still too experimental for use as an
Risk factors for the development of cardiovascular
Atherosclerosis is prevalent in all countries, and
plaque formation seem to be different than risk factors
clinical trials can be conducted globally in this type of
for IMT thickness.17 In our experience, about 40% of
disease. Therefore, availability of various tests must
plaques are asymptomatic. In these plaques, which are
be considered, because many countries do not have
mostly located in the bulb, tissue type rather than
facilities similar to those in Western countries, which
plaque size is the most important factor for determin-
limits the ability to translate findings consistently from
ing vulnerability to rupture. It has been shown that
country to country.26,27
calcified plaques are not correlated with stroke,whereas soft plaques have a greater likelihood of
rupturing and causing stroke; therefore, an analysis of
In conclusion, atherosclerosis is a multifactorial
the constituents of the plaques is critical.33,34 The
disease, resulting from interaction of multiple risk
Plaque Tissue Typing option provided by Arterial
factors with varying effect over a prolonged course.
Imaging Software (ARTIS; PCI) can help us to deter-
Thus, it is preferable to study the disease and not just
mine whether a plaque has a thin vulnerable cap,
the risk factors for the disease. Furthermore, with
which would make it more likely to rupture than a
many patients not having an abnormal cardiovascular
stable plaque with a relatively small cholesterol core.
risk factor profile, a noninvasive low-cost technique
This computerized system enables us to discriminate
for assessing is disease imperative. QIMT is an ap-
between "hot" and "cold" plaques, the former imply-
propriate technique for use as a surrogate marker both
ing a plaque with increased likelihood of vulnerability
to screen for disease and to manage disease when risk
and rupture and the latter implying a stable plaque.
factors are being modified. QIMT/FMD might be
These findings have been validated, and they indicate
added to several ongoing studies to evaluate the best
that plaque tissue typing would be of great benefit.
marker for different stages of cardiovascular disease.
Other noninvasive imaging techniques include (1)
FMD might be especially suitable if no obstructive
measurement of flow-mediated dilation (FMD), (2)
disease is present, because FMD can detect whether a
electron-beam computed tomography (EBCT) mea-
pathophysiologic state is present. When cardiovascu-
surement of calcium, and (3) magnetic resonance im-
lar risk is present, QIMT is the best method, if there is
aging. FMD assessment of endothelial function is a
endothelial dysfunction and suspected thickening of
good surrogate measure of initial risk for atheroscle-
the far wall of the common carotid artery. Given its
rosis. It indicates very early disease, shows rapid
standardization, QIMT is especially suited to multi-
response to change, is an ambulatory method, and may
center studies. If there is plaque formation, tissue
better reflect pathophysiologic response. However,
characterization should be performed.
outcome studies with FMD are lacking, and disadvan-tages exist, including absence of standards, operatorsensitivity of the procedure, and inability to track
1. Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from
changes because dysfunction either is or is not present
sudden coronary death: a comprehensive morphological classification scheme for
on testing. A study by a group comparing angiography
atherosclerotic lesions. Arterioscler Thromb Vasc Biol 2000;20:1262–1275.
2. Grundy SM. Primary prevention of coronary heart disease: integrating risk
and FMD in evaluating coronary artery disease in
assessment with intervention. Circulation 1999;100:988 –998.
patients and in asymptomatic control subjects showed
3. Barth JD. Which tools are in your cardiac workshop? Carotid ultrasound,
that FMD was better than angiography or cholesterol
endothelial function, and magnetic resonance imaging. Am J Cardiol 2001;87(suppl):8A–14A.
level in identifying the extent of disease.35
4. Hopkins PN, Williams RR. A survey of 246 suggested coronary risk factors.
Another study, evaluating patients with clinical
Atherosclerosis 1981;40:1–52.
5. Sijbrands EJ, Westendorp RG, Defesche JC, de Meier PH, Smelt AH,
signs of coronary disease and matched control sub-
Kastelein JJ. Mortality over two centuries in large pedigree with familial hyper-
jects without disease, showed a significant negative
cholesterolaemia: family tree mortality study. BMJ 2001;322:1019 –1023.
correlation between FMD and QIMT, with the inves-
6. Ogren M, Hedblad B, Isacsson SO, Janzon L, Jungquist G, Lindell SE. Ten
year cerebrovascular morbidity and mortality in 68 year old men with asymp-
tigators concluding that FMD dysfunction may be a
tomatic carotid stenosis. BMJ 1995;310:1294 –1298.
precursor to atherosclerosis.36,37
7. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid
EBCT detects calcifications in the coronary arter-
intima-media thickness and risk of stroke and myocardial infarction: the Rotter-dam Study. Circulation 1997;96:1432–1437.
ies, and its interpretation assumes that cardiovascular
8. Blankenhorn DH, Selzer RH, Crawford DW, Barth JD, Liu CR, Liu CH, Mack
disease parallels extent of calcification. We already
WJ, Alaupovic P. Beneficial effects of colestipol-niacin therapy on the commoncarotid artery. Two- and four-year reduction of intima-media thickness measured
know that soft, not calcified, plaques are the vulnera-
by ultrasound. Circulation 1993;88:20 –28.
ble plaques, which is why the American Heart Asso-
9. Hodis HN, Mack WJ, LaBree L, Selzer RH, Liu CR, Liu CH, Azen SP. The
ciation/American College of Cardiology (AHA/ACC)
role of carotid arterial intima-media thickness in predicting clinical coronaryevents. Ann Intern Med 1998;128:262–269.
expert panel statement did not support EBCT.38 My
10. Hoeg JM. Evaluating coronary heart disease risk. Tiles in the mosaic. JAMA
recent editorial conveys the same blunt message at
greater length.39 Magnetic resonance imaging has
11. Greenland P, Abrams J, Aurigemma GP, Bond MG, Clark LT, Criqui MH,
Crouse JR III, Friedman L, Fuster V, Herrington DM, et al. Prevention Confer-
high sensitivity and specificity for ex vivo plaque
ence V. Beyond secondary prevention: identifying the high-risk patient for
A SYMPOSIUM: DOCUMENTING REGRESSION OF ATHEROSCLEROSIS
primary prevention: noninvasive tests of atherosclerotic burden: Writing Group
and cardiovascular risk factors. Arterioscler Thromb Vasc Biol 1996;16:1388 –
III. Circulation 2000;101:E16 –E22.
12. Sharrett AR, Heiss G, Chambless LE, Boerwinkle E, Coady SA, Folsom AR,
27. Woo KS, Chook P, Raitakari OT, McQuillan B, Feng JZ, Celermajer DS.
Patsch W. Metabolic and lifestyle determinants of postprandial lipemia differ
Westernization of Chinese adults and increased subclinical atherosclerosis. Ar-
from those of fasting triglycerides: the Atherosclerosis Risk in Communities
terioscler Thromb Vasc Biol 1999;19:2487–2493.
(ARIC) study. Arterioscler Thromb Vasc Biol 2001;21:275–281.
28. Baldassarre D, Amato M, Bondioli A, Sirtori CR, Tremoli E. Carotid artery
13. Blankenhorn DH, Hodis HN. George Lyman Duff Memorial Lecture. Arterial
intima media thickness measured by ultrasonography in normal clinical practice
imaging and atherosclerosis reversal. Arterioscler Thromb 1994;14:177–192.
correlates well with atherosclerosis risk factors. Stroke 2000;31:2426 –2430.
14. Alaupovic P, Hodis HN, Knight-Gibson C, Mack WJ, LaBree L, Cashin-
29. Shinnar M, Fallon JT, Wehrli S, Levin M, Dalmacy D, Fayad ZA, Badimon
Hemphill L, Corder CN, Kramsch DM, Blankenhorn DH. Effect of lovastatin on
JJ, Harrington M, Harrington E, Fuster V. The diagnostic accuracy of ex vivo
ApoA- and ApoB-containing lipoproteins. Families in a subpopulation of patients
MRI for human atherosclerotic plaque characterization. Arterioscler Thromb
participating in the Monitored Atherosclerosis Regression Study (MARS). Arte-
Vasc Biol 1999;19:2756 –2761.
rioscler Thromb 1994;14:1906 –1913.
30. Barth JD, Sanchez A, Zhang L, Zonjee MM. A high school student's vascular
15. Byington RP, Furberg CD, Crouse JR III, Espeland MA, Bond MG. Prava-
wall is associated with heart disease risk factors for adults [abstract]. J Am Coll
statin, Lipids, and Atherosclerosis in the Carotid Arteries (PLAC II). Am J
Cardiol 2000;35(suppl A):299.
31. Tuzcu EM, Kapadia SR, Tutar E, Ziada KM, Hobbs RE, McCarthy PM,
16. Hademenos GJ, Massoud TF. Biophysical mechanisms of stroke. Stroke
Young JB, Nissen SE. High prevalence of coronary atherosclerosis in asymp-
tomatic teenagers and young adults. Circulation 2001;103:2705–2710.
17. Barth JD, Shircore A, Zonjee M. Carotid bifurcation plaques exhibit a
32. Barth JD, Zhang L, Zonjee M. A picture tells a thousand words. A person-
different cardiovascular risk factor profile than intima media thickness of the
alized picture enhances a patient's compliance [poster]. AHA Meeting on Patient
common carotid artery. American Heart Association Vascular Biology Meeting;
Compliance, April 29 –30; 1999; Waltham, Massachusetts.
October 26 –28, 1998; San Francisco, California. Abstract 55.
33. Geroulakos G, Hobson RW, Nicolaides A. Ultrasonographic carotid plaque
18. Lakka TA, Salonen R, Kaplan GA, Salonen JT. Blood pressure and the
morphology in predicting stroke risk. Br J Surg 1996;83:582–587.
progression of carotid atherosclerosis in middle-aged men. Hypertension 1999;
34. Grønholdt ML. Ultrasound and lipoproteins as predictors of lipid-rich,
rupture-prone plaques in the carotid artery. Arterioscler Thromb Vasc Biol
19. Koopman JS, Lynch JW. Individual causal models and population system
models in epidemiology. Am J Public Health 1999;89:1170 –1174.
35. Zureik M, Ducimetiere P, Touboul PJ, Courbon D, Bonithon-Kopp C, Berr
20. Zanchetti A. Carotid artery wall alterations as intermediate end points. Clin
C, Magne C. Common carotid intima-media thickness predicts occurrence of
Exp Hypertens 1999;21:595– 607.
carotid atherosclerotic plaques: longitudinal results from the Aging Vascular
21. Hanefeld M, Koehler C, Schaper F, Fuecker K, Henkel E, Temelkova-
Study (EVA). Arterioscler Thromb Vasc Biol 2000;20:1622–1629.
Kurktschiev T. Postprandial plasma glucose is an independent risk factor for
36. Hashimoto M, Eto M, Akishita M, Kozaki K, Ako J, Iijima K, Kim S, Toba
increased carotid intima-media thickness in non-diabetic individuals. Atheroscle-
K, Yoshizumi M, Ouchi Y. Correlation between flow-mediated vasodilation of
rosis 1999;144:229 –235.
the brachial artery and intima-media thickness in the carotid artery in men.
22. Wagenknecht LE, D'Agostino R Jr, Savage PJ, O'Leary DH, Saad MF,
Arterioscler Thromb Vasc Biol 1999;19:2795–2800.
Haffner SM. Duration of diabetes and carotid wall thickness. The Insulin Resis-
37. Barth JD, Zonjee MM, Zhang L, Graziano CR, Manajan M. Early benefits of
tance Atherosclerosis Study (IRAS). Stroke 1997;28:999 –1005.
smoking cessation in young adults [abstract]. Circulation 2000;102(suppl):II-
23. Minamikawa J, Tanaka S, Yamauchi M, Inoue D, Koshiyama H. Potent
inhibitory effect of troglitazone on carotid arterial wall thickness in type 2
38. O'Rourke RA, Brundage BH, Froelicher VF, Greenland P, Grundy SM,
diabetes. J Clin Endocrinol 1998;83:1818 –1820.
Hachamovitch R, Pohost GM, Shaw LJ, Weintraub WS, Winters WL Jr. Amer-
24. Diez-Roux AV, Nieto FJ, Comstock GW, Howard G, Szklo M. The rela-
ican College of Cardiology/American Heart Association Expert Consensus Doc-
tionship of active and passive smoking to carotid atherosclerosis 12-14 years
ument on electron-beam computed tomography for the diagnosis and prognosis of
later. Prev Med 1995;24:48 –55.
coronary artery disease. J Am Coll Cardiol 2000;36:326 –340.
25. Salonen JT, Salonen R. Ultrasound B-mode imaging in observational studies
39. Barth JD. Calcium scores low: ACC/AHA consensus statement on EBCT
of atherosclerotic progression. Circulation 1993;87(3 suppl II):56 – 65.
[editorial]. Int J Clin Pract 2000;54:415.
26. Wei M, Gonzalez C, Haffner SM, O'Leary DH, Stern MP. Ultrasonographi-
40. Neunteufl T, Katzenschlager R, Hassan A, Klaar U, Schwarzacher S, Glogar
cally assessed maximum carotid artery wall thickness in Mexico City residents
D, Bauer P, Weidinger F. Systemic endothelial dysfunction is related to the extent
and Mexican Americans living in San Antonio, Texas. Association with diabetes
and severity of coronary artery disease. Atherosclerosis 1997;129:111–118.
Alan Guerci, MD (Roslyn, New York, USA): With
suggest that there is more soft plaque than calcified
respect to the drawbacks of electron-beam computed
plaque at the site of plaque rupture. However, the
tomography (EBCT), you noted that soft plaques, not
interesting thing is that often both are present, and 1 of
calcified plaques, are most vulnerable to rupturing,
the hypotheses generated is that juxtaposition of soft
and that calcified plaques are not correlated with
and calcified plaque is a predisposing factor for rup-
stroke. However, there are abundant data showing that
ture. This may be why people are making different
calcified plaque in the coronary arteries is a marker for
findings; it may be that having a soft plaque next to a
vulnerable plaque. In a study by von Birgelen et al,1
noncompliant structure is associated with rupture—
pretty much the "bible" on coronary pathology in
however, we don't know that yet.
patients with stable and unstable coronary syndromes,
Dr. Guerci: A couple of years ago, 2 studies had
about 1,300 patients undergoing coronary interven-
autopsy data on ⬎1,200 subjects and showed that
tion were examined by intravascular ultrasound
people dying suddenly or dying of acute myocardial
(IVUS). The investigators, who had no particular rea-
infarction had 3 to 9 times as much coronary calcium
son to be biased for or against EBCT, made a very
as age-matched controls who died accidentally or of
strong statement that calcified plaque on IVUS is a
other natural causes. Another point is that in a slide
Dr. Barth showed, there was a "⫾" next to EBCT for
Steven E. Nissen, MD (Cleveland, Ohio, USA): I
association with clinical outcome. I'm sorry, but that
probably know the IVUS literature as well as any-
is just factually incorrect. Every study looking at the
one—and there is more to this issue. Several studies
issue that I'm aware of has shown a significant asso-
38B THE AMERICAN JOURNAL OF CARDIOLOGY姞
FEBRUARY 21, 2002
ciation between high calcium score and risk of myo-
carotid artery IMT to the coronary arteries. Trials that
cardial infarction or death, consistent with the autopsy
have looked at both show a poor correlation between
data. The question is not whether EBCT predicts hard
coronary angiographic progression and carotid IMT
events, but whether it predicts them as well or better
progression—a correlation value of about 0.2. There-
than standard risk factors. Finally, because I believe
fore, I think the IMT is a great test for the carotids, but
what we're supposed to be talking about is coronary
that's not the heart. Carotid thickening is driven far
disease—not stroke or transient ischemic attack—I
more by hypertension.
don't think the correlation of intima-media thickness
Dr. Nissen: I think we have to be careful in talking
(IMT)– defined carotid pathology and coronary ath-
about correlations, because the data we have to date
erosclerosis is that strong; the number I carry in my
correlate progression of angiographic stenosis in the
head is about 0.4, but Dr. Crouse may know the
coronary lumen versus carotid plaque. We don't know
literature better than I do.
the correlation between progression of the carotid
John Robert Crouse III, MD (Winston-Salem,
plaque and, for example, progression of coronary
North Carolina, USA): The extent of disease in the
plaque on IVUS. Maybe they correlate more closely. I
carotids correlates with the extent of disease in the
think it would be of interest to study whether the
coronary arteries with an r-value of about 0.5. How-
people whose plaques progress by IVUS are the samepeople whose plaques progress by carotid IMT and
ever, the extent of disease in the left coronary artery
whose calcium scores progress on EBCT, and, more
correlates with the extent of disease in the right cor-
importantly, whether drug treatment shows benefits
onary artery with an r-value of about 0.5, too. There-
using each of these endpoints separately.
fore, the carotid artery correlates as well with thecoronary artery as the coronary arteries correlate witheach other.
1. von Birgelen C, Klinkhart W, Mintz GS, Papatheodorou A, Herrmann J,
Christie Ballantyne, MD (Houston, Texas, USA):
Baumgart D, Haude M, Wieneke H, Ge J, Erbel R. Plaque distribution and
I think that there are great data on IMT from clinical
vascular remodeling of ruptured and nonruptured coronary plaques in the samevessel: an intravascular ultrasound study in vivo. J Am Coll Cardiol 2000;37:
trials. However, the big problem is the jump from
1864 –1870.
A SYMPOSIUM: DOCUMENTING REGRESSION OF ATHEROSCLEROSIS
Source: http://preventionconcepts.com.uy/recursos/Prevention4.pdf
Baloney Detection An Essay by Carl Sagan The Fine Art of Baloney Detection The Fine Art of Baloney Detection The human understanding is no dry light, but receives an infusion from the will and affections; whence proceed sciences which may be called "sciences as one would." For what a man had rather were true he more readily believes. Therefore he rejects difficult things from impatience of research;
Internet Symposium on Food Allergens 4(1):2002 Allergen Data Collection - Update: Cow's Milk (Bos domesticus) . Authors in alphabetical order [contact information] Matthias BESLER (Hamburg, Germany) Philippe EIGENMANN (Genève, Switzerland) Robert H. SCHWARTZ (Rochester, NY, USA)