Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
M sc thesis - ids bastian schnabel

The microeconomic impacts of diarrhoeal infections
on rural and suburban households in Uganda
The microeconomic impacts of diarrhoeal infections on rural
and suburban households in Uganda
by Bastian Schnabel
International Development Studies
Student No.: 5760208
Submitted in Amsterdam on the 28.01.2009 to the
Universiteit van Amsterdam
International School of Humanities and Social Sciences
Cover picture: LWI News
Abstract
Health economists, public health workers, and the World Health Organisation are becoming
increasingly concerned about the economic impact of diarrhoeal diseases and about
infectious diseases in general. The direct and indirect economic burdens caused through ill-
health by diarrhoeal diseases impact people especially at the individual and household level.
Also, the financial burdens caused by diarrhoeal infections are suspected to have a huge
impact on the socio-economic and demographic structure of a society (WHO 1996 & 2002).
But even more important, ill-health and infectious diseases often hinder and avert the
development processes of less developed countries.
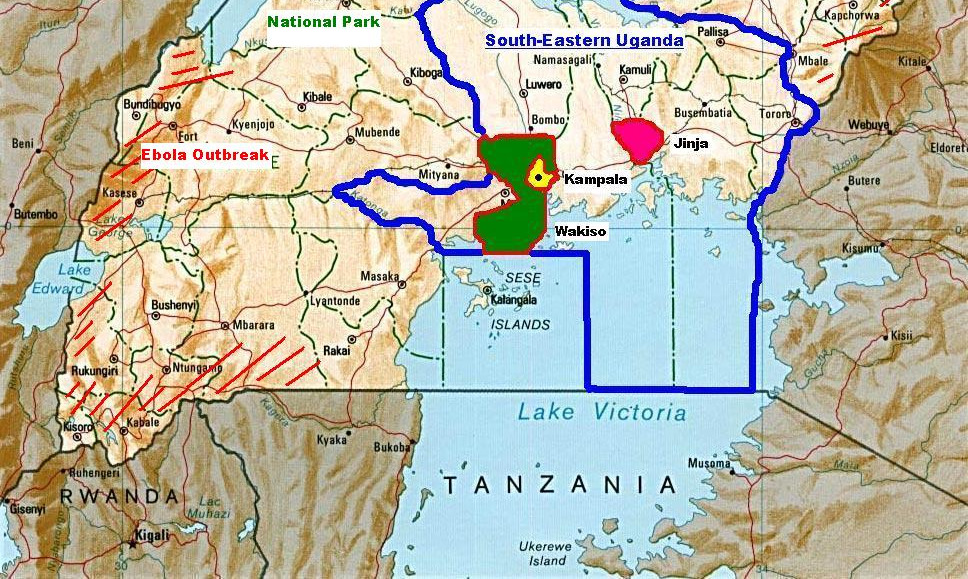
This thesis will analyse how diarrhoeal infections economically impact people at the
household level in Uganda. A field study has been conducted to investigate direct and
indirect financial spending related to the infection of a household member with diarrhoeal
infections, and to find out what economic impact this situation has again on all household
members together. Data have been collected in the three South-Eastern districts Kampala,
Wakiso, and Jinja in Uganda, by applying a household survey, observations, and semi-
structured interviews with health experts.
The analysis shows that households which are impacted by ill-health through diarrhoeal
infections often suffer a large economic and financial burden, which is mainly caused by
expenses for medical treatment and special food. Disease prevention costs can also
substantially decrease the household's financial equity and stability. The study assumes that
on average, the financial burden for households suffering from diarrhoeal infections is as
high as 20% of the total direct and monthly household income, and the costs for disease
prevention alone can be as high as 10% of the household income.
Policy measures and health and sanitation interventions on the communal and
government level are urgently needed to protect especially Uganda's poor people from
further economic pressure caused mostly through preventable diarrhoeal infections. Such
interventions would also bring benefits to the Ugandan macro-economy and would therefore
support overall development.
Table of Contents
List of Figures….…………………………………………………………. 5
List of Tables……………………………………………………………………. 6
1. Introduction………………………………………………………………………. 7
1.1 Introduction………………………………………………………………………. 7
1.2 The economic impact of infectious diseases……………………………. 7
1.3 Diarrhoeal infections, prevalence, and methods of treatment.…………………. 11
1.4 Disease prevention methods………………………….…………………………… 14
1.5 Uganda, its population, and the research locations………………………. 15
1.6 Conclusion………………………………………………………………………… 18
2. Sectoral and policy context………………………………………………….…. 18
2.1 Introduction…………. 18
2.2 The Ugandan health sector.………………………………………………………. 19
2.3 The Ugandan water and sanitation sector…………………………………….…… 22
2.4 NGOs and other organisations involved in health and sanitation practise…….… 24
2.5 Conclusion…………………………………………………………….…………. 25
3. Theoretical framework…….……………………………………………………. 25
3.1 Introduction………………………………………………………………………. 25
3.2 Health economics concerning the economic impact of diseases…………………. 26
3.3 Livelihoods and risk-economics at the household level…………………………. 28
3.4 The medical poverty trap…………………………………………………………. 30
3.5 Rationale for the attention to the economic impact of diseases…………………. 31
3.6 Research question and sub-questions……………………………………………… 32
3.7 Conclusion………………………………………………………………………… 34
4. Methodology……………………………………………………………………… 34
4.1 Introduction………………………………………………………………………. 34 4.2 Epistemology………………………………………………………………. 35 4.3 Conceptual scheme………………………………………………………………. 36 4.4 Definition and operationalisation of concepts……………………………………. 37 4.5 Target population…………………………………………………………………. 41
4.6 Selection of sample size………………………………………………….…. 42
4.7 Sampling methods, variables, and indicators……………………………………. 46
4.8 Data processing and analysis……………………………………………………. 50
4.9 Ethical considerations……………………………………………………. 51
4.10 Conclusion………………………………………………………………………… 52
5. Analysis of locations, households, and of sanitation standards………….…… 53
5.1 Introduction………………………………………………………………………. 53
5.2 Household livelihoods……………………………………………………………. 53
5.3 Living conditions and access to health and sanitation facilities…………………. 55
5.4 Comparison of samples……………………………………………………………. 59
5.5 Conclusion………………………………………………………………………… 60
6. Analysis of the prevalence of disease and ill-health……….…………………. 61
6.1 Introduction………………………………………………………………….……. 61
6.2 Disease prevalence and rate of infection…………………………………….……. 61
6.3 Comparison of samples……………………………………………………………. 63
6.4 Conclusion……………………………………………………………….………. 64
7. Health seeking behaviour………………………………………………. 65
7.1 Introduction…………………………………………………………………….…. 65
7.2 Analysis of the health seeking behaviour………………….……………………. 65
7.3 Chi-square test, regression and scatter plot analysis………………………………. 69
7.4 Special food………………………………………………………………………. 71
7.5 Disease prevention methods……………………………………………….……… 72
7.6 Chi-square test, regression and scatter-plot analysis……………………………… 74
7.7 Comparison of samples and conclusion….………………………………………. 76
8. Economic burden of diarrhoeal infections on households………………….…. 78
8.1 Introduction………………………………………………………………………. 78
8.2 Analysis of the financial impact.…………………………………………………. 78
8.3 Chi-square test, regression and scatter-plot analysis………………………….…. 81
8.4 Comparison of samples and conclusion…………………………………………… 83
9. Risk-economics and coping strategies at the household level……………….… 84
9.1 Introduction…………………………………………………………………….…. 84
9.2 Analysis of risk-economics and coping strategies………………………….……. 85
9.3 Discussion and conclusion………………………………………………….……. 87
10. Discussion and Conclusion……………………………………………. 88
10.1 Introduction…………………………………………………………………….…. 88
10.2 Study limitations…………………………………………………………….…… 88
10.3 Discussion and conclusion of assumptions made…………………………………. 90
10.4 Recommendations………………………………………….……………………… 93
Acknowledgements…………………………………………………………….… 95
References………………………………………………………………………. 96
List of Abbreviations…………………………………………………….……. 101
Appendices………………………………………………………………….…. 103
Household questionnaire………………………………………………….……… 103
List of Figures
Figure 1.1 Salmonella typhi…………………………………………………………….…12
Figure 1.2 Vibrio cholerae……………………………………………………………. 12
Figure 1.3 Map of reported cholera outbreaks in 2005……………………………….……13
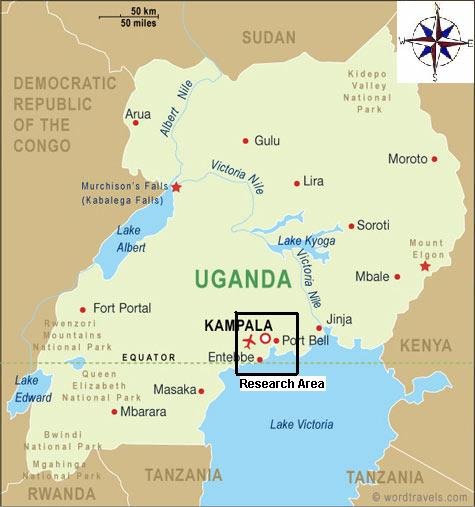
Figure 1.4 Map of Uganda with marked research area……………………………….…. 16
Figure 4.1 Conceptual framework for analysing the economic impact of
infectious diseases……………………………………………………….…… 36
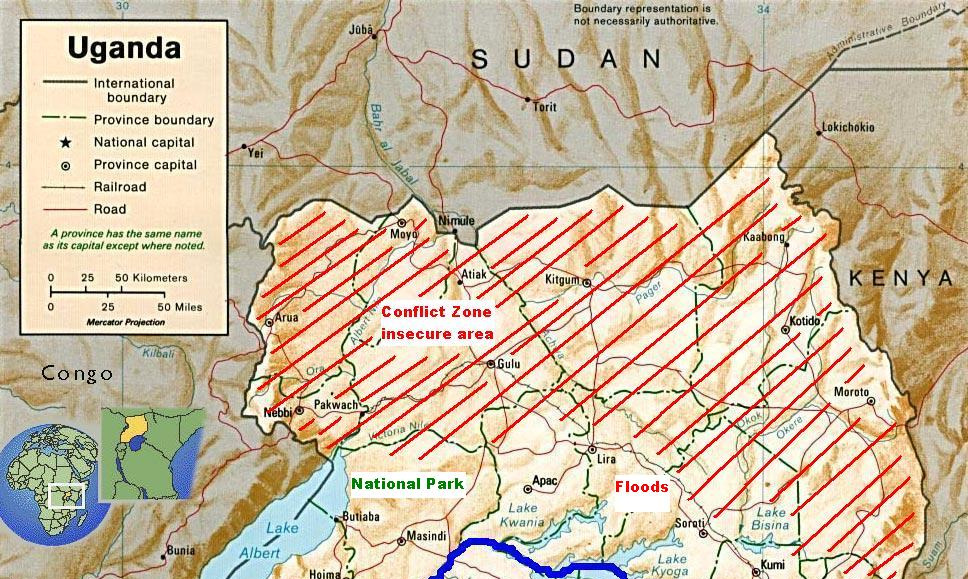
Figure 4.2 Locations of research areas within Uganda……………………………….…. 43
Figure 7.1 Scatterplot of medical treatment costs vs. household income. 71
Figure 7.2 Scatterplot of disease prevention costs vs. household income…………….…. 76
Figure 8.1 Scatterplot of total disease related costs vs. household income……………. 83
List of Tables
Table 4.1 Sample size per study location……………………………………………….… 45
Table 5.1 Household structures by location……….……………………………………. 55
Table 5.2 Mode of occupation, and of water source; and dimensions of housing.…….…. 56
Table 6.1 Rate of households impacted by diarrhoeal infections by location ………….… 62
Table 6.2 Rate of infection compared to No. of episodes and type of
pathogen…………………………………………………………………. 62
Table 7.1 Health care seeking behaviour…………………………………………….…… 66
Table 7.2 Pharmacy consultation only……………………………………………….…… 66
Table 7.3 Time, transport, and company…………………………………………….……. 67
Table 7.4 Medical treatment costs………………………………………………….……. 68
Table 7.5 Association between medical treatment costs and
household income………………………………………………………. 69
Table 7.6 Correlation between medical treatment costs and
household income……………………………………………………. 70
Table 7.7 Special food……………………………………………………………. 72
Table 7.8 Rate of infection versus investments in disease prevention 1. 73
Table 7.9 Rate of infection versus investments in disease prevention 2……………….… 73
Table 7.10 Association between disease prevention costs and
household income………………………………………………………….…. 74
Table 7.11 Correlation between disease prevention costs
and household income…………………………………………………….…. 75
Table 8.1 Income versus rate of infection…………………………………………….…. 79
Table 8.2 Income ratio between infected and uninfected households and
working household members…………………………………………. 79
Table 8.3 Total financial burden caused by diarrhoeal infections……………. 80
Table 8.4 Association between total disease related costs
and household income…………………………………………………. 81
Table 8.5 Correlation between disease related costs and household income. 82
Table 9.1 Range of coping strategies………………………………………………….…. 85
Table 9.2 Household coping strategies 1…………………………………………….…. 86
Table 9.3 Household coping strategies 2………………………………………….……. 86
1. Introduction
1.1 Introduction
The subject of infectious diseases has increasingly gained importance among biologists,
physicians, and epidemiologists since the first pathogens have been identified in the 19th
century. Traditionally, water-born and diarrhoeal infections like e.g. cholera and typhus have
been, and are still of major importance due to their high epidemic potential to infect a very
high number of people in only a very short time. Since the end of World War Two, infections
with diarrhoeal diseases have become less an issue in the Western World, but due to various
climatic and environmental factors, and due to missing infrastructure and insufficient health
systems, they are still a common problem in the less developed world, and especially in Sub-
Saharan Africa. Even more worrying, diarrhoeal infections have become, due to their large
number of incidences, a serious threat for local economies and for the general process of
The first chapter introduces the economic impacts which infectious diseases have on
more and less developed societies, and gives also a description of disease prevention
methods, and of Uganda and its people. First of all, the main issues concerning infectious
diseases will be described in section 1.2 in order to understand the macro- and micro-
economic impacts ill-health can cause. Secondly, a brief biological introduction to the most
common gastrointestinal pathogens will be presented in section 1.3. Thirdly, as the
mitigation of diarrhoeal diseases plays an important role in reducing the burden of infectious
diseases, disease prevention methods will be explored in section 1.4. To get an impression of
Uganda and its people's living conditions, section 1.5 introduces Uganda's topographic and
demographic features. The chapter conclusions are drawn in section 1.6.
1.2 The economic impact of infectious diseases
The economic impact of infectious diseases has been studied since the major outbreaks of
plague and cholera during the middle age in Europe, and is still of major importance for
economists and public health workers today. Especially, when taken into consideration, that a
good health condition is a precondition for any kind of human development and action. Ill-
health can lead to a decrease in human productivity and therefore averts overall development,
which is especially an issue for developing nations (Schultz 1961). According to Schultz
(1961) health is a human capital which we need to protect and invest in to increase the
overall economic output. Ill-health caused by infectious diseases can have many different
economic impacts. The most important direct economic impacts threatening society are:
premature death and consequent loss of productivity, sickness and limited loss of production,
the individual's reduced resistance to other causes of disability or reduced future
productivity, the cost of detection, treatment, rehabilitation of infections, and attempts to
prevent diseases. Also, on the macroeconomic level, poor health affects the size and
composition of the population (Weisbrod 1961).
The social, demographic, and economic burdens caused by ill-health through highly
contagious diseases like for example cholera are experienced by many different regions in
the world, and are still seen, due to their severity and extent, as one of the major obstacles for
sustainable and economic development in Africa. Especially diarrhoeal infections account for
a huge proportion of the global disease burden and mortality, and infections occur
predominantly in tropical regions like Sub-Saharan Africa where there are no or often only
insufficient sanitation facilities available. Moreover, water is increasingly becoming a
dramatic issue on the African continent, as insufficient or contaminated water sources are the
major cause of diarrhoeal infections, respectively, of high child mortality rates (WHO 1996).
For example, in 1998, 308,000 people died of war in Africa, but more than two million died
because of diarrhoeal diseases (WATSAN 2008).
Uganda, located in Eastern Africa in the Great Lakes Region between Lake Victoria
and Lake Albert is one of the hotspots with regard to the prevalence of infectious diseases
causing diarrhoeal symptoms. Due to Uganda's topography, its hot and wet tropical climate,
the prevalence of a wide range of different disease transmitting vectors, and the scarcity of
clean water and sanitation measures, diarrhoeal diseases impact the life of Uganda's
population at all levels, but especially of rural and poor people, and there is suspicion that
this situation might impact Uganda's micro and macro economy and its process of
development (Lucas et al. 1999). According to the Uganda Demographic and Health Survey
2006, malaria and diarrhoeal diseases are the major infectious diseases, impacting the whole
country and especially the western and northern districts; 26% of all children under the age
of five years are, on average, infected with some kind of diarrhoea causing infection (Uganda
Bureau of Statistics 2006). Uganda is also on a regular basis affected by cholera and dysentery
epidemics, and has a high rate of infection with giardiasis, typhoid fever, and hook worms
which further contribute to the overall burden of diarrhoeal diseases.
Various studies in Africa have therefore analysed the different impacts of such
infectious diseases on their victims and their environments, and proved, that infectious
diseases are responsible for a wide range of social and micro- and macroeconomic impacts
on the population (Weisbrod 1961 & 1973; Russell 2004; McIntyre et al. 2006). The
consequences of diarrhoeal diseases are especially a threat for economic growth and
development, and its impacts can be observed on the micro- and macroeconomic level.
Various economic assessments and impact studies from Sub-Saharan African countries with
similar conditions like in Uganda have already outlined some important economic impacts
like e.g. the costs of medical treatment and medication, transport costs to the hospital/doctor,
as well as the loss of household assets at the microeconomic level; and e.g. disease
prevention costs, and the detraction and loss of the labour force at the macroeconomic level
(Russell 2004; WHO 2002). For example, the African Medical and Research Foundation
(AMREF) recons that distance and cost play a major part in Uganda's health crisis, as about
13% of Uganda's people do not seek medical attention because they cannot afford it or
because they cannot reach a health facility. Though, today 72% of the Ugandan population
lives within 5km of a health facility, as compared to 49% five years ago (AMREF 2008).
However, the direct and indirect microeconomic impacts of diseases and ill-health are
different in every country, and due to the lack of sufficient data, there is still a lack in
understanding the relations between disease and economics, and the effects on individuals.
One can already indicate that such economic impacts caused by infectious diseases will
contribute to further poverty, with regard to Whitehead's et al. (2001) medical poverty trap,
which argues that ill-health may lead to more poverty and poverty lead to more ill-health.
Prescott (1999) highlights that a cost burden higher than 10% of the household income is
likely to be catastrophic and it can lead households into poverty. Furthermore, the importance
of analysing economic impacts of diseases is often underestimated, even if such data is
essential for cost-effectiveness analysis in the health and sanitation sector, and for justifying
further pharmaceutical research, and disease prevention methods (Hutton et al. 2004).
In less developed countries (LDCs), diarrhoeal infections are the major killers. For
example in 1998, 2.2 million people died because of diarrhoeal diseases, and most of them
were children under five years of age; and the number of cholera incidents increased in 2006
by 79% (236,896 officially reported cases) (WHO, 2007).
In Uganda, the percentage of diarrhoeal infections in urban areas increased from 2.2% in
2003 to 7.3% of the population in 2006. In the same time, the percentage of diarrhoeal
infections in rural areas increased from 4.4% to 9.8% of the population. In the northern
districts of Uganda, the percentage of diarrhoeal infections reaches as high as 13.8% of the
overall population (Uganda Bureau of Statistics 2006).
Sub-Saharan African has the highest number of diarrhoea and cholera cases, and
cholera has become an important public health issue in western Kenya and Uganda, and may
become an endemic pathogen in this region (Shapiro et al. 1999).
Due to the increasing dissemination and prevalence of diarrhoeal diseases, the social
and economic development of many LDCs, and their prospects of a better future, is being
threatened by the burden of such diseases. For example, the increasing emergence of cholera
has been noted in parallel with the increasing amount of poor and vulnerable populations
living in unsanitary conditions. Therefore, the World Health Organisation (2007) points out,
that diarrhoeal diseases such as cholera remain a threat to public health in LDCs and are used
therefore as a key indicator of social development. Furthermore, diseases can have dramatic
economic impacts at the micro and macro level, and ill-health is increasingly associated with
households being impoverished (DFID 2000). Concern about the relation of diseases, ill-
health, and economic loss has placed health at the centre of development and poverty
reduction strategies (Russell 2004).
The same argument was also put forward by Weisbrod who did some very interesting
and relevant research in North America and the Caribbean concerning the economic impact
of diseases and ill-health, and his studies (1961 &1973) clearly proved, that ill-health has an
enormous impact on the micro and macro economy, particularly in less developed countries.
For example, after the successful eradication of hookworm infections, which mainly cause
diarrhoea, in the American South in the early 1920s, the school enrolment and attendance
rates, and the rate of alphabetisation increased and therefore contributed to the
macroeconomic development (Bleakley 2007). In contrast, there is sufficient evidence that the
parasitic disease schistosomiasis, which causes diarrhoea and which is endemic in most
tropical countries, is responsible for a decline in the overall productivity of the population
impacted. The disease doesn't kill its host, but weakens its physical abilities and therefore
slows down its productivity (Sorkin 1976). Similar effects have been also observed among
populations highly impacted by malaria, which also became less productive. Such situations
will have an impact on the personal and household level as well as on the macroeconomic
level (Sachs et al. 2002; Sorkin 1976). On the microeconomic or household level, incidents of
disease infections often have a huge impact on people's and household's incomes and
savings, as costs for e.g. medical treatment, rehabilitation, and disease prevention can lead to
a financial ruin. Generally, economists must distinguish between direct and indirect
economic impacts, like e.g. the direct loss of household finances, or the indirect loss of
household productive labour, however, both scenarios will have a major economic impact on
the household level (Russell 2004).
Therefore, it's the aim of this thesis to further contribute to the understanding of the
microeconomic impacts of infectious diseases causing diarrhoeal and gastroenterological
symptoms, respectively, to find out how diarrhoeal infections directly and indirectly impact
individuals in Uganda at the household level.
1.3 Diarrhoeal infections, prevalence, and methods of treatment
To fully understand the relationship between economics and ill-health, one should have a
closer look at the definition and concepts of ill-health and diarrhoeal infections, respectively,
how they impact individuals in physiological terms.
Diarrhoea and dysentery are not diseases themselves; they are symptoms of many
diseases and mostly of gastroenterological and gastrointestinal infections. Infectious diseases
causing diarrhoea are on average the most dangerous illnesses, and they kill over two million
people every year, mostly children under the age of five years. There are approximately four
billion cases of diarrhoea world wide each year, which can be caused by a variety of more
than 100 different pathogens including bacteria (e.g. cholera), protozoa (e.g. schistosomiasis)
and viruses (e.g. rotavirus) (WaterAid UK 2007). Pathogens causing diarrhoeal infections are
spread through contaminated food (food-borne disease) or drinking-water (water-borne
disease), through unsanitary disposal of human waste, or from person to person as a result of
poor hygiene (WaterAid UK 2007). Though, many infectious and non-infectious diseases can
cause symptoms of diarrhoea like e.g. malaria or cancer, this study tried to concentrate on
victims and patients affected by the major water-borne and water-related pathogens causing
diarrhoea. These are, according to the WHO, Ancylostoma duodenale, Camplyobacteriosis,
Cryptosporidium, Entamoeba histolica, Escherichia coli, Giardiasis intestinalis, Norovirus
(virus type: Caliciviridae), Salmonella typhi and bacteria, Shingella enteritis, Rotavirus
(virus type: Reoviridae), and Vibrio cholerae. However, because no diagnostic laboratory
tests have been conducted, the researcher can not exclude the possibility that this study
included victims suffering from diarrhoea which has been caused by a disease not related to
the above described criteria.
According to a survey conducted by the Ugandan Bureau of Statistics (2006), are the
percentages of households in urban and sub-urban areas, which have been impacted by at
least one case of diarrhoea two weeks prior the survey, with on average 19.7% much lower
compared to 26.5% in rural areas.

Generally, diarrhoeal infections cause fast depletion of water and sodium in the
victim's body, and if these are not replaced quickly, the victim becomes dehydrated and its
salt and physiological balance becomes severely damaged. If more than 10% of the body's
water is lost, the victim dies. Children, old people, and people who are malnourished or
already weak are most vulnerable to such symptoms, and become even weaker and more
malnourished. The three diseases responsible for most diarrhoea related death are bacillary
dysentery, Vibrio cholerae, and Salmonella typhi (see Figure 1.1 and 1.2), and these
pathogens are highly endemic in Africa's Great Lakes Region.
Bacillary dysentery is more dangerous compared to amoebic dysentery, and it is
estimated that 140 million people get infected with this bacteria each year, and more than
300,000 victims don't survive this infection, mainly children below the age of five years
(WaterAid 2007). One of the areas with the highest prevalence is Sub-Saharan Africa.
Bacillary dysentery is caused by the bacterium Shingella enteritis, which is transmitted via
contaminated water, food, and arthropods (e.g. flies), and which then infects the intestines.
Figure 1.1 Salmonella typhi Figure 1.2 Vibrio cholerae
(Source: WHO 2008)
The major symptom is severe watery and bloody diarrhoea. Treatment is usually based on an
oral rehydration salt solution, high intake of fluids, and in some cases on antibiotics such as
e.g. Ciproflax® (WHO 2008).
The highly infectious disease cholera, which is caused by the bacterium Vibrio
cholerae, is often described as the classic water-borne and diarrhoea causing disease (Sack et
al. 2004). The pathogen is mainly transmitted via contaminated water and food, and is
endemic in most tropical and sub-tropical regions. Originally, the pathogen was only
endemic in the Indo-Bengal region, but it spread in the 18th century all over the world and
caused severe pandemics and left thousands of people death. Similar to Shingella enteritis,
cholera kills mainly children between the age of two and four years, as well as old people,
and people suffering from malnutrition. In 2000, 118,932 cases of cholera were reported in
Africa, and officially 4,690 people died. The number of unreported cases was probably much
higher (Naldoo et al. 2002). Major symptoms are severe watery diarrhoea (adults can lose
more than 14 litres of body fluids a day) and vomiting. Treatment is based on the concept of
replacing fluids as fast as they are being lost, followed by the intake of oral rehydration
solution (ORS) or an intravenous polyelectrolyte solution. Antibiotics can shorten the time of
recovery, but should only be used in limited cases as they increase the risk of the
development of resistant bacteria (Sack et al. 2004). The prevalence of cholera (in 2005) can
be seen in the epidemiological map below (Figure 1.3).
Another very common diarrhoea causing disease in Africa is typhoid fever, which is
caused by the bacteria Salmonella typhi. It is estimated that typhoid fever infects
approximately 17 million people per year, and about 600,000 infected people die each year
(WaterAid 2007). Almost all typhoid cases occur in less developed countries as the pathogen
is virtually eliminated in the developed world through sanitation facilities and vaccines. The
disease causes high fever, diarrhoea, and in some cases even intestinal haemorrhaging or
perforation. In contrast to cholera infections, victims infected with typhoid are often long-
term carriers who spread the pathogen over a long time period (Sack et al. 2004). A vaccine
against typhoid is available, but doesn't provide full protection against infection. Typhoid
fever is mainly treated with antibiotics (WHO 2008).
Figure 1.3 Map of reported cholera outbreaks in 2005 (Source: GISed 2008)
However, the most common infection causing symptoms of diarrhoea in tropical
regions and especially in Africa is an infection with hookworms. It is estimated that about
740 million infections occur through this protozoa in the world's tropical and sub-tropical
regions each year (Hotez et al. 2004). In Sub-Saharan Africa the disease (which often becomes
chronic) is mostly caused by the hookworm Ancylostoma duodenale, which penetrates the
skin or mucous membranes from contaminated soil, water, or food items. The worm then
lives in the small intestines and causes major blood losses into it, which often results in
anaemia, especially in people whose dietary iron level is already low (Feachem et al. 1986).
Children are very vulnerable to this disease as an infection with hookworms can damage their
growth and symptoms can become chronic. The disease can be treated with a single dose of
albendazole, mebendazole, levamisole, or pyrantel, which is the standard treatment for all
infections caused by soil-transmitted helminths (WHO 2002).
1.4 Disease prevention methods
Appropriate and fast treatment is very efficient in reducing the mortality from diarrhoeal
infections, however, this can not reduce the agents responsible for the infection nor does it
decrease the incidents of diarrhoea. The prevention of infectious diseases is one of the key
factors to reduce the human and economic burden caused by the disease. Prevention of
diarrhoea primarily means to protect susceptible people most at risk (these are children, old
people, and people who are already ill or weak) from acquiring diarrhoea causing diseases.
Adequate food, safe water, and personal hygiene are the key words for proper diarrhoea
prevention techniques (Mukhopadhyay et al. 2005).
The WHO (1990) has given priority to the following strategies and interventions for the
prevention of diarrhoeal infections:
First, the promotion of exclusive breast feeding during the first 4 to 6 months of life, because
immunological properties in the breast milk help to protect infants from infection and breast
milk is generally clean.
Second, improved weaning practise, this requires the selection of nutritious food for children
over 4 to 6 months old, and good hygienic education and practice such as e.g. washing hands
before and during food preparation.
Third, the risk of getting infected with a disease causing diarrhoea can be significantly
reduced by using exclusively clean and disinfected water. Prevention of the contamination of
stored water at the household level is therefore important to decrease the transmission of
diarrhoeagenic pathogens. The preferred methods are boiling water or chemical treatment.
Fourth, personal hygiene like proper hand washing with soap and water before preparing
food, before feeding children, and during ablution reduces diarrhoeal infections. House and
kitchen hygiene is also important for the prevention of diarrhoea related diseases.
Fifth, constant access and use of clean, functioning latrines and proper disposal of faeces of
both humans and animals are essential in preventing the spread of pathogens causing
diarrhoea. And last, immunisation against measles reduces the incidents of measles related
diarrhoeal symptoms (WHO 1990). There are also vaccines widely available against the
infections with typhoid, cholera, rotavirus, and Shigella, though they are expensive and still
lack full effectiveness. These prevention measures are especially important during post flood
or post cyclone situations. Also, the supply of safe drinking water and the vaccination of
children against measles are always the first steps to be taken (Mukhopadhyay et al. 2005).
For example, the Water and Sanitation Resource Centre in Uganda (WATSAN) recons that
the simple act of washing hands with soap and water can reduce diarrhoeal infections by one-
third (WATSAN 2008). Furthermore, health officials, local communities, and households must
be actively involved in the process of planning and implementing water resource projects. If
local people have power over their own water sources, they are more likely to protect them
(Hunter et al. 1993).
1.5 Uganda, its population, and the research locations
The field research and data collection for this study took place in Uganda, which is located in
East Africa in the Great Lakes Region between Kenya and the Democratic Republic of
Congo. The topography of the country is defined by tropical bushland, tropical rain forest,
and tropical mountain forest, and the meteorology is strongly influenced by two rain seasons
(from March until June and from September until November). The climate in Uganda during
the field research period was wet and hot and very humid with temperatures between 20˚C
and 35˚C and a high rate of rainfall due to the impact of the main rain season lasting from
March until June.
The Republic of Uganda gained independence from the United Kingdom in 1962, and
is currently governed by the democratically elected President Lt. Gen. Yoweri Museveni who
has held on to power since 1986. Uganda is also, together with Kenya and Tanzania, part of
the East African Community (EAC). The country has 29 million inhabitants, with about 85%
of the population living in rural areas, and with 1.9 million people living in the capital
Kampala. The official language is English, but tribal languages like Luganda, Luo, Iteso
Rwanyankole, and Swahili are also widely used. The Baganda are with 16.9% of the
population the largest ethnic group in Uganda followed by the Banyakole with 9.5% and the
Basoga with 8.4% (CIA factbook 2008). The major minorities in Uganda are international and
internally displaced people (refugees) who in the main have migrated from war suffering
neighbouring countries like the Democratic Republic of Congo, Rwanda, and South Sudan.
But also from Northern Uganda, where a rebel group called the Lord's Resistance Army
abducted more than 20.000 children and displaced more than one million people (Human
Rights Watch 2008).
These internally displaced persons (IDPs) live in hundreds of IDP-camps all scattered across
Northern and Central Uganda.
Despite some unrest in Uganda's north and along the borders, the economy is growing
and the national monthly average income per person and capita for all districts in Uganda is
about $90, though a high proportion of the salaries are earned through the informal business
sector. The national alphabetisation rate is 67%, but school attendance in urban and suburban
areas is generally higher than in rural areas (CIA factbook 2008).
The study locations for suburban interviews were located in and near the Ugandan
capital Kampala, and for rural interviews they were located in the surrounding districts
Wakiso and Jinja in the South-Eastern part of the country.
Figure 1.4 Map of Uganda with marked research area
The few urban areas in Uganda often still impart a rural expression compared to other
East African cities. Thanks to the equatorial climate and the high fertility of the soil, there are
plants and crops growing everywhere in urban places, even next to major roads in the city
centres. Apart from the commercial and traffic impacted city centres and from the nice and
green expatriate settlements, the majority of the poor urban and suburban population lives in
suburbs and slums scattered around the city centres. The target population for this study are
people who live in such slums mainly around Kampala and in rural communities in
neighbouring districts. The main forms of people's livelihoods located in slums are based on
small-scale businesses, on wage and day labouring, and on begging. Livelihoods are mostly
structured very simply and usually concentrated only on gaining basic needs for survival.
During the rainy seasons, these slums are often impacted by floods, and often the slums lack
the most basic infrastructure like paved roads, adequate housing, electricity, or piped fresh
water and sanitation facilities.
Rural areas in South-East Uganda like the districts Wakiso and Jinja are shaped mostly
by tropical bushland as well as by large tea, banana, and cane sugar plantations. The villages
and their fertile fields lie between forests and wetlands as the districts Wakiso and Jinja are
located next to Lake Victoria. Jinja district is also shaped by the magnificent source of the
Victoria Nile River, which crosses the whole district from south to north.
The livelihoods of households located in rural places were predominantly shaped by
subsistence farming and by wage labouring through the commercial farming sector. Though,
most forms of livelihoods in rural places were as simple and basic as in the suburban slums,
most households were at least self-sufficient due to subsistence farming.
The shape and the level of infrastructure in villages depend usually on the region in Uganda,
on its topography, and on its accessibility. Some rural communities, especially the ones near
the capital Kampala, even have access to electricity and to tap water, while people in more
remote rural communities still live very traditional without any infrastructure. With regards
to water supply and sanitation, the access to a clean water sources in Uganda has increased
from 44% in 1990 to 60% in 2004. During the same timeframe, sanitation coverage has also
increased considerably. However, water and sanitation coverage in rural areas, where 88% of
the population lives, is lower than in urban areas (WHO & UNICEF 2006). In urban areas,
fresh water is usually supplied by the National Water and Sewage Corporation (NWSC), a
public corporation working on a commercial basis. In contrast, in rural areas, the local and
district governments are responsible for adequate water supply and sanitation coverage
Additionally, every slum and every village, or a part of it, is controlled and
administered by a chief or community leader who manages local concerns, and most
business, development, and research related activities must be first approved by him. The
chief or community leader usually belongs to the main ethnic group dominating in the region
and is very respected by all community members.
1.6 Conclusion
This chapter introduced and outlined the severe macro- and micro-economic impacts which
diarrhoeal disease can have on societies, by giving at the same time an insight into the
biological part of this subject. Major micro-economic impacts caused through ill-health have
been identified as premature death and the consequent loss of productivity, sickness and the
limited loss of production, the individuals reduced resistance to other causes of disability, the
costs of detection, treatment, rehabilitation, and of attempts to prevent ill-health. The
researcher briefly introduced the most common gastrointestinal pathogens like e.g. cholera
and typhus, and also highlighted how infections with them can be prevented. The sub-chapter
about disease prevention showed, that it is not too late nor is it impossible to reduce the
burden of infections, preconditioned people and governments show concern and provide the
needed finances to condemn this global problem. As the study took place in Uganda, we have
also briefly learned about its topography and its demography to get an impression about local
conditions and setting.
2. Sectoral and policy context
2.1 Introduction
The present chapter presents and outlines the sectoral and policy context in which this study
took place. First of all, a summary of the different agents and sectors which are involved in
the prevention and treatment of ill-health and diarrhoeal infections will be given in section
2.2 in order to understand the complexity of Uganda's health system and its connections and
dependencies to related sectors. Secondly, as the level of sanitation plays an important role in
people being at risk to diarrhoeal infections and to ill-health, the water and sanitation sector
and its related policies will be explained and discussed in section 2.3. Thirdly, in section 2.4,
NGOs and other organisations involved in health and sanitation practise, respectively their
roles and activities will be described. The chapter conclusions are drawn in section 2.5.
2.2 The Ugandan health sector
According to Uganda's Health Sector Strategic Plan 2, which main purpose it is to guide and
to manage the national health sector, there are a number of different sectors and agents
directly and indirectly involved in the health prevention, delivery, and policy process. Apart
from the Ministry of Health, following government sectors are counted to the health related
sector and are also actively involved in fighting diarrhoeal infections:
1. Ministry of Finance, Planning and Economic Development
• Mobilisation of resources 2. Ministry of Lands, Water and Environment
• Mapping availability water sources for all health facilities • Development of water sources • Provision of sanitary services 3. Ministry of Gender, Labour and Social Development
• Mainstreaming gender in plans and activities of all sectors including the engendering of the budget • Development of policies for social protection of the vulnerable groups 4. Ministry of Works, Housing and Communication
• Construction and maintenance of roads for accessing health facilities to facilitate patients flow and referral of patients 5. Ministry of Education
• Interpreting information for promoting and adopting healthy lifestyles • Incorporating public health training into the curricula of schools at all levels • Training of health workers • Research and development 6. Ministry of Local and District Governments
• Recruitment and deployment of appropriate trained staff health workers by District Service Commissions • Delivery of health services • Supervision and monitoring of health service delivery
(Uganda Ministry of Health 2005) As outlined above, Uganda's national health system is shaped by different sectors and agents,
and consists of public health facilities including the health services of the army, police, and
prisons, and of private health delivery systems. However, most institutions directly involved
in health delivery are controlled and managed by the Ministry of Health, and as it is beyond
the scope of this study to consider all agents involved, the health sector itself will be in main
focus in this sub-section.
The private health sector is divided between private-not-for-profit organisations (PNFP)
including missionary health centres, private health practitioners (PHP), and between the
traditional and complementary medicine practitioners (TCMP). Some communities also
provide private health services (Uganda Ministry of Health 2005). Public health facilities are
divided into different levels. They are structured in national level institutions, national
referral hospitals, regional referral hospitals, district health services, and in sub-district health
services like local health centres and village health teams. In contrast to private health
services, medical services provided by the public health facilities are now generally free of
charge, even if Christiaensen et al. (2005) argue that payment for both public and private
health facilities has in practise long been the norm in Uganda (Christiaensen et al. 2005).
However, according to interviews, there are a lot of public health facilities short on adequate
medication and on medical equipment, and patients are often forced to buy the prescribed
medication by themselves through the private health market. Furthermore, according to
Christiaensen et al. (2005) and to various articles published in the local press, corruption and
illicit practise as well as the employment of unqualified staff are not unseen within the public
health services.
However, the Ugandan Ministry of Health has created a public private partnership for
health to improve health services and relations between both sectors. Efforts will be directed
to strengthening and broadening the partnership through more active engagement with other
health related sectors, professional associations, private health care providers, civil society,
and representatives of the principal consumers (Uganda Ministry of Health 2005). The Ugandan
Ministry of health is also concerned about the equitable access for vulnerable communities
and individuals to health services, and therefore included a policy in its Health Sector
Strategic Plan 2 to support these people (Uganda Ministry of Health 2005). The public health
sector considers vulnerable individuals and high-need groups as poor people, children,
orphans, elderly people, women, displaced people, and people living in areas with insecurity.
The efforts of the Ministry for Health are particularly accomplished through increased
funding to primary health care services, the abolition of user fees, and through the targeted
use of the Primary Health Care Conditional Grant (Uganda Ministry of Health 2005).
Furthermore, due to the fact that over 75% of Uganda's disease burden is considered to
be preventable as it is primarily caused by poor personal and domestic hygiene and
inadequate sanitation practices, the Ministry of Health increasingly supports health
promotion, disease prevention strategies, and community health initiatives, and included new
policies concerning these issues in its Health Sector Strategic Plan 2. Diarrhoeal diseases,
which are suspected of diminishing productivity and increasing poverty, are on top of the list
of preventable diseases (Uganda Ministry of Health 2005). Therefore, the public Mulago
Hospital in Uganda's capital Kampala has created a diarrhoea management unit, which
specialised on paediatric treatment and on epidemiological research.
With regards to the health policy frame work, Uganda has developed (together with
international partners and advisors, notably UNICEF), a compact policy frame work that
aims at the improvement of Uganda's health status and at decreasing infectious diseases.
Especially, the Health Policy Advisory Committee (HPAC) has proved beneficial in
providing overall policy guidance to the sector (Uganda Ministry of Health 2005). The lead
paper of this frame work is the Health Sector Strategic Plan, which has first been introduced
in 2000 after the introduction of the newly created National Health Policy (1999). The
policies included in the plan focus on cost sharing of health services, on setting up health
management committees that include participation from local communities, and on the
abolishment of user fees. With regards to the study's focus, the policy's paragraph about the
abolishment of user fees is very interesting, as it is suspected to have a positive effect on
people who are impacted by diarrhoeal infections, because it decreases the financial burden
of patients who seek care in public health facilities. As required by the National Health
Policy (1999), the Health Sector Strategic Plan focuses as well on health promotion, on
disease prevention, and on equitable access to health services for vulnerable communities
and people (Uganda Ministry of Health 2005). Following targets of the Health Sector Strategic
Plan are especially interesting with regards to the study's focus and research question:
- reduction of incidences of annual cases of epidemic diarrhoeal diseases from 3/1000
- reduction of the cholera specific case fatality rate from 2.5% to 1.0%
- increase of the proportion of patients with epidemic diarrhoea receiving appropriate
treatment within 12 hours of onset of symptoms
Subsequently, following core interventions of the Health Sector Strategic Plan are as well
very interesting with regards to the study's focus and research question:
- Diarrhoeal disease surveillance, and epidemic preparedness and response
- Prompt and appropriate case management
- Community education and mobilisation
- Reactivation of the Protocol of Cooperation of Countries in Great Lakes Region
Unfortunately, there is no national or social health insurance system in Uganda yet, but
the Ministry of Health is currently in the process of drafting the law and legal base to govern
the scheme. To provide further support for the subsidisation of medical costs, Community
based Health Insurances Schemes (CBHI) have recently been introduced. However, low
recruitment and retention rates, high management costs, and low uptake by poor people slow
down its success. Still, inadequate financing remains the major constrain inhibiting the
development of the national health sector in Uganda and the funding of health services has
dramatically declined (Lucas et al. 1999). For example, funding a basic package of services in
developing countries has been estimated at US$ 30 - $ 40 per capita, but the current level of
public funding from the Ugandan government for health services per capita is only about
US$ 8 (Uganda Ministry of Health 2005). Furthermore, the World Bank made new loans for the
support of health facilities conditional on the introduction of a national health system based
on user-charges. However, the opposite happened and user fees got abolished. Today, the
health sector and the water sector have been identified as key sectors under the 2004 Poverty
Eradication Action Plan (PEAP), Uganda's main strategy to fight poverty (Republic of Uganda
2.3 The Ugandan water and sanitation sector
The water and sanitation sector is the second most important sector (after the health sector)
for the prevention, mitigation, and control of diarrhoeal infections and therefore plays also a
vital role when it comes to the prevention of disease burdens. Uganda's water and sanitation
sector is defined by a variety of different agents (similar to the health sector) that provide the
following services: clean water for domestic use, water for agricultural use, mobilisation and
training for community management and awareness, and sanitation and hygienic services
(DANIDA 2009). To improve its effectiveness and coverage the sector was reformed through
several laws in 1995, leading to decentralisation and increased private partnership (UN-Water
2006). The lead agency for most concerns related to water and sanitation is the Ministry of
Lands, Water and Environment, respectively, its Directorate of Water Development (DWD).
It provides regulations and policies, coordination, support, capacity building, and some
implementations that cannot be handled by the local governments such as town piped water
supply. The Directorate of Water Development is supported in its role by the semi-private
National Water and Sewerage Corporation (NWSC) that implements and manages the piped
water supply in sub-urban and urban areas (DANIDA 2009). Also, the Environmental Health
Division (EHD) controlled by the Ministry of Health is in charge of an integrated and
national sanitation strategy (Uganda Ministry of Health 2005).
Overall, Uganda has a relatively well-developed framework of national sanitation
policies. Laws and regulations have been created or revised to support these policies, a
process that is still incomplete but currently continuing. For example, the new constitution
established in 1996 states that every Ugandan has the right to a clean and healthy
environment, including drinking water (IRC 2009).
The legislative arm of the national water and sanitation policies is the Ministry of
Lands, Water and Environment, and the executive arm is the Directorate of Water
Development which also supports the local governments and other service providers (DWD
2009). The current legislative water sector framework, implemented through the 1995 Water
Statute, has the objectives to promote rational water use and management, to provide clean,
safe, and sufficient domestic water supply to all people, to develop water and its use for other
purpose like e.g. irrigation and industrial use, and to control pollution and the safe storage,
treatment, discharge, and disposal of waste that may cause water pollution or other threads to
the environment and human health (Republic of Uganda 1995). The management of the water
sector is controlled by following policies:
- The sector policy and legal framework includes the Constitution of the Republic of
- The Local Government Act (1997), Uganda Water Action Plan (1995). - The National Water Policy (1999), Water Statute (1995). - The Water Resources Regulations (1998). - The Water Supply Regulations (1999). - The Water (Waste Discharge) Regulations (1998). - The Sewerage Regulations (1999). Others include: The Environment Management
- Land Act (1998), National Health Policy and Health Sector Strategic Plan (1999). - The National Gender Policy (1997).
(DWD 2009) The National Water Policy (1999) is especially important, as it promotes the principals of
integrated water management and water supply. It also recognises the economic value of
water and supports the participation of all stakeholders in all stages of water supply and
sanitation (DWD 2009). There have also been several efforts to develop an official national
sanitation policy, the latest being the draft National Environmental Health Policy for Uganda.
These policies take into account the needs of different population groups in urban centres,
small towns, rural growth centres and rural communities, and have led to the preparation of
development approaches and technical guidelines that have been adjusted to the social and
economic conditions of the user communities (IRC 2009). Therefore, the policies stated above
together with the health policies create a well connected legal framework which should
decrease diarrhoeal infections as well as its burden, if implemented effectively.
2.4 NGOs and other organisations involved in health and sanitation practise
To some extent the essential follow-on activities and interventions are occurring primarily
through donor-funded programmes for health, water supply, and sanitation. The emphasis,
however, tends to be on sanitation and water supply projects, though funding allocations tend
to favour urban over rural areas. Sanitation is not considered to be a separate programme
area, either in funding or project development terms. Moreover, individual households,
where sanitation needs are greatest, generally receive no material support for the construction
or maintenance of latrines (IRC 2009). Promotional and technical guidance for sanitation is
available at the household level, but even these means of assistance are inadequate to meet
the need (IRC 2009). To overcome this issue several international and non-governmental
organisations are active in Uganda's health and water sectors. Out of these NGO activities
emerged the Uganda Water and Sanitation Network (UWASNET) that functions as a NGO
umbrella organisation providing coordination and capacity building support. Major
contributors and donors are the development corporations of Denmark, Sweden, Germany,
Austria, Great Britain, and the European Union. Especially DANIDA and DED/GTZ/KFW
are very active in the water and sanitation sector. As well as the NGOs African Medical and
Research Foundation (AMREF), WaterAid, the Water & Sanitation Resource Centre
(WATSAN), and the International Centre for Diarrhoeal Disease Research, that all have a
special focus on the prevention and treatment of diarrhoeal diseases. Major joint-
interventions are the National Sanitation Working Group, the National Sanitation Week, the
National Hand-Washing Campaign, and the Water and Sanitation Sector-Working Group
(WSSWG). All of these interventions aim at increasing the participation between the
different stakeholders, at increasing safe water supply and adequate sewage disposal, and at
preventing water-borne and water-related diseases such as diarrhoeal infections (DANIDA
2.5 Conclusion
As outlined, Uganda has developed a structured framework of policies aimed at fighting
diarrhoeal diseases and is still in the process of doing so. The information about the different
sectors and agents involved in Uganda's health, water, and sanitation sectors are an important
base for the study's economic analysis, as most costs created through ill-health are suspected
to emerge from the health sector and to a small extent from the water sector. Especially the
National Health Policy (1999) will be of advantage to the people as it aims at preventing
diarrhoeal diseases as well as its burden through the abolishment of user fees. The water and
sanitation sector also created a range of different laws aiming mostly at the safe supply of
water and at the safe discharge of sewage, which is essential for the prevention of diseases
and ill-health. Additionally, a lot of NGOs are active in this field, and sanitation interventions
seem to become more frequent and effective. However, in terms of policy, there still seems to
be a lack with regards to cost-recovery. Some patients need to consult private health facilities
if they are nearer by, or require additional treatment that cannot be provided by the public
health sector, which creates extra cost. Also, medication and drugs are not always provided
for free under the National Health Policy (1999), and there is no system to compensate for
lost productive labour time such as a national health insurance, though the Ugandan
government is aware of the issue and plans for a national insurance scheme are going ahead.
In any way, the research conducted through this study can help to further adjust the policy
framework and to give further recommendations for policy building.
3. Theoretical Framework
3.1 Introduction
The present chapter further introduces the relations of infectious diseases, ill-health, and the
economy, and also highlights the health economic theories relevant for this study. First of all,
health economic literature and theories will be described in section 3.2 in order to understand
the major coherences between ill-health and the economy. Secondly, to understand how
people mitigate and cope with the burden of ill-health, household livelihoods and the
meaning of risk-economies and coping strategies will be discussed in section 3.3. Thirdly, as
poverty is a status which is suspected to be closely related to ill-health, the concept of the
medical poverty trap will be explored in section 3.4. On the basis of the reviewed literature
and of the introduced theory, the researcher's rationale for studying the micro-economic
impact of diarrhoeal infections on households will by explained. Lastly, section 3.6
highlights the study's research question and sub-questions. The chapter conclusions are
drawn in section 3.7.
3.2 Health economics concerning the economic impact of diseases
"Much present morbidity is unnecessary, much mortality premature. Better health is within
our grasp if only we choose to pay its price."
(Weisbrod 1961)
Theoretical approaches concerning the micro- and macroeconomic assessment of infectious
diseases have been applied since the first cholera epidemics in Europe during the 19th
century. And the English economist Alfred Marshall analysed already in the early 20th
century the rational and irrational motives that led individuals, families, and employers to
invest in human capitals, of which health is one of them. He used this knowledge for
analysing patterns of labour supply and household incomes and his theories still influence
health economics (Agich et al. 1986).
Knowledge and data regarding the economic impact of infectious diseases is becoming
again very important due to recent poverty reduction efforts, due to the rising demand in new
health insurance schemes in developing nations, and due to rising incidence of infectious
diseases caused by global warming. In setting priorities among control efforts across many
different types of diseases, it is essential for development and health authorities to measure
the welfare, capital, and asset loss inflicted upon a population by a given disease (Philipson,
1999). Moreover, information on the economic impact of infectious diseases is needed to
target interventions efficiently and to justify further investments in disease research,
mitigation, and control. Policy makers and planners need exact numbers and statistics of e.g.
disease incidents and their financial impacts to justify e.g. sanitary interventions (Chima et al.,
2003). Such economic health information are also of importance for cost-effectiveness
analysis e.g. in the water and sanitation or development policy sector, and as argued by the
WHO (2002), data about economic costs and effects of disease prevention and intervention
programs as well as about the economic impact of water-related diseases remain critically
important (WHO, 2002; Hutton et al., 2004). Also, microeconomic health data concerning the
extent of diseases is necessary to assess health sector reforms as e.g. the current trend of
privatisation going on most African countries (McIntyre et al., 2006). If medical expenses are
becoming less subsidised, public spending will obviously rise and private savings will
decline, making the household more vulnerable to impoverishment.
Breyer et al. (2005) argue that health is the most important precondition for economic
development, because ill-health decreases and impedes individual and commercial
productivity enormously. Therefore, it is important to analyse what kind of commodities and
assets someone is willing to trade-off in exchange for well being and good health; and also,
to analyse what kind of commodities and assets someone is willing to trade-off in exchange
for the re-establishment of a good health status in the case of ill-health (Breyer et al. 2005).
According to the Grossman model, which argues that health is an integral part of the human
capital, health and capital are both inter-connected assets and the values and optimums of
both are controlled over time by the individual. Therefore, increasing costs for health
services and products also increase the necessary level of investments in the total health
capital, respectively, decrease the total health capital. However, with the progress of the
individual aging process, the level of amortization will increase, and the investment in a good
health status becomes less profitable. Also, a good health status or the total health capital is
influenced by happenstance and is therefore not super imposable and tradable. Moreover, in
the case of less affluent individuals or households, the health status correlates negatively with
the demand of health services, as individuals impacted by ill-health can't afford the necessary
services to restore their health status (Grossman 1972).
However, for developing, infrastructure, and health authorities to be able to finance and
subsidise medical expenses, respectively to prevent them so that they cannot cause economic
impacts at the household level, they rely on data about what micro and macroeconomic
damage ill-health and diseases can cause. Without this data, economists are not able to carry
out cost-effectiveness and cost-benefit analyses to evaluate demand for health services,
health interventions, or expenditures for health care. The cost-effectiveness analysis (CEA) is
an economic analysis that compares the relative expenditures and outcomes (effects) of two
or more courses of action. Cost-effectiveness analysis is often used where a full cost-benefit
analysis is inappropriate e.g. when the problem is to determine how best to comply with a
legal requirement. This analysis is also often used to analyse the "cost-effectiveness" of
health interventions, or disease prevention strategies (Murray et al. 2000). Cost-benefit
analysis (CBA) is mainly used to assess the value for money of very large private and public
sector projects like e.g. the installation of water and sanitation facilities. This is because such
projects tend to include costs and benefits that are less amenable to being expressed in
financial or monetary terms (e.g. environmental damage) (Folland et al. 2007). In health
decision making, such as in bio-medical and disease research, the cost is often replaced by
risk, and the cost-benefit analysis is turned into a risk-benefit analysis.
According to various sources, the household-level and its microeconomic relations are
the preferred unit of analysis for assessing the cost of diseases and illness, by including
indirect and direct incomes and expenditures of the targeted households (Russell, 2004). An
analysis from the microeconomic perspective is important in this study as microeconomics
focus on how individuals and households make decisions to allocate limited resources. Also,
microeconomics considers issues as how households reach decisions about consumption and
savings (The Economist 2008).
3.3 Livelihoods and risk-economics at the household level
Inadequate access to health care is a major health and development issue, which is closely
linked to people's livelihoods and their ability to generate livelihood assets such as e.g.
human or financial capital. Moreover, economic coping strategies at the household level,
respectively household risk-economics, are largely shaped by the availability and
diversification of livelihood assets (Obrist et al. 2007).
This declaration is especially true, when seen through the livelihood approach, which
emphasises people's need to a diverse mix of assets including material and social resources.
Livelihood assets include human and social capital, natural capital, physical capital, and
financial capital. And people's health seeking behaviour, e.g. whether a sick person consults
a pharmacy, a traditional healer, or a professional doctor first, depends largely on the
household's ability to access livelihood assets of the household and the wider society (Obrist
et al. 2007). Basically, people's livelihoods determine their ability to cope with economic and
health shocks. Therefore, the access to livelihood assets is a key issue for sustainable
livelihoods. However, many people have difficulty in accessing household and community
assets, which often constrains their ability to cope with diseases.
As every household needs to apply a set of coping strategies and risk-economics when
impacted by ill-health, regardless of whether it is rich or poor, the analysis of household's
risk-economics and vulnerability is a key feature of livelihoods and of the understanding of
poverty (Devereux 2001). For example, diarrhoeal diseases are a major risk factor for
households and for people's livelihoods in Sub-Saharan Africa, as they can result in a decline
of productivity and financial equity. And according to Christiaensen et al. (2005) infectious
diseases are one of the major determinants for household vulnerability in non-arid areas in
Eastern Africa such as in Uganda.
To mitigate such a risk, individuals or entire villages can, for example, join a
community based health insurance as part of their strategy to mitigate risk from disease
(Wiesmann et al. 2000). To protect the livelihood assets necessary for such insurances,
government and development agencies could, through public interventions, enhance
livelihood-protection functions such as e.g. fertilisers and seed subsidies (Devereux 2001).
Another form of risk-economics and of decreasing household's vulnerability is to diversify
the household income. This strategy is often preferred by households which want to
smoothen their income ex ante a household economic crisis, as the household would be very
unlikely be able to smoothen its income and consumption ex post (Christiaensen et al. 2005).
Informal insurances and self-insurance through household assets would also be an alternative
method of risk-economics as compared to private commercial insurances which are almost
nonexistent in Sub-Saharan Africa anyway. Unfortunately, most households are constrained
to adapt this strategy, probably because access to assets is often limited and asset markets are
poorly functioning during and after a crisis (Dercon 2002).
However, risk-management should be distinguished from coping strategies. According
to Dercon (2002), risk-management strategies attempt to decrease the risk upon income
processes ex ante, therefore, risk-management is income smoothing. In contrast to coping
strategies, which deal with consequences of income risk ex post and are therefore
consumption smoothing (Dercon 2002).
For example, households which cannot afford medical treatment costs because they are poor
and lack any form of insurance, are often avoiding medical treatment completely or substitute
for low quality medical treatment. But even if both of these coping strategies reduce the
financial burden caused by ill-health, they are not ideal, and may even enlarge the issue
(Prescott 1999).
The most common coping strategies applied by households impacted by ill-health and
disease in Sub-Saharan Africa are: intra- and inter-household labour substitutions,
engagement in labour activities other than normal work, financial borrowing from formal and
informal sources, use of savings, change of consumption patterns, and the sale of assets
(Chima et al. 2002, Lucas et al. 1999). Other structural factors which help households to cope
with consumption shocks can include a high level of adult literacy, accessibility of the
markets with regard to livelihood assets, and even the availability of electricity (Christiaensen
et al. 2005). Usually, coping strategies are defined as strategies adopted by family and
household members to minimise the impacts of ill-health on the welfare of all concerned
(Chima et al. 2002). Still, all these measures of crisis prevention, compensation and
substitution strongly rely on people's livelihoods and on the availability of livelihood assets.
It is usually not a question about whether assets are lost trough ill-health, but about the
amount and the value of the assets and about how fast they can get replaced.
3.4 The medical poverty trap
The insecurity of livelihoods and of the access to livelihood assets is also part of a poverty
circle which is driven, among other things, by ill-health and disease. However, livelihood
insecurity is not only a symptom of poverty and ill-health; it is a contributory cause
(Devereux 2001). This phenomenon has been already explained in Whitehead's et al. (2001)
definition about the medical poverty trap, which argues that ill-health may lead to poverty
and poverty may lead to ill-health. The medical poverty trap theory also focuses on
households and their micro-economy to analyse the economic impacts of diseases and ill-
health, and how these factors lead to poverty. Household expenditures created by ill-health
negatively affect household productions and earnings, investment and consumption patterns,
and household health and consumption, and finally can lead to poverty. Basically, being poor
often leads to ill-health, and in turn, ill-health and activities to prevent it also lead to reduced
income capacities (Nelson 1994). Nelson (1994) referred to this ongoing cycle under the term
"drift hypothesis", as ill-health can cause a downward drift in the socioeconomic status. This
assumption deeply correlates with the arguments put forward by Breyer et al. (2005).
Moreover, the consequences of ill-health on a household and its activities and survival
strategies can be quite complex, and affects most social and economic actions of a household
(Feachem et al. 1992).
Lwanga-Ntale et al. (2003) also highlight, that chronic poverty among individuals and
households, is often a consequence of poor health and poor health care systems.
Ill-health leads to the spending of household savings, to the sale of household assets such as
e.g. land and livestock, and to the decline of the household's labour power (Lwanga-Ntale et
al. 2003). Poor households affected by ill-health often need to apply strategies to survive this
difficult period and to cope with the economic burden caused by actions to improve the
health status. Sauerborn et al. (1996) analysed risk-management and coping strategies
applied by households in Sub-Saharan Africa. They found out that most poor households rely
on a mix of following economic strategies when affected by ill-health: intra-household
(labour) substitution, mobilisation of finances and household savings, sale of assets
(livestock), income diversification, and receiving loans and gifts from relatives and friends.
These coping strategies secure the economic survival and vitality of the household, but only
for a limited timeframe. If applied over a long period of time, coping strategies related to
severe and long-time ill-health would harm the microeconomic structure of a household, and
they would lead to household impoverishment (Sauerborn et al. 1996).
To overcome this cycle of ill-health and poverty, development interventions should
tackle household's vulnerability to ill-health and diseases as well as the reduction of poverty.
As poverty correlates with a lack of livelihood assets, any development intervention which
increases access to natural, social, and financial assets will indirectly support livelihood
security, and therefore break this cycle (Devereux 2001). The reduction of official and
unofficial costs and fees for health services, measures against corruption within the health
system, a less constricted access to health services, and a better management of public
finances could also be solutions to stop the medical poverty trap (Whitehead et al. 2001).
However, one of the aspects of the medical poverty trap which has been often
overlooked is the fact that people often cannot even get access to health services because
they are simply to poor or hardly own any livelihood assets. This issue should be taken into
consideration, as it is not uncommon for people to dispense medical treatment because of
their socioeconomic status (Obrist et al. 2007).
3.5 Rationale for the attention to the economic impact of diseases
There is a diverse range of reasons justifying increased research in relations between
development, economics, households, and ill-health caused by infectious diseases. Infectious
diseases are currently the major cause of mortality world wide and they already have a
significant impact on macro- and microeconomic structures (Philipson 1999). Furthermore, a
high level of good health and wellbeing among the average population is also a precondition
for any development activities. As already outlined, poor health and the prevalence of
infectious diseases slow down the productivity of individuals and of the community and the
wider society, and therefore can severely damage asset generating structures. Many
households especially in Sub-Saharan Africa are forced into persistent poverty because they
cannot cope anymore with the social, physical, and financial burdens of ill-health. Only if we
find out more about exactly how diseases impact households and their micro-economies, and
what kind of damage they cause (apart from physiological damage), will we be able to
efficiently create measures to alleviate the impact of ill-health and disease.
The evaluation of ill-health from an economic point of view is particularly important,
as economic analysis divides the health effects of public policies from those of private
decision making (Philipson 1999). With regards to Uganda's policy framework, more specific
data about the impact of diseases is needed as well to adjust current policies and to build new
ones. Also, in setting priorities among control and prevention measures among many
different types of diseases and health threats, public health authorities must find out more
about the direct welfare loss inflicted upon a population by a given disease or threat
(Philipson 1999). Moreover, such data are of critical importance for agencies and authorities to
further justify investments in disease specific research. Unfortunately, only if the economic
burden is significant enough, will funding for health research be made available (Chima et al
2003). The evaluation and the assessment of health sector reforms such as e.g. the ongoing
trend of privatisation in African countries, as well as the carrying out of cost-effectiveness
and cost-benefit analysis especially in the water and sanitation sector is very difficult without
knowing the exact effects of ill-health on welfare (McIntyre et al. 2006). And the newly
emerging market of public and private health insurance schemes in Sub-Saharan Africa is
strongly relying on such data too. The insurance companies will most likely be unable to run
their business, nor be able to calculate revenues and premiums if they are not able to pre-
calculate and estimate future spending on disease specific medical treatments.
Awareness of the economic impact of infectious diseases, and especially about
diarrhoeal diseases, is recently brought into focus by ongoing poverty reduction efforts.
Development and health authorities are becoming more and more aware of the whole impact
diseases can cause, and are increasingly looking for strategies to eradicate, or at least to
reduce, them. This will not be easy, as it is predicted by the Intergovernmental Panel on
Climate Change (2007) that the prevalence and incidence of infectious diseases will
dramatically rise and especially food-borne and water-borne diseases are expected to occur
more often in future.
3.6 Research question and sub-questions
The introduction and the theoretical background have outlined the importance of this subject,
as they highlight the relation between ill-health and poverty and therefore justify the need for
further and improved research in this field. With regard to previous studies, children, rural,
and poor people are most affected by diarrhoeal infections and their consequences.
Therefore, it will be necessary to focus on the economic burden caused at the individual and
household level, to get an improved understanding of the microeconomic impacts.
This study intends to understand how the victims and affected households subsidise or
cope with the financial and overall economic impacts inflicted by infections causing
symptoms of diarrhoea, and whether these coping and risk reducing strategies lead to further
impoverishment. To analyse the total microeconomic burden, the impact of health seeking
behaviour, the impact of prevention methods and expenses on household assets and savings,
as well as on the loss of the victim's and their family's labour time must be measured too.
Furthermore and according to the Uganda Demographic and Health Survey 2006, some
people, especially in rural areas in Uganda, seem to prefer medical treatment based on
traditional and herbal medicine instead of medical treatment based on scientific medicine.
This probably has an affect on the financial expenses for medical treatment expenditure.
Though, this practise is more common in Southern and Northern Uganda. Also, a sick person
does not always seek the attention of a doctor, but often applies some kind of self-treatment.
It would also be very interesting to find out, if there are any associations between the
households (financial) wealth, the rate of infections, and the efforts of households to prevent
diseases and diarrhoeal infections. Moreover, what are the differences between the rural and
sub-urban medical seeking behaviours, and what could be the reasons?
For these reasons, the following research question and sub-questions have been formulated:
Research question:
What are the financial consequences for households in dealing with diarrhoeal
infections in South-Eastern Uganda?
Sub-questions:
1. What kind of medical treatment (public, private, or traditional) is used and preferred by
the people, with regard to infections causing symptoms of diarrhoea?
2. Are there any differences between rural and sub-urban households in health seeking
behaviours, and in cost burdens caused through ill-health?
3. How do households cope with the financial burden caused through diarrhoeal infections
3.7 Conclusion
We are now able to understand how infectious diseases and ill-health are able to influence
and economically impact individuals and households. As argued, health is an important
precondition for development and also an integral part of the human capital. To be able to
increase people's health status, to protect them from ill-health, and to justify further research
and improvements, it is crucial to assess the economic damage caused by various infectious
diseases. This data is also of importance for medical insurances and other health agencies to
be able to carry out cost-effectiveness and cost-benefit analysis. As justified, it is the
household-level and its micro-economic relations that is the preferred focus of assessing the
cost of disease and ill-health.
Poor households suffer more than averagely from the consequences of ill-health and
therefore constantly need to apply risk-economics and coping strategies to mitigate and
decrease the burden of ill-health. Common coping strategies include for example: intra- and
inter-household labour substitutions, financial borrowing from various sources, and the sale
of valuable assets.
The researcher also introduced the concept of the medical poverty trap, which argues
that ill-health leads to poverty and that poverty leads to ill-health. This theory explains why
chronic poverty among individuals and households is often a consequence of a poor health
status and poor health services. To overcome this cycle of ill-health and poverty,
development interventions should tackle a household's vulnerability to ill-health and to
poverty. As this study intends to understand the micro-economic impacts caused by
diarrhoeal infections on households in Uganda, the following research question has been
outlined: how do diarrhoeal infections economically impact rural and suburban households in
Uganda? The researcher also formulated three sub-questions to further investigate any
differences between suburban and rural locations, and in the health seeking behaviour.
4. Methodology
4.1 Introduction
The present chapter presents and describes the study's methodological techniques. First of
all, the study's epistemology will be described in order to understand the philosophical
background the study is based on in section 4.2. Secondly, the study's conceptual framework
will be outlined in section 4.3, followed by the description of the operationalisation of the
concepts, which will be discussed in section 4.4. Thirdly, to appoint the focus of this study,
the target population will be explored in section 4.5; and in order to make it possible to
determine the sample units, the selection of the sample size will be explained in section 4.6.
Section 4.7 outlines the sampling methods, variables, and indicators which are necessary to
collect the relevant data in order to answer the research question. Subsequently, section 4.8
describes the process of analysing and processing the collected data, before moving on to the
ethnical considerations described in section 4.9. The chapter conclusions are drawn in section
4.2 Epistemology
The research is largely based on the philosophical and epistemological stances of
objectivism, justified by the economic and epidemiological concepts used within this study,
which are both mostly of a quantitative nature. "Objectivistic research supports the view that
things exist as significant entities independently of consciousness and experience, that they
have truth and meaning residing in them as objectives, and that scientific research can reach
this objective truth and meanings" (Crotty 1998, p. 5).
The theoretical perspective is mainly based on positivism. Even if some of the collected
data are of qualitative nature, most of the findings are quantitative data and indicators.
However, as some of the methodological indicators such as e.g. indirect costs related to ill-
health and social aspects can only be measured indirectly, they have become a subject of
interpretivism. For example, some information collected through methods such as interviews
and observations are not always as clear to interpret as e.g. quantitative data. Its
interpretation is therefore more theoretical and findings can be very relative with regard to
people's different views and perspectives. Moreover, due to the lack of knowledge (before
the process of data collection) about the significance of some of my anticipated
methodological indicators, and due to the need to consider socio-economic aspects, the
researcher needed to include some aspects of subjectivism into his epistemology, supported
by the theoretical perspective of phenomenology. In comparison with natural scientists, it is
often more difficult for social scientists (including economists) to prove something exactly
and phenomena are rarely verified exactly. With regard to the epistemological framework of
the study, the process of data collection is predominantly shaped by a household survey, and
as already justified, to a smaller extent by phenomenological research techniques such as
informal interviews and observations. Furthermore, the study has been approached with
quantitative measures like health economic models and theory and has been analysed in such
4.3 Conceptual scheme
Figure 4.1 Flow-chart of the conceptual framework for analysing the economic burden of
infectious diseases on the microeconomic and household level
4.4 Definition and operationalisation of concepts
4.4.1 Diarrhoeal infection
Diarrhoeal diseases lead to symptoms of gastrointestinal infection, which can be caused by a
variety of bacterial (e.g. cholera), viral (e.g. rotavirus) and parasitic (e.g. schistosomiasis)
organisms. Infection is spread through contaminated food or drinking-water, or from person
to person as a result of poor hygiene (WHO 2008).
Though, many diseases can cause symptoms of diarrhoea, this study will concentrate on
victims and patients affected by the major classified water-borne and water-related pathogens
causing diarrhoeal infections. These are, according to the WHO, Vibrio cholerae, Giardiasis
intestinalis, Escherichia coli, Salmonella typhi and Entamoeba histolica.
Unfortunately, due to a high proportion of households and their victims suffering from
symptoms of diarrhoea which are not professionally diagnosed, the definition of the term
diarrhoeal disease has been difficult to operationalise, and has therefore been changed to the
definition of diarrhoeal infection instead which describes any infection causing symptoms of
diarrhoea. Due to this operational issue, the study therefore concentrated on all diarrhoeal
infections reported by the household members.
Usually, professional laboratory tests for the correct determination of the pathogen have only
been applied in acute and severe cases, due to a lack of finance and equipment. Therefore,
the researcher did consider all people reporting severe, long-lasting, or chronic watery,
bloody or rice stool as victims of a diarrhoeal infection. This is the same procedure most
local physicians follow. Infections with hookworms were easier to diagnose as this parasitic
pathogen can be seen with the human eye.
4.4.2 Household
A household in this study was defined and characterised as an individual, or group of persons
who, on average, occupy a common dwelling (or part of it). They provide themselves jointly
with food and other essentials for living. Basically, they live together and share their
resources as a unit. Other explanations can be related to the phrases "eating from the same
pot" and "cook and eat together". The researcher decided also for this definition as this is the
most convenient way to observe a household within a household survey in Sub-Saharan
Africa (Statistics South Africa 2005). The household units surveyed for this study included also
family members, who may work or live most of the time away from the household, but who
are significantly contributing e.g. financially to the household spending and savings, and who
also have a close family connection to at least one permanent household member. For
example, a husband or close relative who is working and living at a distant location, but who
is sending money home to its family or household. Some information about the household
structure and its members are important for this study, as for example the number of children
and adults, and the number of employed household members within one household have an
influence on the medical treatment behaviour and on the economic burden.
The researcher's rationale for the decision to observe and analyse households and their
household members as a whole unit was based on experiences collected in similar household
studies and surveys conducted in Sub-Saharan Africa (Statistics South Africa 2000 & Sahn et al.
2000). Similar methods used to calculate the incomes and expenditures of households in Sub-
Saharan Africa and elsewhere like e.g. the social accounting matrix (SAM) take the
household as a unit as well (Statistics South Africa 2000). Moreover, and with regard to the
research question, the major aim of this project is to analyse the financial impact inflicted
upon the whole household unit and not upon individuals within the household as this would
deviate from the main focus. All of the household asset indexes used in the analysis have
been measured on a per household basis. The implicit reason for doing so is that financial
economies and economies of scale of the assets within households are infinite if all possible
aspects are taken into consideration (Sahn et al. 2000). Again, the analysis of individuals
within a household unit would require a complex analysis about intra-household and social
differences first, which is beyond the scope of this study.
However, the researcher recognises the fact that there are maybe intra-household
differences such as e.g. gender or age inequalities within a household unit, which could be
related to unequal access to health care and to unequal spending for individual's health and
well-being. For example, Moss (2002) highlights that the household is the most intimate
location for the abuse of power, authority, and control, and women are often affected in a
number of ways. Often, male partners and in-laws control women's access to money, food,
and health services (Moss 2002). And Osmani and Sen (2003) even argue that women's
exclusion in terms of proper nutrition and healthcare rebounds on the whole society in the
form of their children's ill-health. One example is the fact that malnutrition of the mother can
affect the development of their foetus (Osmani et al. 2003). However, they realise as well that
this phenomena is deeply influenced by geographical location, culture and by religion. The
described phenomenon is far less a problem in Sub-Saharan Africa than for example in South
Asia, North Africa, and the Middle East, where women are primarily excluded from their
rights. Several studies indicated that, based on anthropometric indicators, intra-household
gender inequality is sometimes less of an issue in Sub-Saharan Africa as compared to
inequalities based on age (Haddad et al. 1993. & Sauerborn et al. 1996 & Garg et al. 1998). The
underlying reason for this issue is that the household's income spent for healthcare is usually
concentrated on productive members instead of spreading it between all indigent household
members (Sauerborn et al. 1996). As women usually are contributing much more work to the
household as men it would be irrational to not invest in their health. Mainly, children below
the age of five years are more excluded from modern health services (Sauerborn et al. 1996),
and ill-health is usually associated with higher expenses for medical care when adult
household members are involved (Su et al. 2006). In addition, there are 2.6 % more women
than men in Uganda, 25% of all households are headed by women (Uganda Bureau of Statistics
2006b), and the life expectancy of women in Uganda is 53.4 years, higher than male life
expectancy (51.3 years) (CIA factbook 2008). Also, the number of unattended birth deliveries
is decreasing and maternal health care is increasing (43% of all pregnant women in Uganda
were treated with SP/Fansidar® to protect them against an infection with malaria during
pregnancy) (Uganda Bureau of Statistics 2006b).
Women usually receive more disadvantages in education as they are often referred to as
cheap labour, but this issue is not the focus of this study. As already justified, this study
concentrates only on the monetary and financial impacts created through costs for health
services for the household in whole, and individual inequalities are less of a concern, and
would require an intra-household analysis.
4.4.3 Poverty
"Poverty: a human condition characterized by the sustained or chronic deprivation of the
resources, capabilities, choices, security and power necessary for the enjoyment of an
adequate standard of living and other civil, cultural, economic, political and social rights."
(Source: UNHCHR 2002)
This research focuses mainly on poverty in economic and financial terms, while also
considering social aspects of poverty such as e.g. the number of family members.
The poverty of e.g. human rights, political stability, or other "poor considered processes"
which are not directly related to ill-health will not be included in this study.
As poverty is a very relative explanation and is differently experienced in other
cultures, local (Ugandan) perceptions of poverty will be respected and taken into
consideration. In other studies about Uganda, poverty is defined by the poor themselves as: A
persistent situation like "rain that soaks the poor and does not stop" in which "one survives
marginally", with "problems that follow you", "living hand-to-mouth" and in "perpetual
need" "due to lack of the basic necessities" of life and the "means of production", lack of
social support; and feelings of negativity, frustration, and "powerless" to "influence the
things around one" because "one has no source of life" (Lwanga-Ntale et al. 2003).
4.4.4 Microeconomics
Microeconomics is the part of economics that studies how individuals and households make
decisions to allocate limited resources. Also, microeconomic considers issues such as
households reach decisions about consumption and savings (The Economist 2008).
4.4.5 Assets
Assets are defined as any items of economic value owned by an individual, household, or
business, especially that which could be converted into cash. Examples are cash, securities,
accounts receivable, inventory, real estate and land, a car and other property. On a balance
sheet, assets are equal to the sum of liabilities, common stock, preferred stock, and retained
earnings (InvestorWords 2008).
4.4.6 Direct costs
Any (visible monetary) cost, that can be directly attributed and related to the purchase of a
certain product or service, or respectively, to the loss of values and assets.
4.4.7 Indirect costs
Indirect costs are the opposite of direct costs. Indirect costs are usually not obvious and are
often hidden or not visible. Also, they are often related to direct costs or results from them.
Basically, indirect costs are expenses which are not directly attributable to a product or
4.4.8 Medical treatment costs
Any financial expenses and costs at the microeconomic and household level attributed to
traditional and scientific medicine treatment. Including, direct costs for hospitalisation,
medication, and for transportation to the doctor or the hospital.
4.4.9 Coping strategies
Coping strategies can be defined as actions that aim to manage and subsidise the costs and
impacts of an event or process (e.g. ill-health) that threatens the welfare of one or more
members of the household. Basically, coping strategies are trying to sustain the economic
viability and sustainability of a household (Russell 2004).
Coping strategies in this study are more seen as economic instruments to analyse the
economic survival of a household. Basically, all actions the household members take to
stabilise the economic impacts of a diarrhoeal disease. An example would be, to send a
household member away to live with e.g. wealthier relatives to decrease household expenses.
The term "coping strategies" in this study can not be related to the psychological definition
4.4.10 Disease prevention costs
Any financial expenses and costs at the microeconomic and household level attributed to the
prevention, reduction, and interruption of the transmission and infection of disease causing
4.5 Target population
The main target population in this study have been rural and sub-urban households in Uganda
in which members were previously (within the last six month) and/or are currently affected
by infections causing gastrointestinal and gastroenterological symptoms. With regard to the
definition and operationalisation of the term diarrhoeal infection, the households and their
members chosen should have been impacted previously by ill-health caused by infections
with Ancylostoma duodenale, Camplyobacteriosis, Cryptosporidium, Entamoeba histolica,
Escherichia coli, Giardiasis intestinalis, Norovirus (virus type: Caliciviridae), Salmonella
typhi and bacteria, Shingella enteritis, Rotavirus (virus type: Reoviridae) and Vibrio
cholerae.
In addition and by referring to the thesis's sub-section (1.4) about Uganda and its
people, most forms of people's livelihoods located in suburban slums are based on small-
scale businesses, begging, and day labouring; whereas most forms of people's livelihoods
located in rural areas are based on subsistence farming (Uganda Bureau of Statistics 2006b).
Subsequently, the survey conducted within this study concentrated on households and their
members which had the same forms of livelihood just described.
Therefore, the main target population were households which were relatively poor in
financial terms, and households which lack proper access to fresh water and sanitation
facilities. The target population were based in suburban slums and in rural villages and their
forms of livelihood were usually very simple and predominantly based on wage labouring
and subsistence farming.
This particular target population has been chosen, because the described households and their
members are most vulnerable to infections with diarrhoeal diseases and to the burden of
diseases due to their limited access to proper sanitation and health care facilities.
The second target population in this study, though much smaller in size, consisted of
health workers and physicians working for either private or public health facilities.
Respectively, qualified experts in the health sector who deal with diarrhoeal infections. This
target population was mainly used for background and reference data and to confirm and
compare findings from the household survey. After the arrangement of an appointment for
interviewing, they were interviewed at their workplace usually in a health facility.
The researcher has chosen this particular target population because their responses were
expected to be more specific, precise, and technical when being interviewed about e.g.
sanitation and water infrastructure, medical treatment and epidemiological data as compared
to the mostly quantitative data gained through the household survey. Also, these people are
experts in their field of profession, and they see issues in a different perspective, usually a
more scientific one.
As more precisely outlined in the following sub-chapter 3.4, expert interviews were
conducted with physicians from Mulago Hospital and Mengo Hospital, and the researcher
interviewed a physician from the Mukwano Consultation Clinic which is a private health
facility based within Katanga slum. In Wakiso district, one interview was held with a public
village health centre, and in Jinja district one interview was held with a missionary health
4.6 Selection of sample size
With regard to the mostly quantitative nature of the study's methodology, households from
three different Ugandan districts have been included in a survey, and in each district,
representatives of between 10 and 40 households have been interviewed. The research has
been conducted in the districts of Wakiso, Kampala, and Jinja. As already outlined in section
3.2, the researcher decided on these particular districts in South-East Uganda as they are
regarded as the most safe and accessible ones according to current information of the German
Ministry of Foreign Affairs. At the time the field research was planned, the German Ministry
of Foreign Affairs was warning travellers, to travel in Uganda not outside Kampala and
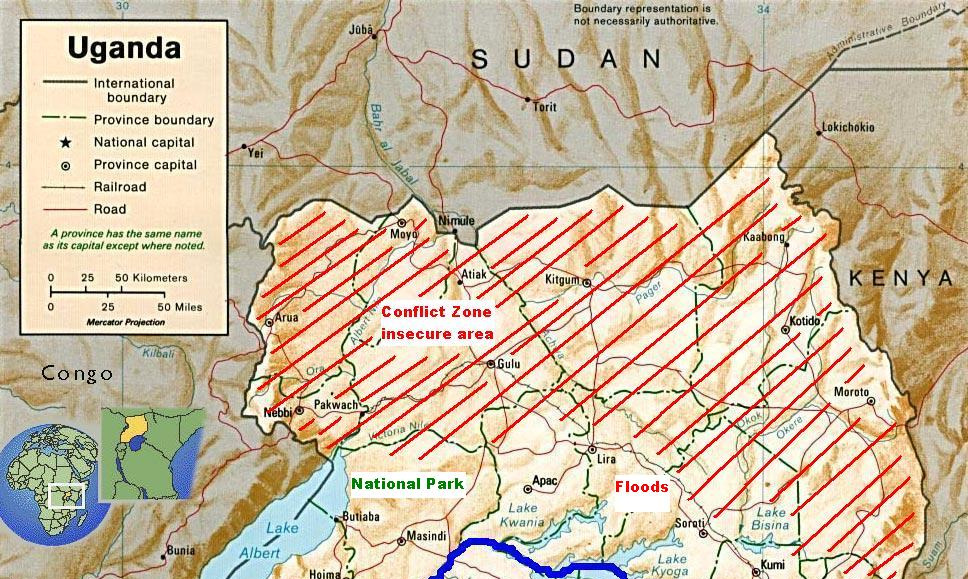
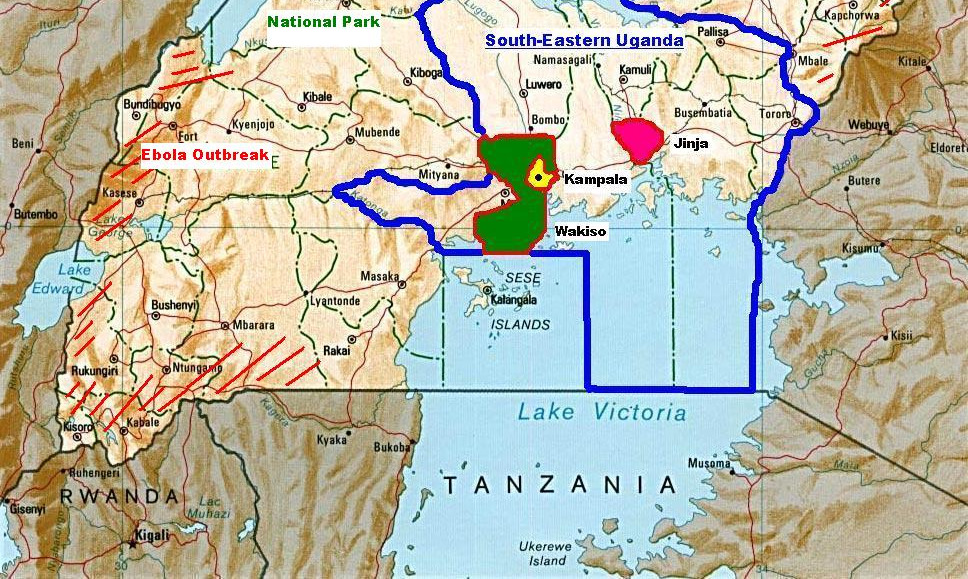
neighbouring districts due to incidents of crime, conflict, and disease outbreaks (e.g. ebola,
cholera, and sleeping sickness) (Auswärtiges-Amt 2008). Also, field research was limited only
to the South-Eastern region because of rebel activities in the Northern region and because of
conflicts along the Congolese, Rwandan, and Kenyan borders, amongst from other security
issues. Another issue were insufficient, bad, or missing modes of transport. It always takes a
long time to reach rural places due to very bad roads and during the rain seasons it is almost
impossible to travel anywhere in the country. As the researcher needed to find rural and
suburban study units with relatively small distances in between, it was finally decided to
conduct the data collection in the districts of Kampala, Wakiso, and Jinja. Kampala district is
mostly dominated by urban settlements and has the most slums, compared to the districts of
Wakiso and Jinja which are more dominated by rural villages and agricultural activities.
The researcher decided also for these districts, as most households and their livelihoods are
dominated by the same livelihood assets and activities which the researcher anticipated to
Figure 4.2 Locations of research areas within Uganda
focus on, with regard to the target population outlined in the previous chapter.
Figure 4.2 outlines the locations of the districts where data sampling took place, including
insecure areas, and areas were research was not possible due to disease outbreaks and other
The researcher and the local supervision of this study were based in Kampala. The local
supervisor was a health economist and physician working for the School of Public Health
which is part of Makerere University and of the Mulago hospital complex (the largest health
facility in the country). Supervision by this particular researcher was chosen, because he has
extensive experience in analysing economic impacts of diseases. To prevent any
misunderstandings, and to increase the quality of the communication during interviews, the
researcher was also, through the contacts of the local supervisor, assisted by an interpreter as
most people in the villages and slums speak their tribal languages. Also, the interpreter is an
academic, and has experience with sampling survey data in slums and rural villages.
During the first consultations with the local supervisor and the interpreter, the
researcher together with the local supervisor and the interpreter decided on the most
appropriate rural and suburban places for collecting the data. Three different slums and
suburban areas in Kampala district, two villages in Wakiso district, and one village in Jinja
district were chosen. To be more reliable and objective, and to make the results more
statistically significant, a number of different communities have been chosen to generalise
the outcome for all the three different districts where the data collection was conducted.
Criteria for the selection of places were suburban and rural settings, sanitary and housing
conditions, people's standard of living, and the prevalence of diarrhoeal infections. The
researcher was committed to find places for data sampling with a high prevalence of
infectious diseases. Accessibility and security of the research area were also included in these
criteria, with regard to advice from the local supervisor and the researcher's interpreter. And
as it was very complicated to find places with victims affected by diarrhoeal symptoms, who
have been professionally diagnosed with one of the infectious pathogens stated above, the
researcher needed to consult local medical experts, and the local slum/village chiefs to find
its anticipated target groups. Another condition was that the selected community has at least
one traditional, one public, and one private health care provider (with regard to the outline of
the Ugandan health sector described above) within the community or near by (not more than
five kilometres away).
As there are many areas and places in the districts Wakiso, Kampala, and Jinja which share
the same distinct conditions and features as described above, the researcher randomly
selected the communities relevant for this study. As mentioned above, the local supervisor
and the interpreter also advised the researcher about areas best to go, but still, the researcher
randomly decided for the research locations relevant for this study. The three sub-urban areas
(slums) finally chosen within Kampala district were Bukesa, Katanga, and Katwe. The two
rural villages chosen within Wakiso district were Lutete and Lwadda. And the village chosen
within Jinja district was Nabulesa.
To be objective and to keep the sample group representative, the researcher interviewed
in total 80 households in suburban and in rural communities. The exact numbers of
interviews per study location are outlined in relation to the population size of the study
location in Table 4.1. In each of the three suburban and of the three rural study locations, the
researcher interviewed between 10 and 15 households, and each interview lasted between 30
Table 4.1 Sample size per study location
Type of study
Study location
Sample size per
Population per
location
study location
study location
Expert information has been gained from various public and private medical facilities
being located in and near the Ugandan capital Kampala and in the surrounding districts. After
consultation with the local supervisor, the researcher approached medical experts, mostly
local physicians, who deal with diarrhoeal diseases and their victims. Due to matters of
accessibility, all expert interviews took place in and around Kampala. After arranging
appointments with them, the researcher usually went to the health facility where the expert is
working and interviewed him or her there. Most of these interviews took place in an office or
directly in the surgery.
Expert interviews were conducted with physicians from Mulago Hospital and Mengo
Hospital, which are Uganda's largest public health facilities based in Kampala close to the
three suburban research locations Bukesa, Katanga, and Katwe. Also, the researcher
interviewed a physician from the Mukwano Consultation Clinic which is a private health
facility based within Katanga slum. In Wakiso district, one interview was held with a public
village health centre, and in Jinja district one interview was held with a missionary health
centre. All experts interviewed were working in health facilities close to the household
survey locations. Therefore, the choices of health experts and facilities interviewed cover all
health sectors available in Uganda, and expert information was gained from all the three
districts visited within the household survey.
These expert interviews were especially helpful with regard to epidemiological and medical
treatment information.
4.7 Sampling methods, variables, and indicators
This study is based on a combination of quantitative and qualitative data collection
techniques. The researcher used for this study a survey and conducted informal and semi-
structured interviews, as well as observations.
A survey at the household level was carried out, usually interviewing the head of
household or the mother by using a questionnaire. The questionnaire was made up of 30
questions with mainly closed questions, but some were created in an open-ended style to
allow more flexible responses (see Appendices).
The questionnaire structured the questions as based on the different indicators and variables
as explained in the conceptual scheme (see Figure 3.1). Addressed were: family and
household structure, occupations and direct / indirect disposable household income, disease
infections, medical treatment behaviour and its costs, special nutrition and its direct cost,
household coping strategies, and disease prevention methods. Questions focused also on data
such as, for example, the costs for medication, hospitalisation, or disease prevention
methods. And they focused on the type of medical treatment (traditional or scientific), and in
the case of the victim's death, the questionnaire also asked for funeral costs. Additionally,
household specific data like e.g. the number and gender of the household members and their
profession were recorded. The concepts used in this study and the indicators and variables
used in the questionnaire survey and their interrelations are similar to the concepts and
indicators used in previous and subject related studies by Chima, R.I. et al. (2003);
Grossman, M. (1972); McIntyre, D. et al. (2006); Russell, S. (2004); Sauerborn, R. et al.
(1996); and Uganda Bureau of Statistics (2006).
The researcher recognises the current debate about how to measure household
economic status as there are different approaches discussed currently. In economic literature
on poverty and well-being, there are three approaches that stand out: the income-based
approach, the expenditure-based approach and the asset-based approach which emerged
mainly out of Amartya Sen's theories about household assets (Morris et al. 2000 & Klasen
2000). Also, a fourth approach focuses on the availability of food and basic needs. This
approach determines where the poverty line should be drawn, by measuring food
consumption, income, expenditures, or asset holdings. Morris et al. (2000) analysed different
indicators used in household surveys and described that out of 14 studies in less developed
countries six where based on the income-based approach (Morris et al. 2000). Most household
and welfare studies conducted in South Africa are also based on the disposable monetary
income available per household unit (Statistics South Africa 2000). Empirical studies of
poverty are usually based on one-dimensional indicators of individual welfare such as
income or expenditures per-capita or per-equivalent adult (Bibi 2005). According to Lloyd et
al. (1993) there is no internationally agreed approach for assessing the relative income of
households that vary in size and structure, therefore the researcher decided to measure the
direct disposable income available for the whole household unit. Also, it is often more simple
to assess the financial income only, instead of measuring the household's consumptions and
expenses. The most conventional technique is to divide the household income by household
size to get an approximate estimate of income per head (Lloyd et al. 1993).
In addition, Milanovic (2002) actually highlights, that it is actually a potential problem that
some surveys measure wealth in income and some in expenditures, as both are recognised
welfare indicators.
Though, this method can only be used to analyse the household unit as the income and
the consumption needs of individuals are usually different and as they can change by e.g.
gender and age. One of the advantages of the income-based approach is that it measures the
whole disposable and monetary income available whereas the expenditure-based approach
can't estimate a household savings (Deaton 2001).
However, the disadvantages of the income-based approach compared to the
expenditure-based approach are that it gives only a short-term impression and fluctuates
more, and consumption smoothing and home produced assets can be less accurately
measured (Klasen 2000). In some cases, consumption smoothing is an important matter due to
national and international price fluctuations, and especially expenses for health care are often
subject to very high price fluctuations. Therefore, expenses for health care should be ideally
measured in a long-term study to be less biased by market and price fluctuations. However,
as the researcher had only a limited time-frame available to collect his field data, this study
had to rely on a cross-section set of data instead of long-term panel survey data.
Nevertheless, imputed values and assets of e.g. home production are only of importance if
they can be turned in monetary assets, as this is the currency mainly used in health facilities.
The study's household survey tried to assess the household's expenses for health care
caused by diarrhoeal infections for the previous six month, and therefore, the household's
monthly average disposable income has also been assessed for the previous six months. The
researcher has chosen this particular time-frame, because incomes generated through, in
particular, the informal sector are often very unreliable and unstable and people therefore
often have difficulties to remember their monthly total amount of income over a longer time
period. In addition, as people often don't keep track of their (health) expenses, it is also
difficult for them to remember expenses for things paid further in the past.
Therefore, the questions in the questionnaire have been formulated with regard to the
concepts mentioned above and mainly focused on indicators and variables such as household
structure, disposable household income, direct and indirect expenses for health care, and
coping strategies. As already mentioned, it is not always easy to measure or answer questions
and indicators in a "yes – no" mode, that is why some questions in the questionnaire have
been open-ended, which made it easier to record all (socio) economic impacts.
According to traditional rules, and due to the fact that most communities in Africa have
a leader or chief, the researcher needed to consult (usually with the help of the interpreter)
the community leader before he was able to take up any research in the designated area. The
process of data sampling was only possible after the community leaders have given their
permission. When the chief or community leader was absent, or when he did not agree with
any data collection activities, the researcher was forced to leave the community and to shift
to a different place where data collection was possible. Therefore, the procedure of
consulting the community leadership was an essential part of the data sampling methods, and
strongly influenced the choices for study locations.
After the identification and consultation of the potential communities and areas for data
sampling mentioned above, households have been purposely approached and interviewed by
applying a non-random sampling method as the rate of disease incidents was generally high
(above average). Also, a random sample was not always possible as not all households were
willing to participate in the survey, and some household communities were absent too.
Non-random sampling is a valuable method for sampling a small number of units impacted
by typical issues, like e.g. diarrhoeal infections. However, one disadvantage of this method is
how to assess how typical the sample really is (Crotty 1998).
The households approached usually consisted of a single house, dwelling, or hut with
the characteristics mentioned in the previous subchapter. The interpreter then asked for the
head of the household or for the mother (the mother of the family is usually responsible for
the care of ill household members) whether he or she was willing to participate in the survey.
In each household, the researcher consulted the head of the household, respectively, the
person who manages most of the household activities in particular related to food, and child
care (which is usually the mother). Due to the fact that most men were busy with work during
day hours, most participants in the household survey were women. Yet, the mother of the
household usually manages most of the household and its economic activities anyway.
The researcher interviewed at leased 10 households in every study location.
The household members were told that participation was on a voluntary basis and that
the collected data would be treated confidentially and would only be used for research
purposes. As it can be difficult to approach and interview somebody suspected to have a
diarrhoeal infection, the researcher and the interpreter needed to be especially sensitive when
collecting the data. In case the reply was positive and after the introduction of the researcher
to the household members, the researcher together with his interpreter, started to interview
the head of the household or the mother. The interview was introduced through a normal not
subject related conversation, and always took place in a confidential and private setting.
Semi-structured interviews and informal conversations have been organised with
experts in this research field as mentioned in the previous sub-chapters. Most experts were
medical doctors treating disease affected patients, as well as officials employed in the health
and sanitation sector. With regard to the research technique of triangulation, the interviews
helped to find out if the study's methodological indicators are significant enough,
respectively, if the impacts described by the experts are similar to the concepts and variables
used by the researcher. Moreover, informal conversations and formal interviews helped to
expose any hidden or indirect disease related economic impacts not covered by the
questionnaire. And the interviews helped the researcher to understand how patients get
treated and what costs are related to the treatment.
Triangulation is used to create checks and balances at different levels of aggregation in data
research to increase the data's variability and credibility.
The set of questions which were asked during these interviews were more professional
compared to the questions in the household survey and to informal interviews, because
experts often see the issue from a different perspective. Also, they were able to give more
detailed information about statistical and numerical data as well as about the costs and
expenses related to the health care system.
Observations were also applied in the areas relevant for research, to get a general
impression about people's livelihoods, about what kind of sanitation and health facilities
were available, and about how people deal with ill-health. This tool was very important, as
the researcher was able to directly observe e.g. how people prepare food, what they eat, or
how the people managed their water supply.
4.8 Data processing and analysis
The data and findings from the questionnaire have been statistically analysed with the help of
the computer programs Microsoft -Excel and Minitab, and then presented in a numerical
context. Numerical tables and charts like frequency/contingency tables and bar charts helped
to analyse and understand the collected data. All the quantitative results from the 80
questionnaires have been first analysed with frequency tables in Excel to get via cross
tabulations a general overview and expression of the outcome, and to measure as well if there
are any associations and correlations between the different categories and variables. If an
association was suspected, a chi-square test has been carried out between the two variables to
prove the association. Furthermore, data assumptions, and relationships and correlations
between variables have been analysed with the regression analysis and with scatter plots
(Mukherjee et al. 1998). To find out if treatment costs, total disease related costs, and
prevention costs are dependent on the direct financial household income; chi-square tests and
regression analysis have been carried out to test the associations and correlations between
treatment costs, total disease related costs, prevention costs, and the direct financial
household income.
To answer the main research question, the total direct and monthly disposable mean
household income has been compared with the total financial mean disease related
expenditures (including and excluding prevention costs). According to Prescott (1999) a cost
burden greater than 10% of the total financial household income will have a catastrophic
impact on the household.
The informal and semi-structured interviews have been transcribed to the relevance,
significance, and objectivity of the content. And the content was analysed according to the
relevant themes. Same as the findings from the formal semi-structured expert interviews,
which have been examined and transcribed in a similar way as the informal interviews, their
results have been set in an (socio)-economic context. The findings from all interviews have
also been used to cross reference the outcomes from the quantitative survey analysis and
from observations.
After analysing the various forms of data, the results have been used to answer the
research question and sub-questions, and have also been compared to previous research
completed by the Ugandan Bureau of Statistics (2006), and to the "medical poverty trap
theory" and the other theories used in the theoretical base of this study.
4.9 Ethical considerations
To protect human rights, and to comply with the ethical and scientific regulation in Uganda,
a research proposal summarising this study has been submitted to the ethical committee at the
Uganda National Council of Science and Technology (UNCST). This is a normal
administrational procedure to formally register as an academic researcher in Uganda and to
get the necessary legal and ethical approvals. After examination by the committee, the
researcher was granted research permission.
As highlighted in sub-section 3.4 and with regard to traditional and ethical rules, the
researcher always needed to consult the community leader or chief first before he was able to
take up any research in a designated study location. The process of data collection was only
possible after the community leaders have given their permission. To comply with local
ethics the researcher always respected this tradition, but in some cases the community
leader's permission was refused. Reasons were that the community leader demanded a small
"compensation" which the researcher was not willing to pay; or they complained, that
already many "white people" had come to their community with promises of help which
were never fulfilled.
Health and gender specific research and data is generally very sensitive and must
always be treated confidentially. To meet this standards, to protect and respects the human
rights of the study's participants, and to comply with the regulations and conditions set by the
Uganda National Council of Science and Technology, the researcher followed ethical
regulations. Interviews and discussions have been conducted in a private location where it
was not possible to overhear them. The researcher took particular care in ensuring that no
other people were present to observe the interviews, to protect privacy. Data obtained from
participants was for evaluation purpose only. No identifying information has been collected
from participants in the survey. All research material was maintained in a locked cabinet with
access only to the researcher. Collected information will not be passed on to any third party,
and will be treated confidential. Furthermore, the researcher can assure that there have been
no risks to participants during this study.
Participants and households will benefit from this study inform of knowledge
improvement regarding the economic impact of diarrhoeal diseases. Also, the risk-benefit
ratio is favourable since there are no risks but immediate benefits to participants. The
participants have been introduced to the purpose of the data collection activities and have
been asked for participation. And the researcher explained that participation is voluntary, and
that if a person agrees to participate, he/she can still refuse any question. No compensation
has been provided or paid to participants.
The analysed results and findings from the study will be predominantly used to support
a master thesis, however, the findings will also be made available to the School of Public
Health in Uganda for the benefit of the participants. Furthermore, a copy of the final thesis
will be submitted to the Council of Science and Technology as contribution to local health
research. The researcher will make sure, that all participants have access to the collected data
through the Uganda National Council of Science and Technology, so that they can benefit
4.10 Conclusion
In concluding the study's methodology, the study's epistemology is based on the
philosophical stances of positivism as the study is mostly of quantitative and objectivistic
nature. This choice has been justified in imitation of Crotty (1998), who argues that things
exist as significant entities independently of consciousness and experience, that they have
truth and meaning residing in them as objectives, and that scientific research can reach this
objective truth and meanings.
The target population have been households located in rural and suburban areas in
South Eastern Uganda. The researcher decided to study the household as a unit, and also
justified his decision to measure the direct financial and disposable household income for the
study's assessment of the micro-economic burden caused through diarrhoeal infections.
The main tool for data collection was a household survey based on a questionnaire,
which has been carried out in three different South Eastern districts. The questionnaire
focused on themes such as e.g. household structure, household income, health seeking
behaviour, costs for medical treatment, and disease prevention methods.
Other techniques included semi-structured interviews and observations. Criteria for the
selection of communities for data sampling were suburban and rural settings, sanitary and
housing conditions, people's standard of living, and the prevalence of diarrhoeal diseases.
Together with his interpreter, the researcher purposely surveyed and interviewed on average
ten households per community. Interviews have also been conducted with local health
The findings from the household survey will be statistical analysed with the computer
programs Microsoft-Excel and Minitab, and the findings from interviews and observations
will be transcribed in accordance to their relevance. The outcomes are analysed and
displayed in the following chapters.
Finally, the researcher highlighted the ethical considerations to prove the study's
concern for the ethical rights of the communities and people studied. Main issues are the
general sensitivity and legitimisation of the subject as well as the question about how the
participants can benefit from this study.
5. Analysis of locations, households, and of sanitation standards
5.1 Introduction
The present chapter presents and analyzes the study findings with regard to the selected
households in the sub-urban and rural samples. First of all, the main characteristics of the
household livelihoods will be described in order to understand the major income earning
activities of the members of these households in section 5.2. Secondly, their location and
living conditions in terms of housing structures and access to facilities and services, notably
sanitation, will be discussed in section 5.3. As the level of sanitation plays an important role
in people being at risk to diarrhoeal infections, the sanitation standards will be explored in-
depth. Thirdly, in section 5.4, on the basis of the survey, observation, and interview data
collected a comparison will be drawn between the two selected samples in order to determine
which households are relatively more at risk to diarrhoeal infections. The chapter conclusions
are drawn in section 5.5.
5.2 Household livelihoods
According to the household survey and to the researcher's observations, most agricultural
activities are almost impossible in the suburban and urban areas and slums due to the lack of
land and space available. Therefore, people's livelihoods are mainly shaped by the need to
create some form of financial income to purchase their needed commodities and groceries for
survival. Subsequently, the dominant forms of livelihoods of the survey's respondents in
urban and suburban areas in Uganda are formal and informal small-scale businesses, which
offer services like e.g. the trade of fruits, charcoal, and self-brewed alcohol to polishing
shoes, while the livelihoods of others is shaped by day labouring, and begging. Day
labouring and low paid physical and service work is the major type of disposable income for
most men and their households, while women usually manage all household related activities
including caring for children and dependents. Often they also have a small-scale business
going on to further support the financial and disposable household income. Women and
teenager in urban areas in Uganda often sell newspapers, cell-phone cards, crafts, or food
products like e.g. sweets and fruits in the streets and therefore contribute to a large proportion
to the informal business sector.
In contrast, people's livelihoods in rural areas are mainly defined through agricultural
activities such as e.g. the farming of livestock and crops like bananas, cane sugar, and maize.
Day labouring in the formal and informal agricultural sector and subsistence farming are the
common forms of disposable income generation. Some people also sell crafts and food items
like fruits and vegetables next to major roads. As a high proportion of household livelihoods
in rural areas are shaped by subsistence farming only, they are often more vulnerable to
seasonal variations like e.g. dry seasons or floods, though, the climatic conditions are
relatively stable in most of Uganda due to its geographical position on the equator.
However and in contrast to households in suburban slums, rural families and household often
own a small piece of land and livestock like e.g. chickens or a cow, and are able to survive
therefore through subsistence farming, which makes them less vulnerable to economic and
financial fluctuations. Also, people from rural areas often have better access to food such as
crops, meat, and dairy products, and the costs for food and housing are, compared to urban
areas, much lower.
One major disadvantage of the informal business sector compared to formal
employment is the lack of financial and social security. People who base their livelihoods on
informal kinds of income don't receive paid holidays or paid sick leave, and are usually not
insured against e.g. medical costs or death. For example, if the main "bread-earner" of a
household is ill, this situation will have consequences for all household members. Therefore,
households often need to find ways to mitigate and cope with unexpected (financial-) crises.
According to the survey, money for medical expenses, in both suburban and rural locations,
is in most cases extracted from the direct disposable household incomes. If the disposable
income is not enough, money is often borrowed from relatives or household items like e.g.
the mobile phone or the stereo are sold to create such finances. Though, as financial assets in
rural areas, compared to other livelihood assets, are of less importance it is often not possible
for households to invest much money in health care. If people in rural areas are in need of
expensive or private medical care they often need to sell other assets like e.g. livestock or a
piece of their land to generate money.
Nevertheless, due to the fact that most livelihood assets are gained through the formal
and informal business sector, people in urban areas are less affected by seasonal and climatic
variations. Though, changes in weather can influence the costs of local food, external factors
related to the world trade market have a much larger impact on people's disposable income,
especially in urban areas. This is one of the reasons why the urban household incomes
fluctuate much more in accordance to inflation rates and disposable money in circulation.
Therefore, the disposable incomes of people living off day labouring and begging are very
unreliable, and these people are usually more vulnerable to ill-health and to the financial
burden of diseases, with regard to the medical poverty trap explained in section 3.4.
When taken into consideration that rural households are less affluent in financial terms,
by including the affects of seasonal variations, rural households seem to be more vulnerable
to the financial burden of diarrhoeal infections.
5.3 Living conditions and access to health and sanitation facilities
With regard to the household survey, the number of people sharing one household ranges
from 2 to 9 household members in suburban communities, and from 2 to 10 household
members in rural communities. The average size of a group of household members sharing
one household in a rural community is with 4,8 household members slightly higher than to
4,5 household members in sub-urban communities (Table 5.1). Table 5.2 presents the
average mode of occupation, of main water source, and of dimensions of housing and
property separated by location.
Table 5.1 Household structures by location
Location
Mean No. of
Mean No. of female
Mean No. of
household members
household members
children below the
on average
on average
age of 12 years
Sub-urban
4,5 2,3 1,9
N = 45
Rural
4,8 3,1 1,8
N = 35
All
4,7 2,7 1,9
N = 80
Table 5.2 Mode of occupation, and of water source; and dimensions of housing
Location
Mode of occupation
Dimensions of
Source of fresh-
housing space and
water on average
of spaces between
houses on average
Sub-urban
Small-scale business
Community tap
water source
Community tap
and ground water
source
Women and children represent the largest groups of household members. The
researcher also counted the number of female headed households; however, the number was
low on average. The number of children per household below the age of 12 years in suburban
and rural communities ranged equally from zero to five children. However, rural households
had on average more children, which could be explained by the greater availability of farmed
food and by the higher demand in agricultural labour. Out of 45 suburban households, only
two households were female headed; and out of 35 rural households, no households turned to
be out as female headed. The researcher assumes that the ratio of female headed households
could be higher as estimated in this survey, as the sample size was relatively small compared
to the population size. It was the impression of the researcher that there is a much higher
number of female headed households in suburban and slum areas, which could be related to
the higher number of HIV/Aids infections among men in suburban areas.
With regard to informal conversations held with the mothers of households, the rate of
children from urban slums who receive basic education is relatively high compared to rural
areas; despite the fact that most households struggle to pay the school fees.
Also, security in the slums is only an issue during night time, even if some slums are subject
to organised crime. The researcher was able to observe, that the use of narcotic drugs like
opium and cannabis is common especially among street children.
Furthermore, rural villages are traditionally governed by a chief and the different districts of
a slum are controlled by a community leader who usually belongs to the major ethnic group
of the region. He controls most community activities and acts as a communal leader.
Most people in the slums have access to public, private, and traditional health facilities and
most medication is available through the private market. As most facilities available within
the Ugandan health sector are concentrated in suburban and urban areas, households located
in such places have a greater availability and choice of treatment. However, as private
medical facilities are usually much better in terms of treatment and hospitalisation,
appropriate and professional medical treatment is still a matter of money and depends on the
disposable household income available. Therefore, households or people who have only very
limited financial resources available, are usually only able to consult public health services or
health services provided by non-governmental organisations, which are mostly free of
charge. With regard to interviews held with local physicians, the prevalence of infectious
diseases in the slums is generally high and the most common illnesses, especially among
children and older people, are acute/viral respiratory infections, measles, and gastrointestinal
infections like typhus and hook worms. HIV/AIDS is also a common issue among people
living in slums. For example, an interviewed physician from the Mukwano Consultation
Clinic in Katanga slum mentioned: "yes, diarrhoeal diseases are very common here in the
slum and the level of sanitation standards is severe, however, diarrhoeal diseases are still
more common the rural areas due to the lack of proper functioning medical facilities".
Access to health care in rural areas is much lower and major health facilities like public
and private hospitals are mainly located in urban areas. Health services in rural areas are
dominated by public health centres and by some small semi-private health facilities managed
by religious missions or by non-governmental organisations like e.g. Medecins sans
Frontieres (Uganda Ministry of Health 2005). Also, the density of pharmacies in rural areas is
much lower. However, the traditional health sector still has considerable influence in some
rural places, and often they can be paid with items like food instead of money which again
saves the household's finances. Nevertheless, the prevalence of infectious diseases in rural
areas such as in the districts Wakiso and Jinja is much higher. Especially children below the
age of five years and people older than 60 years suffer often from infections with malaria,
HIV/Aids, acute respiratory illnesses, and diarrhoeal diseases like typhus and hook worms.
The interviewed physicians also mentioned that sleeping sickness (African Trypanosomiasis)
is increasing in rural places, especially in north and east Uganda. Outbreaks caused by
flaviviruses (e.g. yellow fever) and by viral hemorrhagic fevers like the Ebola and Marburg
virus are not uncommon in Uganda's western districts. A major Ebola outbreak had just been
embanked before the researcher arrived in Uganda. Malaria, acute respiratory infections, and
diarrhoeal infections are the major causes of childhood mortality in rural areas (Uganda
Bureau of Statistics 2006).
The researcher observed that the level of sanitation standards in the slums is often very
limited and the only facilities are communal latrines and communal water taps, which create
a perfect ground for pathogens related to diarrhoeal infections. The urban infrastructure of
the piped fresh water and sewage system is only of basic standard and can not adapt fast
enough to the growth of the slums, and the piped water is despite disinfection with chlorine
not regarded as drinkable without further treatment such as e.g. boiling or chemical
disinfection. Most people often need to queue for a long time until they can fill up their
canister with only a limited amount of water. Also, most houses in rural and sub-urban
communities lack proper toilet facilities, though, most rural houses have a private latrine, and
most urban slums are provided with communal latrines. However, in the urban slums,
hundreds of people often need to share one public latrine and often there is no possibility for
the user to even wash their hands. Furthermore, due to the lack of adequate sanitation and
drainage, babies and small children often play on grounds contaminated with sewage, which
probably is one of the reasons why they form the largest group of victims infected with
diarrhoeal diseases. Moreover, the relatively small and vulnerable bodies of children suffer
more from diarrhoeal infections because they contain less water and their immunity is
weaker. Generally, hygienic conditions or at least the overall hygienic situation with regard
to the disposal of organic waste, is much better in rural communities.
In rural villages and communities the researcher was able to observe, that the density of
the population and their houses and properties is much less, and the amount of people using
the same latrine is much lower too. The number of people living under one roof is often
much higher in rural places, and their houses are often larger and in a better shape compared
to the huts found in the suburban slums. Most people in rural areas live in small villages
which usually lack proper sanitation facilities and infrastructure. However, compared to
urban areas, most latrines are pit-latrines and are not connected to an (open) sewage system.
And more than 12 out of 100 people in rural places have no access to any kind of latrine or
toilet (Uganda Bureau of Statistics 2006). Potable water supply is also only basic in rural areas,
but most villages and communities possess their own well or borehole and therefore have
constant access to clean groundwater, if not contaminated by animal faeces. An increasing
number of rural villages are also gaining access to the piped water system as more
infrastructure projects are being implemented.
As everywhere in South-East Uganda, rural places are often impacted by floods during
the rainy season, and the people live very close to their livestock, which can lead to the
contamination of their houses with sewage. A major flood caused by heavy rains had just
occurred between the towns of Entebbe and Kampala when the researcher arrived in Uganda,
and according to the local supervisor "this is the best time to arrive in Uganda for research
about diarrhoea", as many people fell sick with diarrhoeal infections due to the flooding of
fresh water depots and open sewage canals.
5.4 Comparison of samples
One of the most obvious differences observed by the researcher with regard to rural and
suburban housing was that the density of the population and of the housing is extremely high
and concentrated in suburban communities in comparison to rural communities. Most people
there live in small huts made out of clay or corrugated iron sheets which are build often next
to open sewages. Whereas rural houses and properties tend to be larger in size and often also
contain some form of land used for the cultivation of crops.
It was the researcher's impression, that with appointment to hygiene and environmental
health, rural areas often seemed to have a cleaner and healthier environment, especially in
terms of sanitation and sewage disposal as descript in section 5.3. Even if the systems for
water supply and sewage disposal are more advanced and developed in the suburban and
urban locations, as observed by the researcher, the overall hygienic and sanitary conditions
seemed to be much better in the rural villages, which is probably due to the lower population
desity and to lower numbers of people who use the same latrines and water sources.
Additionally, and with regard to Hunter et al. (1993) stated in chapter 1.4, households in rural
locations seem to have more power over their water sources, as the water usually comes from
bore holes and wells belonging to the local community, and these water sources are not yet
connected to the public water system. Rural households are therefore more likely to protect
their water sources against contamination.
However, as the network and the accoutrements of urban health facilities is more advanced,
the rate of diarrhoeal diseases is according to one of the interviewed physicians still higher in
most rural locations. The prevalence of diarrhoeal infections will be analysed and compared
in more detail in the following chapter.
The household survey also revealed that the number of household members is slightly
higher in the rural villages as compared to the number of people sharing one household in the
suburban slums. Furthermore, when taken into consideration that rural households are less
affluent in financial terms (as argued in section 5.2), by including the affects of seasonal
variations, rural households seem to be more vulnerable to the financial burden of diarrhoeal
infections. Nevertheless, people from rural areas often have a better access to food like crops,
meat, and dairy products, and the costs for food and housing are compared to urban areas
When comparing all the differences in housing, livelihoods, and medical and sanitation
facilities between suburban slums and rural locations, the researcher would clearly argue that
rural households are less at risk from diarrhoeal infections, though medical treatment is better
in the urban centres.
5.5 Conclusion
According to the findings presented in section 5.3, there are considerable differences between
suburban and rural locations as well as between their households and people's livelihoods. In
both areas, people lack proper access to fresh water and appropriate sanitation facilities.
Interestingly, most of the rural places visited by the researcher had higher sanitation
standards when compared to the suburban slums. With regard to the literature reviewed in
chapters 1.3 & 1.4 about disease prevalence and prevention, one explanation for this
difference could be the extremely high density of households and people located in the
slums, followed by the fact that the ratio of people using the same water source and the same
latrine is also much higher in suburban slums as compared to rural villages.
The structures of the households showed no major differences between suburban and
rural locations, though the household survey revealed that the mean numbers of the total
household members and of females living in one household are slightly higher in rural
People's livelihoods and their sources of income differ considerably between suburban
and rural areas. Rural livelihoods are usually based on farming and on the agricultural sector,
whereas suburban and urban livelihoods are much more diverse in nature, ranging from
small-scale businesses to day labouring and begging. These findings correlate with the
literature revised about Uganda and its people in section 1.5, and also show that people's
livelihoods in suburban locations are more diverse. In contrast, household incomes in rural
places are less a subject to fluctuations due to the increased possibility of income smoothing
based on subsistence farming.
In conclusion, the analysis of the living conditions and of the medical and sanitation
facilities shows that households located in the slums are, despite better medical access, more
at risk to diarrhoeal infections due to the severe environmental and sanitary conditions.
6. Analysis of the prevalence of diseases and ill-health
6.1 Introduction
This chapter presents and analyzes the study findings with regard to the prevalence of
diarrhoeal infections and ill-health in the sub-urban and rural sample units. First of all, the
number and frequency of reported episodes of diarrhoeal symptoms among the households
interviewed will be measured in section 6.2, and secondly, the outcomes will be discussed
and compared with the location and the mean number of household members in section 6.3.
As these findings highlight the mean epidemiological rate of diarrhoeal infections among the
households surveyed, the epidemiological rate will be explored in-depth. This section will
also continue with the analysis and comparison of the samples, started in section 5.4, in order
to determine which households are relatively more at risk to diarrhoeal infections. The
chapter conclusions are drawn in section 6.4.
6.2 Disease prevalence and rate of infection
The findings of the household survey displayed below in Tables 6.1 and 6.2 reveal, that the
rate of households in which at least one household member suffered at least once in the
previous six months from a diarrhoeal infection is, on average, 60% much higher in sub-
urban slums as compared to a rate of 42% in rural areas. The researcher assumes, as already
mentioned in the previous chapter, that this result is probably created due to the much higher
rate of population and housing density in these areas, and due to better sewage disposal in
rural areas. Another explanation could be, that the rate of HIV/Aids infections is much higher
in suburban and urban areas, and that one of the symptoms of this disease is diarrhoea.
However, these assumptions are only speculations and cannot be proven through this survey.
The statistical analysis of the survey also declares that the number of different episodes
of diarrhoeal infections is also higher among sub-urban households compared to rural
households. These findings presented in Tables 6.1 and 6.2 show a clear contrast to the data
of Uganda's Demographic and Health Survey, which argues that more rural households are
affected by disease infections (Uganda Bureau of Statistics 2006a). However, the Demographic
and Health Survey compares the data from all Ugandan districts, including the very poor
ones in Northern and Southern Uganda and the refugee camps situated in rural areas, where
infection rates are generally higher as in Uganda's South-Eastern region. This could explain
why diarrhoeal infections are statistically more common in rural areas.
According to interviews with medical doctors, children are most affected by diarrhoeal
infections and more than half of the victims suffering from diarrhoea are children below the
age of five years. Nevertheless, this fact is already widely recognised by health experts, and
this finding also correlates with findings presented by the WHO (1996) and by Uganda's
Demographic and Health Survey (2006).
Despite the fact that these findings represent a timeframe of six months only, they
suggest a generally high prevalence of infectious diseases and of diarrhoea causing pathogens
in both rural and sub-urban areas over a longer time period and therefore demonstrate the
need for action.
Additionally, the analysis of the survey data declares, that only one of the interviewed
households suffered from a case of death which has been related to a diarrhoeal infection.
This finding suggests that most diarrhoea causing infections are less severe than infections
from other diseases like e.g. malaria or measles, and that their impact might be less dramatic
as if impacted by diseases which end more often deadly. Further research on this issue would
be necessary to be able to draw any definite conclusions.
Table 6.1 Rate of households impacted by diarrhoeal infections by location
Location
No. of diarrhoea Rate of total
households
impacted
households
household size
interviewed
households
over past 6
month
Sub-urban
Table 6.2 Rate of infection compared to No. of episodes and type of pathogen
Location
Percentage
Mean No. of episodes
Mode of common
of symptoms of
types of pathogens
households
diarrhoea on average
causing diarrhoea
infected
among positive
on average
households
Sub-urban
2,6 Salmonella,
Typhoid,
N = 45
1,5 Salmonella,
Typhoid,
N = 35
N = 80
The most common pathogens causing diarrhoeal infections are according to interviews
with experts conducted with local doctors are caused by the novo and rota virus, Salmonella
typhi and bacteria, Cryptosporidium, Shingella enteritis, and by hookworms such as e.g.
Ancylostoma duodenale. According to an interview with a paediatrician from the Mulago
Hospital in Kampala, more than 50% of all children in rural and in suburban areas suffer
from hookworm infections.
The researcher also found out through the same interview, that in response to this high
level of infection, the Ugandan Health Ministry launched anti-worm campaigns, where
antihelmintic medication is given to all children below the age of six years, basically before
they are enrolled in primary-school.
As already outlined in chapter 1.3, infections with hookworms can cause anaemia and
therefore reduce the physical and mental development of especially children. Also mentioned
in chapter 1.3, a high endemic rate of hookworms can have dramatic impacts on the micro-
and macroeconomy. The interviewed paediatrician stated as well, that lots of children in the
slums die from infections with measles, compared to high malaria infection rates in rural
areas. However, she also said: "children are still most impacted by diarrhoeal diseases, and
they are the ones who are least able to cope with the affects of ill-health", furthermore
"especially infections with typhus and e.coli are common among young children, and
immediate treatment is essential to avoid death".
When asked about the gender ratio of people infected with diarrhoeal diseases seeking
treatment, the interviewed paediatrician interestingly mentioned: "most patients are male
children". This answer was similar to the answer of the interviewed physician from the
Mukwano Consultation Clinic who stated "most patients are adult males", though his clinic
is a private health facility. However, the researcher is not able to prove if this finding is a
result of gender specific disadvantages or if the infection rate of males is simply higher.
Another physician from Mengo Hospital in Kampala stated: "the number of people
infected with diarrhoeal infections is relatively high among the poor people living in the
slums, however, this is not only an urban issue", also "the lack of clean water and of proper
sanitation facilities seems to be the main problem, and people need to be better educated
about hygiene practices".
6.3 Comparison of samples
With regard to prevalence of diarrhoeal pathogens, and with regard to the groups mostly
impacted them, the findings from the expert interviews clearly correlate with the findings
presented by the WHO and WaterAid which have been stated in chapter 1.3. As indicated by
the literature, children are among the most affected by diarrhoeal infections. Also, poor
sanitary standards and a poor knowledge of hygienic practise seems to be a problem, which
again are good conditions for the prevalence of diarrhoeal infections with regard to
information provided by WaterAid (2007).
The results of the statistical analysis of the household survey clearly show that the rate
of diarrhoeal infections is considerably higher in the suburban slums as compared to the rate
of infections in the rural areas. Interestingly, this finding stands in contrast to the findings of
the Ugandan Bureau of Statistics (2006) presented in chapter 1.3.
Additionally, when comparing this finding to the poor living and sanitary conditions of the
slums mentioned in chapter 5.4, it is not surprising that households located in slums are more
affected by ill-health. Moreover, this finding correlates with the widely accepted assumption
that diarrhoeal infections are strongly related to poor sanitary conditions.
Though, the researcher visited only three different rural locations and therefore can't
generalise this finding for all of Uganda.
Nevertheless, sanitary measures in the slums were disastrous as compared to the three
villages surveyed, and therefore the researcher sees his assumption made in chapter 5.5
confirmed, and again argues, that households located in the slums are, despite better medical
access, more at risk to diarrhoeal infections.
6.4 Conclusion
In conclusion, the analysis of the epidemiological rate of diarrhoeal infections reveals that the
surveyed slums have a much higher rate (60%) of households impacted by diarrhoeal
infections as compared to the rate of infections of the surveyed rural villages (42%). Also,
the mean number of episodes of diarrhoeal infections is higher among sub-urban households
(2.6) as compared to rural households (1.5), see Table 6.2.
With regard to the study's findings already outlined, it is suspected that the poor
environmental and sanitary conditions found in the slums, are the main cause for the high
rate of infections with diarrhoeal diseases. Generally, the rate of diarrhoea causing infections
is, on average 51% considerably high, and therefore highlights the need for action.
7. Health seeking behaviour
7.1 Introduction
The present chapter presents and analyses the study findings with regard to people's health
seeking behaviour. First of all, the rates of diarrhoea impacted households which consulted
public, private, and alternative health facilities as well as the related costs for medical
treatment, and transport used to reach the facility will be analysed in section 7.2. Secondly, a
chi-square test and a regression and scatter plot analysis will be carried out in section 7.3, to
find out, if the total medical treatment costs, respectively, if the behaviour of paying for such
services, is related to the direct financial and disposable household income. Thirdly, the
researcher will analyse in section 7.4 the costs for special food, which is often needed by
infected patients for recovery from ill-health. Section 7.5 will analyse disease prevention
methods of the households as well as the related cost burdens. In order to find out, if the costs
for disease prevention methods are related to the direct disposable household income, a chi-
square test and a regression and scatter plot analysis will be carried out in section 7.6.
Finally, in section 7.7, on the basis of the survey, observation, and interview data collected a
comparison will be drawn between the two selected samples in order to determine and to
discuss any differences found, followed by the chapter's conclusion.
7.2 Analysis of the health seeking behaviour
The findings from the household survey and its different variables and concepts defining the
health seeking behaviour are displayed below in Tables 7.1 to 7.10 and in Figure 7.1 and 7.2
with regard to the study's findings. The direct disposable income and spending is presented
in the local currency Ugandan Shilling (UGX), which is currently in relation to US$ 1 UGX
1,700. Also, this study considers, in accordance with the Ugandan Health Sector Strategic
Plan 2, all non-public health facilities as private-sector health facilities. This includes as well
missionary hospitals and health facilities operated by non-governmental organisations.
The rate of households in rural communities impacted by diarrhoeal infections which
were seeking professional medical treatment is according to the survey (see Table 7.1) with
87% considerably higher as compared to households in sub-urban communities. On average,
most victims (74%) of diarrhoeal infections are seeking professional medical attention.
The percentage of people who consulted a traditional healer was according to the
household survey surprisingly very low (see Table 7.1). The interview held with the
physician from the private Mukwano Consultation Clinic confirmed this finding: "the rate of
people who consulted a traditional healer only is declining since the Ugandan government
disposed most user fees for the public health system. However, in very remote regions of the
country are traditional healers still very common, especially in Southern and Western
Table 7.1 Health care seeking behaviour
Location
Percentage of positive
Percentage of positive
cases who took up
cases who took up
professional medical
alternative treatment
treatment
Sub-urban
N = 27
Rural
N = 15
All
N = 42
As described in Table 7.2, the average rate of people being affected by diarrhoeal
infections who consulted a pharmacist only was with 13% considerably low too. Still,
households located in sub-urban locations consulted pharmacies on average more often.
Table 7.2 Pharmacy consultation only
Location
No. of diarrhoea
Percentage of
impacted households diarrhoea impacted
who only consulted a
households who only
pharmacy for
consulted a pharmacy
treatment
for treatment
Sub-urban
3
11,1%
N = 27
Rural
1
6,7%
N = 15
All
4
9,5%
N = 42
The transport time for people to reach professional medical care has in all cases been
less than six hours (see Table 7.3), which indicates that the network of medical facilities is
relatively well expanded. Also, the financial amounts spend for transportation is on average
not very high, and don't seem to have such a big impact on the household's savings. Costs
for transport range in suburban areas from only 500 UGX to 2,000 UGX (US$ 0.30 – 1.18),
and in rural areas from 400 UGX to 3,000 UGX (US$ 0.24 – 1.77).
Most people seeking medical attention are, especially in sub-urban areas, accompanied
by a household member. Though, most patients who are being accompanied by somebody
are children who come together with their mothers. In contrast, adults suffering from
diarrhoeal infections are almost never accompanied by another household member, whereas
children are almost always accompanied by someone.
Table 7.3 Time, transport, and company
Location
Mean time spend
Percentage of positive
Money spent on
for examination,
cases who have been
transport to the
treatment,
accompanied
doctor/hospital on
transport on
Sub-urban
88% 1.000 UGX
N = 27
57% 1.730 UGX
N = 15
73% 1.365 UGX
N = 42
During the process of surveying and due to observations, the researcher also found
evidence which indicates that the health seeking behaviour within a household or a family is
often influenced by certain hierarchies. Often, only the man or father of the family makes
major decisions and decides about major household spending or if a household member is
brought to a hospital. Adult household members impacted by severe and bloody diarrhoea are
almost always granted permission for ambulant and stationary medical treatment. In contrast,
it is suspected that especially in very poor households children are often denied access to
costly medical treatment and are therefore suffering most. These inequalities based on age
are in line with observations made by Haddad et al. (1993), Sauerborn et al. (1996), Garg et
al. (1998), who argue (see chapter 4.3) that the underlying reason for this issue is that the
household's income spent for healthcare is usually concentrated on productive members
instead of spreading it between all indigent household members.
The interviewed physician from the Mukwano Consultation Clinic also mentioned that most
of his patients are adults, though his clinic is a private health facility which charges UGX
20.000 ($12) per standard consultation. Also, this finding confirms the findings of Su et al.
(2006) who argue that ill-health is usually associated with higher expenses for medical care
when adult household members are involved (see chapter 4.3).
In contrast to the survey results gained from rural locations, is the rate of people
affected by diarrhoeal infections in sub-urban areas who consulted a public health facility
with 63% almost double compared to the same rate of people living in rural areas (see Table
7.4). Even if the medical treatment in public hospitals is (according to the researcher's
observations) often very basic and inadequate, and most public hospitals lack proper
medication and drugs. According to the interview held with the paediatrician from the public
Mulago Hospital, private health facilities often also offer a better cost-performance ratio as
most fees for private medical treatment already include the costs for medication and drugs. In
contrast to patients seeking treatment at public health facilities, who usually get
Table 7.4 Medical treatment costs
Location
Percentage of
Money spend for
Money spend for
positive cases who
treatment only on
used public health
from pharmacies
facilities
only on average
Sub-urban
63% 8.280 UGX 2.000 UGX
N = 27
Rural
29% 11.400 UGX 2.940 UGX
N = 15
All
46% 9.840 UGX 2.470 UGX
N = 42
medication prescribed which the public facility can't afford and which are not available at
this facility. But often, most people can't afford them either, and as a result of poor medical
supply, they need to abstain from them and therefore receive inadequate treatment. However,
public health facilities provide a prophylaxis against worm infections, and most major
vaccinations against childhood infections are free of charge for all children under the age of
six. Unfortunately, according to the interview, a lot of poor households in sub-urban and
rural areas are not aware about these complementary services.
According to the household survey, costs for private or semi-private health services
seem to be much higher in suburban and urban areas. This is very likely due to the fact, the
most private-sector health facilities in rural areas are dominated by non-governmental
organisations like e.g. mission hospitals. In contrast, most private-sector health facilities in
urban areas are dominated by private health practitioners (PHPs), who charge much higher
fees. The costs for medical treatment only ranged in suburban areas from zero to 40,000
UGX (US$ 23.53) and above, and in rural areas from zero to 15,000 UGX (US$ 8.82). The
expenses for professional medical treatment of diarrhoeal infections are on average slightly
higher in rural areas, but make up a huge proportion of the disease related economic burden
in both, rural and sub-urban areas. The costs for medication only are much lower as
compared to the treatment costs. They ranged from 500 UGX to 16,000 UGX (US$ 0.29 –
9.41) in suburban areas, and from 500 UGX to 10,000 (US$ 0.29 – 5.88) in the villages.
Although, according to interviews, some people collect traditional herbs for self treatment,
and therefore don't have any expenses.
Another issue discussed in all interviews, is the fact that most public doctors and
hospitals don't apply laboratory tests to properly diagnose the exact pathogen which caused
the infection. Public health facilities often lack finances, proper diagnostic equipment, and
expertise to carry out laboratory tests. However, a physician from Mengo Hospital
mentioned: "the situation is improving in sub-urban and urban areas. For example,
Uganda's capital Kampala developed a good network of public and private laboratories, and
laboratory specific studies and university courses are being extensively supported through a
government education scheme". Still, doctors can often only guess the reason for the
infection based on clinical symptoms, and often link symptoms of diarrhoea to malaria or to
bacterial infections and therefore almost always apply a treatment based on the availability of
either chloroquine, Coartem® (artemether-lumefantrine) or on antibiotics like Ciprofloxacin
or Doxicycline, or on a oral dehydrations therapy (ORT). Also, as most diarrhoeal infections
are treated in a similar way anyway and often even with the same medication, standard
treatment procedures based only on symptoms are still a much better solution as compared to
7.3 Chi-square test, regression and scatter plot analysis
To find out, if the total medical treatment costs (including costs for medications/drugs,
transport, and special food), respectively if the behaviour of paying for such services, are
related to the direct disposable household income, a chi-square test and a regression and
scatter plot analysis have been carried out.
Table 7.5 Association between medical treatment costs / direct household income
Chi-Square Test: test for association between total medical treatment costs
and direct household income
Expected counts are printed below observed counts
Chi-Square contributions are printed below expected counts
C1 C2 Total
1 500 30000 30500
2594,87 27905,13
1691,212 157,264
31 32000 180000 212000
18036,46 193963,54
10810,346 1005,243
N
Total 378000 4065000 4443000
Chi-Sq = 362782,528; DF = 30; P-Value = 0,000
Null hypothesis: there is an association between the total medical costs and the
direct household income.
Result: the null hypothesis can be rejected as the P-value is below 5%
Conclusion: there are no associations between the total treatment costs and the
direct household income. Therefore, the investment in medical treatment is not
dependent on the household income.
Table 7.6 Correlation between medical treatment costs and direct household income
Regression Analysis: Medical treatment costs versus Direct household
income
The regression equation is
Medical treatment costs = 6265 + 0,0452 Direct household income
Predictor Coef SE Coef T P
Constant 6265 4028 1,56 0,131
Household income 0,04521 0,02571 1,76 0,089
N = 31 S = 12270,3 R-Sq = 9,6% R-Sq(adj) = 6,5%
Analysis of Variance
Source DF SS MS F P
Regression 1 465584782 465584782 3,09 0,089
Residual Error 29 4366253928 150560480
Total 30 4831838710
Medical
Household treatment
Obs income costs Fit SE Fit Residual St Resid
9 150000 40000 13047 2257 26953 2,23R
19 40000 40000 8074 3216 31926 2,70R
Null hypothesis: the population correlation between the total medical treatment
costs and the direct household income is zero.
Results: the Null hypothesis cannot be rejected as the P-value is above 5% and the
regression square is only 9.6%.
Conclusion: the population correlation is not significantly greater than zero, and
there is no linear relationship between X and Y for each value.
Scatterplot of Medical treatment costs vs Household income
Figure 7.1 Scatterplot of medical treatment costs vs. direct household income
The results outlined in Tables 7.5 and 7.6 and in Figure 7.1 reveal, that there are no
associations or correlations between the total medical treatment costs and the direct
disposable household income. Also, the population correlation between both variables is
almost zero. However, by close inspection of the scatter plot (Figure 7.1), and by excluding
the most extreme outliers, the scatter plot analysis reveals a weak association between the
total medical costs and the total direct disposable household income.
7.4 Special food
Many households affected by ill-health through diarrhoeal infections changed food
consumption patterns, either as part of the victim's therapy or to prevent future infections.
The statistical analysis of the household survey reveals, that special food based on a
high quality and on a high nutrition content like e.g. beef, fresh vegetables, milk powder, or
vitamin tablets is usually more expensive, and can (as presented in Table 7.7) make up a high
proportion of the total treatment costs and of the economic burden caused by diarrhoeal
infections. According to the survey's findings, costs for special food in suburban areas and in
slums ranged from zero to 40,000 UGX (US$ 23.53) compared to a maximum price of
30,000 UGX (US$ 17.65) in rural areas. Also, more households in rural areas invest in
special food after being hit by diarrhoeal infection, compared to households in sub-urban
areas. Moreover, the costs for special food are on average nearly as high as for professional
medical treatment. However, especially households in rural communities are often able to
farm and produce their own food and can therefore subsidise financial losses through this
ability. Therefore, it is not surprising that the rate of people in rural communities who
required special food is 24% higher as compared to the rate in suburban communities (see
Table 7.7). Moreover, rural households often sell their agricultural surplus, and therefore
Table 7.7 Special Food
Location
Percentage of affected
Money spend on special
households who
food on average per
required special food
Sub-urban
30%
11.700 UGX
N = 27
Rural
54%
10.080 UGX
N = 15
All
42%
10.890 UGX
N = 42
increase their risk-economic ability, which gives them a strong advantage compared to their
urban counterparts. However, this procedure can be influenced by seasonal variations and
rural households can therefore not always rely on their own farm output.
According to the household survey, the expenses for special food are among the
highest, apart from disease prevention costs and medical treatment costs. Therefore,
unplanned household expenses for special food can cause an enormous economic burden for
households, especially for suburban and urban households.
7.5 Disease prevention methods
According to the household survey most people in rural and in sub-urban areas are aware
about the prevalence of infectious diseases, and about the fact that the piped water is not
drinkable, therefore most households (about 95%) apply disease preventive measures.
The most common disease prevention methods, mentioned by households during the
survey, are the boiling of water, the use of mosquito nets, and the appliance of hygienic
measures like hand-washing and the use of soap. According to the survey, out of 45
interviewed households in suburban communities 34 households (76%) boiled their water
before using it, 23 households (50%) used soap when washing their hands, 12 households
(26%) used mosquito nets during the night, and 5 households (11%) even used chemicals
(e.g. purification tablets based on silver ions, chlorine, and natriumdichlorisocyanurat) for
water treatment.
In contrast, out of 35 interviewed households in rural communities 25 households
(71%) boiled their water, 22 households (63%) used soap, 13 households (28%) used
mosquito nets, and 3 households (8%) used chemical prevention methods. One household
head explained, that he disinfects his water by mixing it with aloe-Vera before drinking it.
The analysis shows, that boiling of water and chemical treatment for water disinfection are
more popular among suburban households. Though, water purification tablets are expensive
and often not available in rural areas. Interestingly, rural households use on average 13%
more soap for personal hygiene compared to suburban households.
Furthermore and according to the cross tabulation (see Table 7.8 & 7.9), the results
from the survey clearly show that households which have a higher disposable income suffer
much less from diarrhoeal infections (see Table 8.1 in the following chapter).
Additionally, disease prevention techniques can be considerably expensive with regard to the
survey's outcomes, as people e.g. need to by charcoal to boil water or they need to buy soap
for personal hygiene. Households in sub-urban communities invest on average more money
in disease prevention compared to households in rural communities. The reason for this could
be the fact, that the rate of infections is much higher in sub-urban areas.
On average, about 10% of the total monthly household income in rural and sub-urban areas is
being invested in disease prevention methods.
Table 7.8 Rate of infection versus investments in disease prevention 1
Location
Percentage of Money spent for disease
Money spent for disease
prevention
prevention
infection rate
measurements on
measurements on
average per month -
average per month -
positive cases only
negative cases only
N = 80
N = 42
N = 38
Sub-urban
10.330 UGX 20.594 UGX
9.375 UGX 12.313 UGX
9.853 UGX 16.454 UGX
Table 7.9 Rate of infection versus investments in disease prevention 2
Location
Percentage of
Money spent for
Total rate of disease
mean infection
disease prevention
prevention costs
measurements on
compared to the total
average per month -
direct income
all cases
N = 80
Sub-urban
60% 15.462 UGX 13.70%
42% 10.844 UGX 8.30%
51% 13.154 UGX 11.0 %
7.6 Chi-square test, regression and scatter-plot analysis
To find out, if the costs for disease prevention methods, respectively if the behaviour of
investing in such techniques, are related to the direct disposable household income, a chi-
square test and a regression and scatter plot analysis have been carried out. The results
(which are outlined below in Tables 7.10 and 7.11 and in Figure 7.2) reveal that there are no
associations or correlations between the total disease prevention costs and the disposable
household income. Also, the population correlation between both variables is almost zero.
Though, households with an income above the average generally invest more in disease
prevention methods. Most households, including the poor ones, adapt their level of disease
prevention efforts to the environmental conditions they live in. Also, by close inspection of
the scatter plot (see Figure 7.2), and by excluding the most extreme outliers, the scatter plot
analysis reveals a weak association between disease prevention costs and the total direct
disposable household income. Still, the result of the scatter plot analysis is clearly negative
due to the high number of outliers.
Table 7.10 Association between disease prevention costs and household income
Chi-Square Test: Association between Disease prevention costs
and direct household income
Expected counts are printed below observed counts
Chi-Square contributions are printed below expected counts
Disease
prevention Household
costs income Total
1 2000 30000 32000
2304,88 29695,12
40,329 3,130
80 3500 158000 161500
11632,46 149867,54
5685,544 441,302
N
Total 919000 11840000 12759000
Chi-Sq = 927454,662; DF = 79; P-Value = 0,000
Null hypothesis: there is an association between the costs for disease prevention
methods and the direct household income.
Result: the null hypothesis can be rejected as the P-value is below 5%
Conclusion: there are no associations between the costs for disease prevention
methods and the direct household income. Therefore, the investment in disease
prevention is not dependent on the household income.
Table 7.11 Correlation between disease prevention costs and household income
Regression Analysis: Disease prevention costs versus Household income
The regression equation is
Disease prevention costs = 2995 + 0,0574 direct household income
Predictor Coef SE Coef T P
Constant 2995 2871 1,04 0,300
Household income 0,05738 0,01603 3,58 0,001
N = 80 S = 14465,9 R-Sq = 14,1% R-Sq(adj) = 13,0%
Analysis of Variance
Source DF SS MS F P
Regression 1 2683138041 2683138041 12,82 0,001
Residual Error 78 16322349459 209260890
Total 79 19005487500
Disease
Household prevention
Obs income costs Fit SE Fit Residual St Resid
19 320000 52000 21358 3196 30642 2,17R
34 90000 50000 8159 1865 41841 2,92R
43 200000 50000 14471 1819 35529 2,48R
45 300000 100000 20210 2924 79790 5,63R
48 650000 3500 40294 8206 -36794 -3,09RX
Null hypothesis: the population correlation between the costs for disease prevention
and the direct household income is zero.
Results: the Null hypothesis cannot be rejected as the P-value is above 5% and the
regression square is only 14.1%.
Conclusion: the population correlation is not significantly greater than zero, and
there is no linear relationship between X and Y for each value.
Scatterplot of Disease prevention costs vs Household income
Figure 7.2 Disease prevention costs vs. direct household income
7.7 Comparison of samples and conclusion
The findings from the household survey clearly show some differences between the slums
and the rural villages with regard to health seeking behaviour and with regard to disease
prevention methods.
With regard to the analysed survey data, the analysis of the health seeking behaviour
reveals that on average 74% of people suffering from symptoms of diarrhoea consulted for
professional medical treatment. Interestingly, the rate is with 87% slightly higher in rural
locations as compared to the rate of 61% in sub-urban communities. As the health sector is
less developed in rural areas, the only explanation for this outcome the researcher could think
of is that maybe that in rural places the diarrhoeal infections and their pathogens are on
average more severe as compared to most infections in suburban places. However, as this
study implies no laboratory analysis, the researcher can only assume this suspicion.
Furthermore, the rate of people affected by diarrhoeal infections in sub-urban areas who
consulted a public health facility is with 63% almost double as high as compared to the same
rate of people living in rural areas (see Table 7.4). This finding is probably explained by the
fact that costs for private or semi-private health services seem to be much higher in suburban
and urban areas. Also, most private-sector health facilities in rural areas are dominated by
non-governmental organisations like e.g. mission hospitals. In contrast, most private-sector
health facilities in urban areas are dominated by private health practitioners (PHPs), who
charge much higher fees. Also, competition between the private health facilities is much
greater in urban areas as observed by the researcher.
With regard to the chi-square test and the regression and scatter-plot analysis, the
researcher was not able to find any associations between the medical treatment costs and the
direct disposable household income. This finding indicates that the health seeking behaviour
is not always connected to the household's wealth, but to the severity of the disease. Though,
as the study analysed the disposable household income only, it may underestimates the
consumption levels of the rural poor and their ability for consumption smoothing. The
researcher recons, that the outcomes might very well be different when another measure of
household income would have been used.
The times for the patient's transportation to the health facilities were in all cases below
six hours, and none of the interviewed patients paid considerable high amounts for it. The
only small difference observed was, that patients from rural locations pay on average UGX
1,000 ($0.60) more for transportation to a health facility, which is probably due to the fact
that the network of health facilities in rural areas is less dense, and that distances between the
health facilities are larger as compared to urban areas. Nevertheless, even small amounts
contribute to the total financial burden caused by the diarrhoeal infection and have therefore
been taken into consideration. Meanwhile, the low figures for transport time and costs are
probably explained by the researcher's choice for research locations near (max. 5 kilometres)
health facilities.
The analysis of the expenses for special food revealed, that less than 42% of the
surveyed households, which have been impacted by a diarrhoeal infection, required special
food. However, the costs for special food were much higher in the sub-urban locations as
compared to the rural villages. This is may explained due to the fact, that most livelihoods of
rural households are based on subsistence farming, and that the prises for food are therefore
lower in rural areas. Also, more households in rural areas demanded special food after being
hit by diarrhoeal infection, compared to households in sub-urban areas.
Moreover, the costs for special foods are on average nearly as high as for professional
medical treatment and therefore contribute to a very high proportion to the total cost burden
of diarrhoeal infections.
Furthermore, the researcher found out through his survey that almost all households in
suburban and in rural household apply some kind of disease prevention method.
Interestingly, the rate of households in sub-urban and in rural areas which boiled water for
disinfection, which used mosquito nets during nights, and which used chemicals for
disinfection was almost equal. Only the rate of households, which used soap when washing
hands, was with 63% higher in rural communities as compared to the sub-urban
communities. The chi-square test, the regression and the scatter-plot analysis revealed that
there is no clear association between the direct disposable household income and the costs for
disease prevention methods. One explanation for this finding could be, that the prevalence of
pathogens and of their hosts is so high in certain areas (like e.g. in slums) that the households
have no choice and are constrained to apply disease prevent methods if they don't want to be
impacted by ill-health. Generally, the costs for disease prevention methods are very high and
also contribute to a large proportion to the total cost burden of diarrhoeal infections.
Concerning the answering of the study's research questions, and with respect to the
findings made within this chapter, the researcher is now able to answer the first, and partly,
the second sub-question, thus: rural households seem to prefer private and traditional health
care as compared to sub-urban households which prefer public health care. Though, this
conclusion is based only on quantitative findings, which is why the researcher believes, that
this outcome is less influenced by choice but by the availability and by people's possibilities
to access public, private, or alternative health care facilities.
8. Economic burden of diarrhoeal infections on households
8.1 Introduction
This chapter presents and analyses the study findings with regard to the household's
economic and financial burden caused through diarrhoeal infections. First of all, the overall
financial burden for the sub-urban and rural households will be assessed through a statistical
analysis in section 8.2. Secondly, a chi-square test, a regression and a scatter-plot analysis
will be conducted in section 8.3 to find out, if the total disease related costs are related to the
disposable household income. Thirdly, in section 8.4, on the basis of the household survey, a
comparison will be drawn between the two selected samples in order to determine which
households are financially more impacted by the burden of ill-health and by diarrhoeal
infections, followed by the chapter's conclusion.
8.2 Analysis of the financial impact
As already outlined in chapter 5.2, people's livelihoods in rural areas are dominated by
farming, and livelihoods in sub-urban and urban areas are mainly dominated by small-scale
and informal businesses, followed by day labouring and begging. Interestingly and according
to the analysed results of the household survey, people in rural areas seem to earn on average
a little bit more money (see Table 8.1) compared to people who work in the slums.
Nevertheless, one should keep in mind, that Uganda's South-Eastern rural districts are
relatively well developed (for African conditions) due to large-scale industrial farming
activities, whereas paid labour is difficult to find in the slums or in refugee camps.
Furthermore, rural communities have the major advantage that they can produce their own
food and they can sell their agricultural surplus to the urban centres. However, the direct
income range in suburban areas is, according to the survey, with zero to 650,000 UGX (US$
382) larger than the direct income range in rural areas, which is between 20,000 and 350,000
UGX (US$ 12 – US$ 206); however, the number of working household members is higher in
rural areas. These findings also correlate with the data presented in Uganda's National
Household Survey (Uganda Bureau of Statistics 2006b).
Table 8.1 Income versus rate of infection
Location
Percentage
Direct income on
Direct income on
Direct income
average per
average per
on average per
infection rate month - positive
month and per
month and per
household capita
household
- negative cases
capita - all cases
N = 80
N = 42
N = 38
N = 80
Sub-urban
113.000 UGX
135.500 UGX
124.250 UGX
130.000 UGX
220.000 UGX
175.000 UGX
121.500 UGX
177.750 UGX
149.625 UGX
Table 8.2 Income ratio between infected and uninfected households and working
household members
Location
No. of working
Direct income on
Direct income
Direct income
household
average per month
on average per
on average per
members on
and per household
month and per
month and per
capita - positive
household
household
capita - negative
capita - all
N = 80
N = 42
N = 38
N = 80
Sub-urban
1
113.000 UGX 135.500 UGX 124.250 UGX
2
130.000 UGX
220.000 UGX 175.000 UGX
1,5 121.500 UGX
177.750 UGX
149.625 UGX
Moreover, the results from the cross tabulation in Tables 8.1 and 8.2 indicate, that the
direct disposable income of most households which suffered from diarrhoeal infections is
lower on average compared to the income of households which didn't suffered from ill-
health and diarrhoeal infections in the previous six month of the survey.
According to the results of the survey outlined in chapter 7, households impacted by
diarrhoeal infections suffer in financial terms most from the direct costs for professional
medical treatment and from the costs for special food, if required. Additionally, after
counting all the different expenses caused through the diarrhoeal infection together, such as
e.g. costs for medical treatment, transportation, medication, and special food, the results
reveal, that the total rate of disease related expenses per episode of diarrhoeal infection,
compared to the total direct and monthly disposable household income, makes up on average
more than 20% of the total disposable household income (see Table 8.3). And if counted
together with the total costs for disease prevention methods, the total rate of disease related
expenses, compared to the total household income, makes up on average even more than
30% of the total disposable household income. Therefore, the study's findings suggest that
diarrhoeal infections do have an enormous economic impact on individuals and on
household's finances.
Table 8.3 Total financial burden caused by diarrhoeal infections on households
Location
Total rate of disease Total rate of disease
Total rate of disease
prevention costs
related costs
related costs
compared to the
compared to the total
compared to the
total income
income excl.
total income incl.
prevention costs
prevention costs
Sub-urban
13,70%
N = 45
8,30%
N = 35
All
11,00%
N = 80
The direct financial burden caused by diarrhoeal infection has been set in relation to the
direct and disposable monthly household income on average. However, when the total
financial disease burden is compared to the direct household income over a longer time
period such as e.g. one year or longer, the total financial disease burden will be more evenly
spread too and therefore becomes less severe. Though, this depends on the household's
ability and strategies to cope with the economic burden, on the number of episodes, and on
its ability to evenly spread the financial burden over several months. Nevertheless, this
calculation has measured only the direct financial costs created through diarrhoeal infections,
but not the indirect costs like e.g. lost productive time and power. Therefore, the real
economic burden caused by ill-health would probably be much higher, if all variables would
have been taken into consideration.
8.3 Chi-square test, regression and scatter-plot analysis
To find out, if the total disease related costs are related to the direct disposable household
income, a chi-square test and a regression and scatter plot analysis have been carried out. The
results (which are outlined below in Tables 8.4 and 8.5 and in Figure 8.1) reveal that there
are no statistical associations or correlations between the total diseases related costs and the
direct disposable household income. Also, the population correlation between both variables
is almost zero. However, this does not mean, that ill-health caused though diarrhoeal
infections has no economic impact. It basically means that the level or amount of disease
related costs is not dependent on the disposable household income. But again, by close
inspection of the scatter plot (see Figure 8.1), and by excluding the most extreme outliers, the
scatter plot analysis reveals a weak association between the total disease related costs and the
total direct disposable household income.
Table 8.4 Association between total disease related costs and direct household income
Chi-Square Test: Association between total disease related costs
and direct household income
Expected counts are printed below observed counts
Chi-Square contributions are printed below expected counts
Total disease Household
related costs income Total
1 2500 30000 32500
6074,33 26425,67
2103,249 483,463
31 17000 180000 197000 36819,78 160180,22 10668,821 2452,385 N Total 934400 4065000 4999400
Chi-Sq = 436133,869; DF = 30; P-Value = 0,000
Null hypothesis: there is an association between the total disease related costs
and the direct household income.
Result: the null hypothesis can be rejected as the P-value is below 5%
Conclusion: there are no associations between the total disease related costs and
the household income. Therefore, the investment in better health is not necessarily
dependent on the direct household income.
Table 8.5 Correlation between disease related costs and direct household income
Regression Analysis: Total disease related costs versus Household
income
The regression equation is
Total disease related costs = 19882 + 0,0782 direct household income
Predictor Coef SE Coef T P
Constant 19882 6760 2,94 0,006
Household income 0,07824 0,04315 1,81 0,080
S = 20595,8 R-Sq = 10,2% R-Sq(adj) = 7,1%
Analysis of Variance
Source DF SS MS F P
Regression 1 1394559800 1394559800 3,29 0,080
Residual Error 29 12301475684 424188817
Total 30 13696035484
Total
disease
Household related
Obs income costs Fit SE Fit Residual St Resid
11 300000 85000 43355 8172 41645 2,20R
13 90000 70000 26924 4103 43076 2,13R
Null hypothesis: the population correlation between the total disease related costs
and the household income is zero.
Results: the Null hypothesis cannot be rejected as the P-value is above 5% and the
regression square is only 10.2%.
Conclusion: the population correlation is not significantly greater than zero, and
there is no linear relationship between X and Y for each value.
Scatterplot of Total disease related costs vs Household income
dtela 50000 ree 40000
saeis 30000l dta 20000
Figure 8.1 Total disease related costs vs. direct household income
8.4 Comparison of samples and conclusion
Interestingly, when the disposable household income is set in comparison to the location the
survey reveals, that people in rural areas seem to have a higher income compared to people
who live in the sub-urban slums. Nevertheless, one should keep in mind that the
unemployment rate is relatively high in the slums, and as mentioned in chapter 5.2 the
income in urban areas fluctuates more. Furthermore, rural communities have the major
advantage that they can produce their own food as most of their livelihoods are based on
subsistence farming, and they can sell their agricultural surplus to the urban centres.
However, the financial income range is when set in comparison to the location, much larger
in the sub-urban areas, which is not surprising when considering that most livelihoods there
are based on small-scale and service industries. In contrast, the number of working household
members is higher in rural areas, which is most likely explained by the fact that most rural
households gain their income from agricultural activities.
Moreover, the results from the cross tabulation in Tables 8.1 and 8.2 indicate, that the
direct disposable income of most households which suffered from diarrhoeal infections is
lower on average compared to the income of households which didn't suffered from ill-
health and diarrhoeal infections in the previous six month of the survey. This finding could
indicate that household incomes decreased through the burden of the diarrhoeal infection, or
that the household got impacted because of limited finances available. The fact is, with
regard to the medical poverty trap explained in chapter 3.4 by Whitehead et al. (2001), that
this finding indicates that ill-health is somehow related to poverty and low incomes. Also, it
was found out that there are no statistical associations or correlations between the total
disease related costs and the direct disposable household income. This means that low
income households suffer more from the burden of ill-health when seen from an economic
Additionally, after counting all the different expenses caused through the diarrhoeal
infection together, the results reveal, that the total rate of disease related expenses per episode
of diarrhoeal infection, compared to the total direct and monthly disposable household
income, makes up on average more than 20% of the total disposable household income. And
if counted together with the total costs for disease prevention methods, the total rate of
disease related expenses, compared to the total household income, makes up on average even
more than 30% of the total disposable household income. The financial burden caused
through ill-health is, when compared between the locations, slightly higher for the sub-urban
household. Supported by the comparisons made in chapters 5.4 and 6.3, this outcome
suggests again, that households located in slums are relatively more at risk to the financial
burden of ill-health. However, and as mentioned already in the previous chapter, as the study
analysed the disposable household income only, it may underestimates the consumption
levels of the rural poor and their ability for consumption smoothing. The researcher recons,
that there is a potential that the outcomes might very well be different when another measure
of household income would have been used.
In addressing the research question, we can now argue that diarrhoeal infections have
an enormous impact on household finances, in both, sub-urban and rural areas. With regard
to Prescott (1999) stated in chapter 1.2, a cost burden of more than 10% can be catastrophic
for households, therefore the results from this study indicate that diarrhoeal infections and ill-
health have a considerable potential to increase poverty among the people which are already
poor, regardless of the location.
9. Risk-economics and coping strategies at the household level
9.1 Introduction
The present chapter presents and analyzes the study findings with regard to the risk-
economics and coping strategies applied by the households in the sub-urban and rural
samples. The risk-economics and coping strategies of the surveyed households will be
analysed in section 9.2 in order to understand how individuals and households financially
manage the burden of ill-health, respectively, how they mitigate such burdens. Afterwards, in
section 9.3, on the basis of the survey outcomes, the findings will be discussed and then
9.2 Analysis of risk-economics and coping strategies
With regard to the findings made by Chima et al. (2002) and of Lucas et al. (1999) and stated
in chapter 3.3,the researcher analysed the risk-economics and coping strategies applied by the
households by the following criteria: inter-household labour substitution, engagement in
other labour, spending of savings, change of consumption patterns, sale of assets, and
borrowing of money. Subsequently, the questionnaire used within the survey contained one
question for each criterion mentioned.
The findings of the household survey reveal that most households in both rural and sub-
urban communities which have been financially impacted by ill-health through diarrhoeal
infections apply coping strategies. According to the survey, out of 42 households which have
been affected by at least one episode of diarrhoea, 28 households (67%) applied at least one
coping strategy to substitute for the economic burden caused. Furthermore, economic coping
strategies are strongly associated with ill-health and diseases by most households surveyed
and coping strategies are not experienced as an unusual phenomenon
Table 9.1 Range of coping strategies
Coping strategy
N = 27
N = 15
N = 42
labour substitution
Engagement in
other labour
Spending of
Change of
consumption
patterns
Sale of assets
Borrowing of
especially among the poor. As outlined in Table 9.1, 9.2, and 9.3, the most common coping
strategies at the household level are based on spending first the household savings, followed
by the sale of household assets, and by intra-household labour substitution. Usually,
households affected by ill-health use first their monetary/financial savings to compensate
medical treatment costs. Intra-household labour substitution is very common among rural
households, which is not surprising, as agricultural work can easily be transferred to another
person, respectively, household member.
Table 9.2 Household coping strategies 1
Location
Percentage of
Percentage of
Percentage of
affected
affected households
affected household
households
which engaged in
which spend extra
which substituted
other labour activities
savings to cope with
to cope with extra
extra costs
productive time
Sub-urban
15% 7% 70%
N = 27
53%
N = 15
All
34% 4.5% 72%
N = 42
Table 9.3 Household coping strategies 2
Location
Percentage of
Percentage of
Percentage of
affected households affected
affected
which changed
households which households which
consumption
sold household
borrowed money
patterns
Sub-urban
33%
N = 27
Rural
27% 40%
N = 15
All
N = 42
The least favourite coping strategies applied by disease impacted households are the
engagement in other labour activities, followed by a change of consumption pattern and
borrowing money. However, the engagement in other labour activities than normal is
conditioning on the availability of other labour opportunities.
According to the survey, household assets which have been most often sold are mainly
electronically goods like e.g. mobile phones or stereos.
Rural households have in terms of risk-management an advantage, as they are able to
produce and to trade their own agricultural products. According to observations and
interviews most rural households store parts of their harvest for iniquitous times. Moreover,
as the prices and profit-margins for agricultural products are subject to many different
indicators such as e.g. the weather or national inflation rates, some households store their
surplus until the prices reach the highest level. Often, this time is during or after disasters like
e.g. politically unstable situations or severe weather events. Though, this practise is as
already outlined a subject to seasonal variations and can not always be relied on.
9.3 Discussion and conclusion
The findings show, that almost all households which have been impacted by diarrhoeal
infections apply at least one kind of coping strategy, though, the range of coping strategies is
very diverse. Most households, in both, sub-urban and rural locations, used first their savings
to compensate for medical expenses. This behaviour is quite rational as most costs for
medical treatment and medication usually need to be paid relatively fast upon outbreak and
discovery of the infection. Therefore, it is most logical for impacted households to use the
money which they already have in their hands first.
Rural households also seem to prefer labour substitution, very much in contrast to sub-
urban households. But with regard to their main livelihood which is subsistence farming, and
with regard to the higher number of household members (see chapter 5), it is understandable
that this strategy is very effective in replacing the output of a lost productive household
member. In contrast, as agricultural work is less of importance, and as formal employment is
more common in urban places, it is more difficult to substitute for lost labour.
However, the rate of households which sold assets and which changed consumption
patterns was quite equal between both locations. It is very logical that households which have
only limited finances available are trying to turn non-monetary assets into monetary assets to
create the capital needed. In terms of risk-economies, assets like livestock or other valuable
possessions are a very good insurance against financial burdens. Furthermore, the strategy of
changing consumption patterns is a good method to save money before an episode of ill-
health as well as after. It is therefore a good method in terms of risk-economic and coping
With regard to the third sub-research question, which was enquiring how households
cope with the financial burden created by diarrhoeal diseases, we can now argue that in sub-
urban location households mainly prefer to spend savings followed by a strategy-mix of
changing consumption patterns, the sale of assets, and borrowing money from friends and
relatives. In contrast, rural households also spend their savings first, but then prefer labour
substitution, and the sale of assets such as e.g. livestock.
10. Discussion and Conclusion
10.1 Introduction
This chapter will discuss the findings and outcomes that were presented in the previous
chapters. The discussion here will focus on the assumptions and conclusions made in the
thesis's analysis. First, in section 10.2, the limitations of this study will be outlined to
highlight and justify the constraints and boundaries of this study and of the assumptions
made in the analysis. Secondly, the findings will be discussed and major assumptions will be
concluded in section 10.3. Lastly, recommendations for policies, the prevention of diarrhoeal
infections, and for the prevention of related economic burdens will be discussed in section
10.2 Study limitations
There have been several limitations within this study, mostly related to feasibility of the data
sampling process.
One major limitation was that most people who were affected by diarrhoeal infections
lived in districts in northern Uganda and along the Congolese border, which were due to
security issues not accessible for field research. And the fact that northern Uganda is
extremely insecure limited the research to the south-eastern part of the country. Furthermore,
the researcher would have been constrained to hire for almost every different part and district
of the country a different interpreter due to the researcher's inability to speak local tribal
languages. Also, large distances between major towns, bad roads which were almost non
existent, and the limitation of public transport to highly insecure motorbikes (boda bodas) or
over aged buses (matatatus) which drivers usually not even had a driving licence, made it
often a challenge to travel between places.
Another limitation was also the dependency on an interpreter, and on the permission for
data collection from the community leader or village chief. Though, the interpreter was very
helpful, data collection through an interpreter limits sometimes the accuracy of the results, as
data is sometimes interpreted differently or influenced by the interpreter's perceptions.
Additionally, not all community leaders or village chiefs were corporative, and some even
demanded a small "compensation" for their services, which created extra challenges for the
researcher, as he was not willing to pay for the access of scientific data. When the chief or
community leader was absent, or when he did not agreed with any data collection activities,
the researcher was forced to leave the community and to shift to a different place where data
collection was possible. Therefore, the process of surveying the sub-urban and rural
households was controlled by and depended on the community leader's or chief's courtesy.
The data collection methods needed also some adaptations as the originally planned
random household sample has been changed to a household sample which purposefully
allocated its targets, which means that it is difficult to generalise the results for the whole
community. Furthermore, the researcher planned originally to interview also patients affected
by diarrhoeal infections who were currently treated at local hospitals, as well as their caring
family members or friends who accompanied them, but due to the lack of permissions from
the medical facilities, and more importantly, due to the lack of privacy for interviews, this
was not possible.
The operationalisation of the term diarrhoeal disease, respectively the correct definition
or diagnoses of the pathogen responsible for the diarrhoeal infection was also not easy. The
issue was that most cases of diarrhoeal infections don't get properly diagnosed in a
laboratory due to the lack of finances and proper medical equipment. Most physicians can
only guess the reason for the infection based on symptoms, and apply a more general form of
treatment. This procedure is not always optimal, because it limits the validity of the
diagnosis, respectively, of the method of treatment. Therefore and as already outlined in
chapter 4.4, the researcher used the term diarrhoeal infection which is less specific and much
easier to operationalise in this circumstances.
Also, the collected data is limited and don't represents the situation for all of south-
eastern Uganda due to the relative small number of samples chosen. The study would have
been more representative if the researcher would have included a higher number of samples
of both sample units, but this was difficult due to the limited time frame.
Moreover, as it is very difficult to measure indirect household incomes like e.g. home farmed
groceries or home produced food, the comparisons and analysis based on household income
data is limited to the direct reported disposable household incomes only. Nevertheless, the
researcher is aware that the study's definition of the household income is a limitation.
However, the total income could be measured by transforming consumption expenditures and
patterns into some income measure.
Lastly, it could be argued that not all household members benefit or suffer equally from
the household income or its loss, respectively, not all household members suffer the same
burden inflicted by ill-health or by a given disease infection. The researcher takes this issue
into account, but makes clear that this study sees the household as one social and economic
unit as done in similar household and income surveys, and reminds that intra-household
issues are not of primary focus within this study.
10.3 Discussion and conclusion of assumptions made
The outlined and reviewed literature based on previous studies in this academic field
highlighted already the dramatic impacts of ill-health on the individual and household
economic level. It is argued by several academics and health experts, that good health is an
essential human capital, and also a major precondition for personal as well as for micro- and
macroeconomic development. Furthermore, good health conditions among a society are
dependent on the availability of livelihood assets to secure the generation of further human,
physical, and financial capitals (Obrist et al. 2007). But when livelihood assets are not
available and when people are impacted by ill-health and only spend assets and are not able
to replace them, then their economic situation will degrade continuously. And when
individuals and households are already weakened through the human and economic burden
caused by diarrhoeal infections, it will be even more difficult for them to reverse this
situation, as argued by Whitehead et al. (2001). Also, if too many households are threatened
by poverty through ill-health, the overall rate of development in a society will discretionary
To improve the original evidence and literature, the aim of this thesis was to investigate
and to analyse how exactly diarrhoeal infections economically impact individuals and
households in Uganda. After conducting a household survey and after collecting field data in
South-Eastern Uganda, the analysis clearly suggested that households which are impacted by
ill-health through diarrhoeal infections often suffer a large economic burden, mainly caused
by expenses for medical treatment and special food. Disease prevention costs can also
substantially decrease the household's financial stability and equity. On average, the direct
economic burden for households suffering from diarrhoeal infections and diseases is as high
as 20% of the total direct and monthly household income. And the costs for disease
prevention alone can be as high as 10% of the direct monthly household income. With regard
to the theoretical evidence and because the overall economic burden for households impacted
by diarrhoeal infections is on average above 10% (Prescott 1999), this study indicates that
diarrhoeal infections significantly impact households and their economic and financial
structures in many ways. Households are affected especially in their income and asset
spending behaviour, in their process of income and asset generation, and as well as in their
risk-economic abilities. The research question stated in this thesis can therefore be answered
with positivistic confidence, as the consequences for households impacted by diarrhoeal
infections were large financial casualties and income losses. However, as the study analysed
the disposable household income only, it may underestimates the consumption levels of the
rural poor and their ability for consumption smoothing. The researcher recons, that the
outcomes might very well be different when another measure of household income would
have been used. But as already justified in the study's limitations, it is not very easy to
calculate the value of (agrarian-) products that are non-disposable or gained through
subsistence farming.
Surprisingly, the rate of households suffering from infections with diarrhoeal infections
was much higher in suburban communities. It was originally assumed by the researcher that
it would be the way around and that rates of infections would be higher in rural areas as
indicated by the Uganda Demographic and Health Survey (Uganda Bureau of Statistics 2006a).
The researcher links these results to the observed fact that the environmental, living, and
sanitary conditions are much inferior in the suburban and urban slums compared to rural
villages. Also, another explanation could be, that the rate of HIV/Aids infections is much
higher in suburban and urban areas, and that one of the symptoms of this disease is diarrhoea.
The health seeking behaviour analysed revealed, that hardly any victims suffering from
diarrhoea in this part of Uganda used traditional or alternative medicine. And only a small
fraction of people consulted a pharmacy only. Subsequently, the findings indicated that most
people prefer professional medical treatment. However, most people in suburban areas
consult a public health facility, compared to rural areas, where most people consult private
health facilities. This could be explained by the fact, that according to the study's household
survey, the average incomes are slightly higher among rural households compared to the
household incomes in suburban slums. However, public health facilities are more common in
urban centres and often difficult to reach in rural areas. Nevertheless, private health facilities
and health facilities organised by religious or non-profit organisations are more concentrated
in remote places, which could explain why households located in rural areas consult more
private or semi-private health facilities.
The study was also able to find out, that to prevent or cope with an economic burden
caused by ill-health; most households surveyed applied a set of risk-economic and coping
strategies. The most common coping strategies applied by the households are based on labour
substitution, and spending household savings, and on a change in consumption patterns. The
study's findings indicate, that households affected by ill-health use first their monetary
savings to compensate medical treatment costs. The least favourite coping strategies applied
by disease impacted households are the engagement in other labour activities, followed by
borrowing money, and by the sale of household assets. These actions were justified by most
heads of households with the fact, that spending spare money and household savings as well
as changing consumption patterns for a limited period of time would impact the household's
abilities to cope with further economic burden less, than making financial debts or the selling
of valuable household investments and assets. Household and livelihood assets, like e.g.
livestock, are often seen as a kind of insurance in terms of risk-economic strategy, and they
shouldn't be sold off too quickly.
The researcher looked as well for associations and correlations between the different
indicators and variables used in the survey, and suspected relations between the rate of
disease infection, between disease prevention measures, between the household locations,
and the direct household income. But after applying chi-square tests, and regression and
scatter plot analysis, these assumptions could be rejected with the results that there is no clear
association or correlation between these indicators and variables. Though, the scatter plot
analysis revealed that wealthier households tend to be slightly less impacted by diarrhoeal
disease even if they are spending on average less on disease prevention methods. And most
of these wealthier households are based outside the suburban slums in rural communities.
These finding could be interpreted by the assumption, that wealthier households can
usually afford better living and sanitation standards. Moreover, even if the general disposable
household income in rural areas would be as low as in the slums, the environmental and
sanitary conditions in most rural communities are much better and therefore result in a
correspondingly lower infection rate with diarrhoea causing diseases. For example, the
cholera epidemic in the year 2000 in Durban (South Africa) clearly demonstrated that even if
sufficient sanitation facilities like pit latrines are installed in the townships, the risk of
infections isn't lowered when the concentration of latrines and of people using them is to
high (Koenig 2008). However, one should not forget, that the prevalence of diarrhoea causing
pathogens is not necessarily related to wealth but to the standard of sanitation and hygiene.
Most of the study's findings highlight in a similar way that ill-health has a serious
impact on people's finances and on poverty as presented by findings of previous studies
conducted in this field and mentioned in the theory; though their sample units were larger in
size and often more representative. The coping and prevention methods applied by the
interviewed households, respectively their impacts, were also very similar to the household
reactions studied by for example McIntyre et al. 2006; Chima et al. 2003; Russel et al. 2004,
in other Sub-Saharan African countries. But even if the average economic burden for
households is above 10% of the direct household income, the overall economic damage
caused by these economic impacts must be seen differently compared to economic burdens
caused by other infectious (e.g. Aids) and non-infectious diseases (e.g. cancer and diabetes),
because the majority of diarrhoeal infections usually do not last very long, and most victims
are children. Nevertheless, general assumptions about the impact of health costs can not be
made in this study, as the number of samples studied was relatively low, and due to the fact
that ill-health and related costs are defined through many different variables and indicators,
like e.g. different forms of diseases, therapies, or health perceptions, which make it difficult
to state definite assumptions. Therefore, further conclusions should not be drawn without
additional information and research conducted in this field. However, this study can be an
indicator and a stimulator for further research in this field and in this geographic region, and
it helps to get an idea about the impact of infectious diseases.
Subsequently, as diarrhoeal diseases are still one of the major causes for overall
morbidity and death in Sub-Saharan Africa, actions and interventions on all levels are
urgently needed to improve the health and economic status of Africa's people.
10.4 Recommendations
The suggestions for improvement of the current situation in Uganda focus mainly on the
prevention of diarrhoeal diseases and of ill-health in general. Also, the researcher recons that
children must get special attention and treatment to combat the cycle of ill-health and
poverty. One step forward could be to launch more vaccination campaigns which could help
to lower the rate of new infections with diarrhoeal diseases, as new vaccines become
approved. For example, several studies conducted in South-East Asia proved that the
vaccination of children against the infections with the rotavirus is very cost-effective to
combat the economic burden caused by diarrhoea causing diseases (Podewils et al. 2005;
Fischer et al. 2005).
However, the most effective and sustainable measures to decrease the rates of new
infections and therefore of ill-health are the installation of efficient water and sanitation
facilities, the improvement of existing sewerage systems and of wastewater treatment plants,
followed by the education of especially women and children about personal and general
sanitation and hygiene (Hutton et al. 2004).
With regards to Uganda's policy structure, there still seems to be a gab when it comes
to cost-recovery. As mentioned in chapter 2, some patients need to consult private health
facilities if they are nearer by, or require additional treatment that cannot be provided by the
public health sector, which creates extra cost. Also, medication and drugs are not always
provided for free under the National Health Policy (1999), and there is no system to
compensate for lost productive labour time such as a national health insurance, though the
Ugandan government is aware of the issue and plans for a national insurance scheme are
going ahead. Such interventions would also bring benefits to the Ugandan macro-economy
and would therefore support the overall development of the country.
Moreover, health interventions should also focus more on ill-health and disease
prevention to tackle the issue at its roots. Though, some NGOs and organisations are already
busy in this field but not all communities and people can be reached yet. Disease prevention
is often regarded as more cost-effective compared to disease treatment and eradication
measures. For example, a very sustainable and newly emerging prevention measurement is
the instalment of urine-diversion latrines (UDs) which separate urine and faeces and
therefore allow faster decomposition of sewage. This technique could be a real improvement
for crowded urban slums which have a high density of pit latrines (Koenig 2008). In contrast,
another emerging prevention measurement is the Community-Led Total Sanitation approach
(CLTS) which concentrates on a change in sanitation behaviour through community
participation rather than constructing only pit latrines. This approach concentrates on the
whole community rather than on individual behaviours, and the collective benefit from
stopping open defecation can encourage a more cooperative approach. People decide together
how they will create a clean and hygienic environment that benefits everyone (WATSAN
2008). In any way, the research conducted through this study can help to further adjust the
policy framework and to give further recommendations for policy building.
Currently, the coverage of the supply of safe drinking water in Uganda is between 56%
and 62%, but the Ugandan government plans (in accordance with the Millennium
Development Goals) to supply safe access to drinking water to all Ugandans by the year
2015. As the lack of safe drinking water correlates with the rate of diarrhoeal infections, and
as they again correlate with economic burdens at all levels, actions to combat this cycle are
vital and need to be taken urgently. However, this goal can only be achieved if changes and
improvements in the infrastructure and water sector occur fast, and if all parties are included
in this development process.
I am especially thankful to my mother, who emotionally and financially supported this study,
and I also want to thank my grandparents who gave financial support too.
Special thanks go also to the Makerere University's School of Public Health and to my
local field supervisor Dr. Sebastian Olikira Baine, without whom the study would have been
difficult to realise.
And I want to thank my local interpreter Arinaitwe Euzobio, who confidentially
translated my interviews and navigated me around the slums and villages.
Finally, I would like to thank all individuals, households, and experts who supported
my research and interviews, and who supported me with relevant data, for their help.
References
Agich, G. and C. Begley (eds.) (1986). The price of health. D. Reidel Publishing Company, Dordrecht. AMREF – Our work in Uganda www.amref.org/where-we-work/our-work-in-uganda/ (visited on 20 September 2008) Auswärtiges Amt (2008). Reise- und Sicherheitshinweise – Uganda. www.auswaertiges-amt.de/diplo/de/Laenderinformationen/Uganda/Sicherheitshinweise.htm (visited on 17 March 2008) Bleakley, H. (2007). Disease and development: evidence from hookworm eradication in the American South, in The Quarterly Journal of Economics, Vol. 122, No. 1, pp. 73-117. Bibi, S. (2005). Measuring poverty in a multidimensional perspective: a review of literature. PMMA Working Paper 2005-7. University of Tunis. Breyer, F., P. Zweifel, and M. Kifmann (2005). Gesundheits-ökonomik (5th Edition). Springer-Verlag, Berlin. Chima, R., C. Goodman, and A. Mills (2003). The economic impact of malaria in Africa: a critical review of the evidence, in Health Policy, Vol. 63, pp. 17-36. CIA Factbook – Uganda www.cia.gov/library/publications/the-world-factbook/geos/ug.html (visited on 20 January 2008) Christiaensen, L. and K. Subbarao (2005). Towards an understanding of household vulnerability in rural Kenya, in Journal of African Economics, Vol. 14, No. 4, pp. 520-558. Crotty, M. (1998). The foundation of social research: meaning and perspectives in the research process. Sage, London. DANIDA – Danish International Development Agency www.danidadevforum.um.dk/NR/rdonlyres/993143D3-108B-4162-AF57-EBDBDFA74318/0/Ugandapaper.doc (visited on 14 January 2009) Deaton, A. (2001). Counting the world's poor: problems and possible solutions, in The World Bank Observer, Vol. 16, No. 2, pp. 125-147. Dercon, S. (2002). Income risk, coping strategies, and safety nets, in The World Bank Research Observer, Vol. 17, No. 2, pp. 141-166. Devereux, S. (2001). Livelihood insecurity and social protection: a re-emerging issue in rural development, in Development Policy Review, Vol. 19, No. 4, pp. 507-519. DFID (2000). Better health for poor people – strategies for achieving the international development targets. Department for International Development, London.
DWD – Directorate of Water Development – Policy and legal Framework www.dwd.co.ug/default2.php?active_page_id=321 (visited on 14 January 2009) Feachem, R., T. Kjellstrom, C. Murray, M. Over, and M. Phillips (1992). The health of adults in the developing world (eds.). Oxford University Press, New York. Feachem, R., M. McGarry, and D. Mara (1986). Water, wastes and health in hot climates. John Wiley and Sons Ltd., Chichester. Fischer, T., Dang Duc Anh, L. Antil, N. Cat, P. Kilgore, V. Thiem, R. Rheingans, H. Tho, R. Glass, and J. Bresee (2005). Health care costs of diarrhoeal diseases and estimates of the cost-effectiveness of rotavirus vaccination in Vietnam, in The Journal of Infectious Diseases, Vol. 192, No. 15, pp. 1720-1726. Folland, S. and S. Miron (2007). The economics of health and health care (5th edition). Pearson Prentice Hall, New Jersey. Garg, A. and Morduch, J. (1998). Sibling rivalry and the gender gab: evidence from child health outcomes in Ghana, in Journal of Population Economics, Vol. 11, No. 4, pp. 471-493. GISed – geographical information maps, cholera map www.gised.com.au/maps/cholera-05.gif (visited on 14 August 2008) Grossman, M. (1972). On the concept of health capital and the demand for health, in The Journal of Political Economy, Vol. 80, No. 2, pp. 223-255. Haddad, L. and Reardon, T. (1993). Gender bias in the allocation of resources within households in Burkina Faso: a disaggregated outlay equivalent analyses, in The Journal of Development Studies, Vol. 29, No. 2, pp. 260-276. Hotez, P., S. Brooker, J. Bethony, M. Bottazi, A. Loucas, and S. Xiao (2004). Hookworm infections, in The New England Journal of Medicine, Vol. 351, No. 8, pp. 799-807. Human Rights Watch – News http://hrw.org/english/docs/2003/03/28/uganda5451.htm (visited on 25 May 2008) Hunter, J., L. Rey, K. Chu, E. Adekolu-Jhon, and K. Mott (1993). Parasitic disease in water resource development – the need for intersectional negotiation. WHO, Geneva. Hutton, G. and L. Haller (2004). Evaluation of the costs and benefits of water and sanitation improvements at the global level. World Health Organization, Geneva. Intergovernmental Panel on Climate Change (2007). Working Group 2 Report: Impacts, Adaptations, and Vulnerability. Geneva. IRC – International Water and Sanitation Centre, Uganda www.irc.nl/page/3294 (visited on 14 January 2009) Klasen, S. (2000). Measuring poverty and deprivation in South Africa, in Review of Income and Wealth, Vol. 46, No. 1, pp. 33-58.
Koenig, R. (2008). Durban's poor get water service long denied, in Science, Vol. 319, No. 8, pp. 744-746. Lloyd, C. and Gage-Brandon, A. (1993). Woman's role in maintaining households: family welfare and sexual inequality in Ghana, in Population Studies, Vol. 47, No. 1, pp. 115-131. Lucas, H. and A. Nuwagaba (1999). Household coping strategies in response to the introduction of user charges for social services: a case study on health in Uganda. IDS Working Paper 86. Institute of Development Studies, UK. Lwanga-Ntale, C. and K. McClean (2003). The face of chronic poverty in Uganda as seen by the poor themselves. Conference paper. Chronic Poverty Research Centre, Kampala. McIntyre, D., M. Thiede, G. Dahlgren, and M. Whitehead (2006). What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts?, in Social Science & Medicine, Vol. 62, pp. 858-865. Milanovic, B. (2002). True world income distribution, 1998 and 1993: first calculation based on household surveys alone, in The Economic Journal, Vol. 112, No. 476, pp. 51-92. Morris, S., Carletto, C., Hoddinott, J., and Christiaensen, L. (2000). Validity of rapid estimates of household wealth in income for health surveys in rural Africa, in Journal of Epidemiological Community Health, Vol. 54, No. 12, pp. 381-387. Moss, N. (2002). Gender equity and socioeconomic inequality: a framework for the patterning of women's health, in Social Science & Medicine, Vol. 54, No. 5, pp. 649-661. Mukherjee, C., H. White, and M. Wuyts (1998). Econometrics and data analysis for developing countries. Routledge, London. Mukhopadhyay, A. and A. Krishna-De (2005). Perspectives in environmental health – vector and water borne diseases. Originals, Delhi. Murray, C., D. Evans, A. Acharya, and R. Baltussen, (2000). Development of WHO guidelines on generalized cost-effectiveness analysis, in Health Economics, Vol. 9, No. 3, pp. 235-251.
Naldoo, A. and K. Patric (2002). Cholera: a continuous epidemic in Africa, in The Journal of The Royal Society for the Promotion of Health, Vol. 122, No. 2, pp. 89-94. Nelson, M.A. (1994). Economic impoverishment as a health risk: methodologic and conceptual issues, in Advances in Nursing Science, Vol. 16, No. 3, pp. 1-12. Obrist, B., N. Iteba, C. Lengeler, A. Makemba, and C. Mshana (2007). Access to health care in contexts of livelihood insecurity: a framework for analysis and action, in Plos Medicine, Vol. 4, No. 10, pp. 1584-1588. Osmani, S. and Sen, A. (2003). The hidden penalties of gender inequality: foetal origins of ill-health, in Economics and Human Biology, Vol. 1, No. 1, pp. 105-121.
Philipson, T. (1999). Economic epidemiology and infectious diseases. US National Bureau of Economic Research Working Paper 7037. Cambridge, MA. Podewils, L., L. Antil, E. Hummelman, J. Bresee, U. Parashar, and R. Rheingans (2005). Project cost-effectiveness of rotavirus vaccination for children in Asia, in The Journal of Infectious Diseases, Vol. 192, No. 15, pp. 133-145. Prescott, N. (1999). Coping with catastrophic health shocks. Conference on social protection and poverty. Inter American Development Bank, Washington, DC. Republic of Uganda – Ministry of Finance, Planning and Economic Development www.finance.go.ug/docs/PEAP%202005%20Apr.pdf (visited on 14 January 2009) Republic of Uganda – 1995 Water Statute http://faolex.fao.org/docs/pdf/uga5251.pdf (visited on 14 January 2009) Russell, S. (2004). The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome, in American Journal of Tropical Medicine and Hygiene, Vol. 71, No. 2, pp. 147-155. Sachs, J. and P. Malaney (2002). The economic and social burden of malaria, in Nature, Vol. 415, No. 7, pp. 680-685. Sack, D., R. Sack, G. Nair, and A. Siddique (2004). Cholera, in The Lanced, Vol. 363, No. 9404, pp. 223-233. Sahn, D.E. and Stifel, D.C. (2000). Poverty comparisons over time and across countries in Africa, in World Development, Vol. 28, No. 12, pp. 2123-2155. Sauerborn, R., A. Adamas, and M. Hien (1996). Household strategies to cope with the economic costs of illness, in Social Science & Medicine, Vol. 43, No. 3, pp. 291-301. Sauerborn, R., Bergman, P., Nougtara, A. (1996). Age bias, but no gender bias, in the intra-household resource allocation for health care in rural Burkina Faso, in Health Transition Review, Vol. 6, pp. 131-145. Schultz, T.W. (1961). Investment in human capital, in The American Economic Review, Vol. 51, No. 1, pp. 1-17. Shapiro, M., M. Otieno, P. Adock, P. Phillips-Howard, W. Hawley, L. Kumar, P. Waiyaki, L. Nahlen, and L. Slutsker (1999). Transmission of epidemic Vibrio Cholerae 01 in rural Western Kenya associated with drinking water from Lake Victoria: an environmental reservoir for cholera?, in The American Society of Tropical Medicine and Hygiene, Vol. 60, No. 2, pp. 271-276. Sorkin, A.L. (1976). Health economics in developing countries. Lexington Books, Massachusetts. Statistics South Africa (2000) Measuring poverty in South Africa. Pretoria.
Statistics South Africa – Income and Expenditure Survey 2005/2006 www.statssa.gov.za/ies/faq.asp (visited on 20 January 2008) Su, T., Kouyate, B., Flessa, S. (2006). Catastrophic household expenditures for health care in a low-income society: a study from Nouna District, Burkina Faso, in Bulletin of the World Health Organisation, Vol. 84, No. 1, pp. 21-28. The Economist - Microeconomics www.economist.com/research/Economics/searchactionterms.cfm?query=microeconomics (visited on 20 January 2008) Uganda Bureau of Statistics (2006a). Uganda Demographic and Health Survey 2006. Kampala. Uganda Bureau of Statistics (2006b). Uganda National Household Survey 2005/2006. Kampala. Uganda Ministry of Health (2005). Health Sector Strategic Plan 2 (HSSP 2). Kampala, Uganda. Uganda Ministry of Health – Health infrastructure www.health.go.ug/health_units.htm (visited on 20 February 2008) UN-Water – World Water Assessment Programme (2006) http://unesco.unesco.org/images/0014/001467/146760e.pdf (visited on 14 January 2009) WaterAid UK – Diarrhoeal diseases www.wateraid.org/uk/what_we_do/the_need/disease/684.asp (visited on 10 December 2007) WATSAN Resource Centre Uganda – Facts and Figures www.watsanuganda.watsan.net/page/280 (visited on 08 September 2008) WATSAN Resource Centre Uganda – Ecological Sanitation www.watsanuganda.watsan.net/page/264 (visited on 08 May 2008) Weisbrod, BA., R. Andreano, R. Baldwin, E. Epstein, A. Kelley, and T. Helminiak (1973). Disease and Economic Development – the impact of parasitic diseases in St. Lucia. The University of Wisconsin Press, Wisconsin. Weisbrod, B.A. (1961). Economics of public health – measuring the economic impact of disease. University of Pennsylvania Press, Philadelphia. Whitehead, M., G . Dahlgren , and T . Evans (2001). Equity and health sector reforms: can low-income countries escape the medical poverty trap?, in The Lancet, Vol. 358, pp. 833-836. Wiesmann, D. and J. Jutting (2000). The emerging movement of community based health insurances in Sub-Saharan Africa: experienced and lessons learned, in Africa Spectrum, Vol. 35, No. 2, pp. 1-19.
WHO – Water-related diseases, typhoid www.who.int/water_sanitation_health/diseases/typhoid/en/ (visited on 30 June 2007) WHO – Diarrhoea fact sheet www.who.int/topics/diarrhoea/en/ (visited on 20 January 2008) WHO – Action Against Worms Issue 3 2002. www.who.int/wormcontrol/en/action_against_worms.pdf (visited on 01 July 2007) WHO (2002). Improving health outcomes of the poor. The Report of Working Group 5 of the Commission on Macroeconomics and Health. World Health Organization, Geneva. WHO (1996). The World Health Report 1996 – Fighting disease, fostering development. World Health Organisation, Geneva. WHO (1990). A manual for the treatment of diarrhoea for physicians and health workers. WHO/CDD/SER/80.2 Rev 2. Geneva. WHO & UNICEF (2006). Joint monitoring programme for water supply and sanitation. www.wssinfo.org/pdf/country/UGA_wat.pdf (visited on 21 October 2009)
List of Abbreviations
AMREF: African Medical and Research Foundation
CBA: Cost-benefit analysis
CBHI: Community based health insurance scheme
CEA: Cost-effectiveness analysis
CLTS: Community-Led Total Sanitation Approach
CIA: Central Intelligence Agency
DFID: Department for international development
DWD: Directorate of Water Development
EAC: East African Community
EHD: Environmental Health Division
HPAC: Health Policy Advisory Committee
LDC: Less developed country
IDP: Internally displaced people
MDG: Millennium Development Goals
NGO: Non-governmental organisation
NWSC: National Water and Sewage Corporation
ORS: Oral rehydration solution
ORT: Oral rehydration therapy
PEAP: Poverty Eradication Action Plan
PHP: Private health practitioners
PNFP: Private-non-for-profit organisation
SSA: Sub-Saharan Africa
TCMP: Traditional and Complementary Medicine Practitioners
UD: Urine-diversion
UGX: Ugandan Shilling
UNCST: Uganda Council of Science and Technology
UNICEF: United Nations International Children's Fund
UWASNET: Uganda Water and Sanitation Network
WATSAN: Water & Sanitation Resource Centre
WHO: World Health Organisation
WSSWG: Water and Sanitation Sector-Working Group
Appendices
Household questionnaire
Survey about the microeconomic impact of diarrhoeal diseases on rural and
sub-urban households in Uganda
This survey questionnaire will support the research for a graduate thesis, which is supervised by the University of Amsterdam in Holland. The aim of this survey is to improve the scientific understanding of the (micro-) economic impacts caused by diarrhoeal diseases on individuals and households.
The collected information will be treated confidentially and will only be used for
scientific purposes by the researcher. Furthermore, the collected information will
not be passed on to a third party.
Gender:
Male � Female �
Age:
15 – 35 � 36 – 60 � 61+ �
Permanent location of the individual or household interviewed: ………………….
Rural � Sub-urban � Urban � Refugee camp �
1. How many people in total belong to your household?
Please state the number of household members:
2. How many of these household members are female?
Please state the number of household members:
3. How many of the total household members are below the age of 12 years?
Please state the number of household members:
4. Are you physically or financially supporting and contributing to a household?
Yes � No � If yes, please specify your contribution: …………….
5. How many household members are physically or financially supporting and
contributing to your household?
Please state number of household members:
6. Have you, or a member of your household, recently (in the past 6 month) been
affected by an infection causing symptoms of diarrhoea, or watery or bloody
stool?
Yes � No �
7. If yes, how many episodes of symptoms of diarrhoea, or watery or bloody stool
occurred in the household in the past 6 month?
Please state the frequency of episodes:
8. If yes, do you know what kind of disease caused the symptoms of diarrhoea,
respectively, was the disease professionally diagnosed?
If professionally diagnosed, please state the cause for the diarrhoea: …………………
9. Did you, or the effected household member, took up any medical treatment from
a doctor or in a hospital to reduce the health impact of the disease?
Yes � No �
10. Did you, or the effected household member, took up any traditional or
alternative treatment to reduce the health impact of the disease?
Yes � No �
(If no professional medical or traditional treatment has been applied, please go to
question 17)
11. How much time in total did you, or the effected household member, spend for
medical examination and treatment, including for the return transportation?
< 6 hours � > 6 hours � > 12 hours � > 24 hours � > 48 hours �
12. Have you, or the effected household member, been accompanied by another
household member when you took up medical or traditional treatment?
Yes � No �
13. How much money did you, or the effected household member, spend for the
transport to the doctor?
Please state the amount in Ugandan shilling (UGX):
14. Was the doctor or medical facility private or public?
Private � Public �
15. How much money did you, or the effected household member, spend for the
treatment and/or for the hospitalisation?
Please state the amount in Ugandan shilling (UGX):
16. How much money in total did you, or the effected household member, spend
for medication (including traditional medication) to treat the infection and the
diarrhoea?
Please state the amount in Ugandan shilling (UGX):
17. How much is the total household income on average per month?
Please state the amount in Ugandan shilling (UGX):
18. How much money are you, or the infected household member, earning per
week?
Please state the amount in Ugandan shilling (UGX):
19. Did you, or the effected household member, required special food due to the
impact of diarrhea and ill-health?
Yes � No �
20. If yes, how much extra money did you, or the effected household member,
spend for the special food during the entire time period of ill-heath?
Please state the amount in Ugandan shilling (UGX):
21. Did a member of your household recently (in the past 6 month) died as a
result of an infection causing symptoms of diarrhoea?
Yes � No �
22. If yes, how much money did you, or the household, spend for the funeral
costs?
Please state the amount in Ugandan shilling (UGX):
23. Did household or family members needed to substitute for lost productive time
due to your, or your household member's, infection with a diarrhoeal infection?
Yes � No �
24. Did you, or the effected household member, needed to engage in labour
activities other than your normal work, to cope with the extra costs caused by
the diarrhoeal infection?
Yes � No �
25. Did you, or the effected household member, needed to spend any extra
savings to cope with the extra costs caused by the diarrhoeal infection?
Yes � No �
26. Did you, or the entire household, needed to change any consumption patterns,
due to the extra costs caused by the diarrhoeal infection?
Yes � No �
27. Did you, or the household community, needed to sell any (household) assets
like livestock or property, to cope with the extra costs caused by the diarrhoeal
infection?
Yes � No �
28. Did you, or the effected household member, needed to borrow money to cope
with extra costs caused by the diarrhoeal infection?
Yes � No �
29. Do you, or the household, apply any methods or techniques to prevent
infections and ill-health?
If yes, please specify the prevention methods or techniques: …………………………
30. How much money do you spend per month for any disease prevention
methods or techniques?
Please state the amount in Ugandan shilling (UGX):
Thank you very much for supporting my research and for completing this
questionnaire!
Source: http://www.wasser-wissen.de/linklisten/masterarbeiten/M%20Sc%20%20Thesis%20-%20IDS%20Bastian%20Schnabel.pdf
helping dental patients to quit tobacco Dh INFORMAtION READER bOx Partnership Working Document Purpose Best Practice Guidance Gateway Ref: 8177 Smoking cessation guidance for primary care dental teams Publication Date General Dental Practitioners Circulation List PCT CEs, Directors of PH Guidance to GDPs on the contribution that dental teams can make to smoking cessation
28 February 2016 Issue No. 2016/02A PATENTS JOURNAL BRUNEI DARUSSALAM Brunei Darussalam Intellectual Property Office (BruIPO) The Brunei Economic Development Board 4th Floor Block 2D, Jalan Kumbang Pasang Bandar Seri Begawan BA1311 Negara Brunei Darussalam Tel: +673 223 0111 │Fax: +673 238 0545 Email:website: www.brunei-patents.com.bn Brunei Darussalam Intellectual Property Office (BruIPO) © 2013. All rights reserved. Modification or reproduction of this Journal without the permission of BruIPO is prohibited.