Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Druck







DIABETES
PEPTIDES
Peptides and Diabetes
PEPTIDES FOR
DIABETES RESEARCH
According to data from the International Diabetes Federa-tion, more than 250 million people around the world suf-fer from diabetes mellitus, a chronic metabolic disorder characterized by hyperglycemia. Diabetes mellitus can be divided into two main types, type 1 or insulin-dependent diabetes mellitus (IDDM) and type 2, or non insulin-depen-dent diabetes mellitus (NIDDM). The absolute lack of insu-lin, due to destruction of the insulin producing pancreatic β-cells, is the particular disorder in type 1 diabetes. Type 2 diabetes is mainly characterized by the inability of cells to respond to insulin. The condition affects mostly the cells of muscle and fat tissue, and results in a condition known as „insulin resistance".
means ‘to fl ow through'. The adjective mel-
Diabetes was already known in ancient
litus, which comes from Latin and means
times. The name of this disease was created
‘honey-sweet', was added by the German
by the Graeco-Roman physician Aretaeus
physician Johann Peter Frank (1745-1821).
of Cappadocia (approx. 80 - 130 AD) and is
It was introduced in order to distinguish di-
derived from the Greek word diabainein that
abetes mellitus, also called ‘sugar diabetes', from diabetes insipidus, where an exces-sive amount of urine is produced as a result of a disturbance of the hormonal control of reabsorption of water in the kidneys. In 1889, pancreatic secretions were shown
EFFECTS OF
to control blood sugar levels. However, it took another 30 years until insulin was
purifi ed from the islets of Langerhans. In the following 50 years scientists detected
Over time, diabetes mellitus can lead
the system-wide effects of insulin in liver,
to blindness, kidney failure, and nerve
muscle, and adipose tissues. In the 1970s,
damage. Diabetes mellitus is also an
the insulin receptor was discovered, and 10
important factor in accelerating the
years later, its tyrosine kinase activity was
hardening and narrowing of the arter-
demonstrated. Despite this steady prog-
ies (atherosclerosis), leading to stroke,
ress, one of the most challenging health
coronary heart diseases, and other
problems of the 21st century remains the
blood vessel disorders.
dramatic increase in diabetes mellitus that
is occurring throughout the world. Today
fi de bridge) linked by two disulfi de bridges
Glucose homeostasis
diabetes mellitus is one of the main causes
to a B-chain of 30 amino acids. β-Cells
is accomplished by
of death in most developed countries.
secrete insulin in response to a rising level
complex physiological
mechanisms. Control
According to data from the International
of circulating glucose. The normal fasting
of blood glucose levels
Diabetes Federation, more than 250 mil-
blood glucose concentration in humans and
involves insulin, gluca-
lion people around the world suffer from
most mammals is 80 to 90 mg per 100 ml,
gon and other peptide
diabetes and this number will grow to more
associated with very low levels of insulin
hormones such as
than 380 millions by 2030. Further 300
secretion. After a meal, excess sugars must
glucagon-like peptide
million people have impaired glucose toler-
be stored so that energy reserves will be
1 (GLP-1) and glucose-
ance, a condition that can signal oncoming
available later on. Excess glucose is sensed
dependent insulinotro-
pic polypeptide (gastric
diabetes. More than 90% of the diabetics
by β-cells in the pancreas, which respond
inhibitory polypeptide
have type 2 diabetes, a chronic disease as-
by secreting insulin into the bloodstream.
sociated with insulin defi ciency and insulin
Insulin causes various cells in the body to
resistance. Complications seen with diabe-
store glucose (see Fig. 1):
tes range from heart disease (2 to 4 times
• Insulin stimulates skeletal muscle fi bers
higher occurence than in non-diabetics)
to convert glucose into glycogen. It also in-
to blindness, kidney disease, amputations,
duces the synthesis of proteins from amino
nerve damage and erectile dysfunction.
acids circulating in the blood.
As obesity spreads, the number of type 2
• Insulin acts on liver cells. It stimulates
diabetics rises. Over 80% of diabetics are
them to take up glucose from the blood
obese. Consequently, the treatment of risk
converting it into glycogen while inhibiting
factors such as obesity, hypertension, and
the production of the enzymes involved in
hyperlipidemia assumes major impor-
tance and must be coordinated with a good
• Insulin acts on fat cells to stimulate the
glycemic control for the reduction in total
uptake of glucose and the synthesis of fat.
mortality in type 2 diabetes mellitus. In this
In each case, insulin triggers these effects
monograph, we describe the pancreatic and
by binding to the insulin receptor, a hetero-
gastrointestinal peptide hormones that are
tetramer of two extracellular α-subunits
involved in the control of blood glucose, the
that are bonded by disulfi des to two trans-
classifi cation, and the treatment of diabe-
membrane β-subunits. Insulin receptor
tes mellitus.
activation leads to specifi c phosphorylation events followed by an increase in glucose
Pancreatic Peptide Hormones
storage and a concomitant decrease in
The islets of Langerhans contain four main
hepatic glucose release.
cell types: β-cells secreting insulin, α-cells
C-Peptide is applied as a diagnostic tool. It
secreting glucagon, δ-cells secreting
is released in amounts equal to insulin, so
somatostatin and γ-cells secreting pancre-
the level of C-peptide in the blood indicates
atic polypeptide (PP). The core of each islet
how much insulin is being produced by the
contains mainly the β-cells surrounded
pancreas. The concentration of C-peptide is
by a mantle of α-cells interspersed with
measured in diabetics to differentiate be-
δ-cells or γ-cells. Insulin is synthesized as a
tween endogenous (produced by the body)
preprohormone in the β-cells of the islets of
and exogenous (injected into the body)
Langerhans. Removal of its signal peptide
insulin, since synthetic insulin does not
during insertion into the endoplasmic retic-
contain the C-peptide. Inappropriate use
ulum generates proinsulin which consists
of insulin in persons with a low blood sugar
of 3 domains: an amino-terminal B-chain, a
level results in a low C-peptide level. The
carboxy-terminal A-chain and a connecting
C-peptide level can also be determined in
peptide known as C-peptide. Within the en-
patients with type 2 diabetes showing how
doplasmic reticulum proinsulin is exposed
much insulin is produced by the β-cells.
to several specifi c endopeptidases. These
Abnormal high amounts of C-peptide can
enzymes excise the C-peptide, thereby
indicate the presence of a tumor called
generating the mature form of insulin, a
insulinoma which secretes insulin.
small protein consisting of an A-chain of 21
β-Cells also secrete a peptide hormone
amino acids (containing an internal disul-
known as islet amyloid polypeptide (IAPP)
Peptides and Diabetes
Promotes insulin release
Stimulates breakdown of glycoge
Stimulates formation of glycogen
Stimulation of glucose uptake
from blood
Tissue cells
(muscle, kidney, fat)
Opposing effects of
insulin and glucagon
or amylin. This 37 amino acid peptide is
Fig. 1). It counterbalances the action of in-
structurally related to calcitonin and has
sulin, increasing the levels of blood glucose
weak calcitonin-like effects on calcium
and stimulating the protein breakdown
metabolism and osteoclast activity. Amylin
in muscle. Glucagon is a major catabolic
shows about 50% sequence identity with
hormone, acting primarily on the liver. The
calcitonin gene-related peptide (CGRP). It is
peptide stimulates glycogenolysis (glycogen
stored together with insulin in the secre-
breakdown) and gluconeogenesis (syn-
tory granules of β-cells and is co-secreted
thesis of glucose from non-carbohydrate
with insulin. Amylin's most potent actions
sources), inhibits glycogenesis (glycogen
include the slowing of gastric emptying and
synthesis) and glycolysis, overall increas-
the suppression of postprandial glucagon
ing hepatic glucose output and ketone body
secretion. The hormone also reduces food
formation. In people suffering from diabe-
intake and inhibits the secretion of gastric
tes, excess secretion of glucagon plays a
acid and digestive enzymes.
primary role in hyperglycemia (high blood
Thus, there is therapeutic potential of IAPP
glucose concentration). Glucagon is clini-
agonists for the treatment of patients with
cally used in the treatment of hypoglycemia
absolute amylin defi ciency (type 1 diabe-
in unconscious patients (who can't drink).
tes) or relative amylin defi ciency (type 2
Somatostatin release from the pancreas
and gut is stimulated by glucose and amino
In addition, amylin is the major component
acids. In diabetes, somatostatin levels are
of the pancreatic amyloid deposits occur-
increased in pancreas and gut, presum-
ring in the pancreas of patients with type 2
ably as a consequence of insulin defi ciency.
Somatostatin inhibits secretion of growth
Glucagon secretion is stimulated by low,
hormone, insulin and glucagon.
and inhibited by high concentrations of glucose and fatty acids in the plasma (see
Gastrointestinal Peptide Hormones
Glucose-dependent insulinotropic poly-
peptide (GIP) and glucagon-like peptide 1 (GLP-1) have signifi cant effects on insulin secretion and glucose regulation. They are
Post-translational
released after ingestion of carbohydrate-
and fat-rich meals and stimulate insulin se-cretion postprandially. Both gut hormones constitute the class of incretins and share considerable sequence homology. GIP is a
single 42 amino acid peptide derived from a larger 153 amino acid precursor (see Fig. 2).
The peptide was originally observed to inhibit gastric acid secretion (hence it was
the circulating GLPs.
Fig. 2.
Structure of prepro-GIP
designated gastric inhibitory polypeptide).
The primary physiological responses to
Subsequent studies have demonstrated po-
GLP-1 are glucose-dependent insulin
tent glucose-dependent insulin stimulatory
secretion, inhibition of glucagon secretion
effects of GIP administration in dogs and
and inhibition of gastric acid secretion and
rodents. GIP also regulates fat metabolism
gastric emptying. All effects of GLP-1 are
in adipocytes, including stimulation of lipo-
exerted by activation of the GLP-1 receptor,
protein lipase activity, fatty acid incorpora-
a seven transmembrane spanning G-
tion, and fatty acid synthesis. Unlike GLP-1,
protein-coupled receptor (GPCR), leading to
GIP does not inhibit glucagon secretion or
increased cAMP production and enhanced
gastric emptying. The peptide promotes
protein kinase A (PKA) activity.
β-cell proliferation and cell survival in islet
The potential use of GLP-1 for the treatment
Structure of preproglu-cagon: GRPP, glicentin-
cell line studies.
of diabetes has been considered. GLP-1 ex-
related pancreatic
GLP-1 is derived from the product of the
erts antidiabetogenic properties in subjects
peptide; IP, intervening
proglucagon gene. This gene encodes a
with type 2 diabetes by stimulating insulin
peptides. Further pep-
preproprotein (see Fig. 3) that is differen-
secretion, increasing β-cell mass, inhibit-
tides derived from the
tially processed dependent on the tissue in
ing glucagon secretion, delaying gastric
preproprotein include
which it is expressed. In pancreatic α-cells,
emptying, and inducing satiety, thus slowing
glicentin which is com-
prohormone convertase 2 action leads to
the entry of sugar into the blood. However,
posed of amino acids 1-69, oxyntomodulin
the release of glucagon. In the gut, prohor-
GLP-1 is rapidly degraded by the enzyme
(glucagon-37) consisting
mone convertase 1/3 action leads to the
dipeptidyl peptidase IV (DPP IV), making it
of amino acids 33-69,
release of several peptides including GLP-
unattractive as a therapeutic agent.
and the major proglu-
1. Bioactive GLP-1 consists of two forms:
Successful strategies to overcome this dif-
cagon fragment (MPGF)
GLP-1 (7-37) and GLP-1 (7-36) amide. The
fi culty are the use of DPP IV-resistant GLP-1
comprising amino acids
latter form constitutes the majority (80%) of
receptor agonists, such as NN2211 (lira-
Post-translational
GLP-1 (7-36) amide
Peptides and Diabetes
glutide, a fatty acid-linked DPP IV-resistant
insulin-dependent diabetes mellitus or
derivative of GLP-1) or exendin-4 (exena-
maturity-onset diabetes) is associated with
tide). An alternative approach is the use
insulin resistance rather than the lack of
of inhibitors of DPP IV, such as sitagliptin,
insulin as seen in type 1 diabetes. This lack
P32/98 (H-Ile-thiazolidide hemifumarate),
of insulin sensitivity results in higher than
normal blood glucose levels.
amino)ethyl]-Gly-Pro-nitrile) and the Gly-
Type 2 diabetes is not HLA-linked and no
Pro-nitrile-derived compounds vildagliptin
autoimmune destruction of the pancre-
and saxagliptin.
atic cells is observed. The development of
Exendin-4 is a peptide hormone found
type 2 diabetes seems to be multifacto-
in the saliva of the Gila monster, a lizard
rial. Genetic predisposition appears to be
native to several Southwestern American
the strongest factor. Other risk factors are
states. Like GLP-1 exendin-4 exerts its
obesity and high caloric intake. Pancre-
effects through the GLP-1 receptor but is
atic α-cell mass is increased, followed by
much more potent than GLP-1. Exenatide,
an exaggerated response of glucagon to
a synthetic form of exendin-4 has been ap-
amino acids and an impaired suppression
proved by the FDA as an antidiabetic drug.
of glucagon secretion by hyperglycemia.
In contrast to most drugs that work by only
Increased hepatic production of glucose
one mechanism, exendin-4 acts by multiple
with a failure of the pancreas to adapt to
mechanisms, such as stimulation of insulin
this situation and resistance to the action
secretion, slowing gastric emptying, and
of insulin are characteristic features of this
inhibiting the production of glucose by the
disorder. Another important morphological
liver. Furthermore, exendin-4 was shown to
feature is the amyloid deposition in islets.
suppress appetite and promote weight loss.
These deposits consist of islet amyloid polypeptide or amylin, that is believed, to
Classifi cation of Diabetes Mellitus
originate in the β-cell secretory granule.
The American Diabetes Association distin-
Type 2 diabetes occurs most frequently
guishes between two main types of dia-
in adults, but is being noted increasingly
betes mellitus. This division is based upon
in adolescents as well. Type 2 diabetes
whether the ‘blood sugar problem‘ is caused
develops slowly and the symptoms are
by insulin defi ciency or insulin resistance:
usually less severe than in type 1. Some-
Type 1 diabetes (formerly known as insulin-
times the disease is only diagnosed several
dependent diabetes mellitus or juvenile-
years after its onset, when complications
onset diabetes) is a β-islet cell specifi c,
are already present. Common late micro-
T-lymphocyte-mediated autoimmune
vascular complications include retinopathy,
disorder. It is characterized by a failure of
nephropathy, and peripheral and autonomic
the pancreas to produce suffi cient insulin.
neuropathies. Macrovascular complications
Without insulin to promote the cellular up-
include atherosclerotic coronary peripheral
take of glucose, the blood glucose concen-
arterial disease.
trations reach high levels. At concentrations above 10 mM, renal tubular reabsorption
Treatment of Diabetes Mellitus
is saturated and glucose is passed into the
Insulin is essential for the treatment of type
urine. The classic symptoms are excessive
1 diabetes. The effects of insulin and its
secretion of urine, thirst, weight loss and
mechanism of action are described above.
For clinical application, either porcine or
It is known that multiple genes contribute
bovine insulin was given formerly. Today,
to the familial clustering of this disease, the
human insulin (produced recombinantly) is
major histocompatibility complex (MHC)
used. A new approach is the production of
being the most important of these. The
orally active insulin using modifi cations to
MHC class 2 genotype is one of the stron-
make insulin resistant to enzymatic break-
gest genetic factors determining disease
down, facilitating absorption.
Most of the vascular consequences of insu-
Type 2 diabetes (formerly named non-
lin resistance are due to the hyperglycemia
seen in type 2 diabetes. For this reason a
most widely prescribed insulin-sensitizing
Advances in genomics,
major goal of therapeutic intervention in
drug in clinical use. The major site of ac-
proteomics and me-
type 2 diabetes is to reduce circulating glu-
tion for metformin is the liver. Its use can
tabolomics will help us
to further understand
cose levels. There are many pharmacologi-
be contraindicated in patients with liver
the causes of type 1
cal strategies to accomplish these goals:
and type 2 diabetes and
1) The use of α-glucosidase inhibitors (e.g.
4) The thiazolidinediones (e.g. pioglitazone)
might eventually lead
acarbose) leads to a reduction in digestion
have been proven useful in treating the
to novel therapeutic
and thereby minimizes the consequent
hyperglycemia associated with insulin
absorption of glucose into the systemic
resistance in both type 2 diabetes and
circulation. The reduction in glucose uptake
non-diabetic conditions. These products
allows the pancreatic β-cells to regulate
function as agonists for the peroxisome
the insulin secretion more effectively. The
proliferator-activated receptor-γ (PPAR-γ).
advantage of α-glucosidase inhibitors is
PPARs are members of a nuclear receptor
that they function locally in the intestine
superfamily that has important roles in car-
and have no major systemic action. Plants
bohydrate and lipid metabolism. Thiazoli-
are rich sources of α-glucosidase inhibitors,
dinediones enhance peripheral sensitivity
some of which are being evaluated for their
to insulin and, to a lesser degree, decrease
hepatic glucose production by binding to
2) The sulfonylureas (e.g. glibenclamide)
and activating the PPAR-γ. Adverse effects
are referred to as endogenous insulin se-
of thiazolidine-diones include weight gain,
cretagogues because they induce the pan-
anemia, and abnormalities in liver and en-
creatic release of insulin and thus reduce
zyme levels. Resistin, an adipocyte-derived
plasma glucose. Sulfonylureas function
peptide, fi rst identifi ed during a search
by binding to and inhibiting the pancre-
for targets of thiazolidinediones, has been
atic ATP-dependent potassium channels
found to be downregulated by thiazolidin-
normally involved in the glucose-mediated
insulin secretion. Unwanted side-effects
5) GLP-1 analogs stimulate insulin release,
of sulfonylureas are appetite stimulation,
inhibit glucagon secretion, slow gastric
probably via their effects on insulin secre-
emptying and stimulate β-cell proliferation.
tion and blood glucose, often leading to
One of the most promising GLP-1 receptor
weight gain.
agonists is exenatide (exendin-4) which is
3) The biguanides (e.g. metformin) are a
53% identical to human GLP-1 at the amino
class of drugs that lower blood glucose
acid level. The main advantage of exenatide
levels by enhancing insulin-mediated
is its resistance to cleavage and inactiva-
suppression of hepatic glucose produc-
tion by dipeptidyl-peptidase IV (DPP IV). The
tion (gluconeogenesis) and by enhanc-
FDA has approved exenatide as adjunctive
ing insulin-stimulated glucose uptake by
therapy to improve blood sugar control in
skeletal muscle. Metformin is currently the
patients with type 2 diabetes who have not
MORE THAN 250 MILLION PEO-
PLE AROUND THE WORLD SUF-
FER FROM DIABETES AND THIS
NUMBER WILL GROW TO MORE
THAN 380 MILLIONS BY 2030
Peptides and Diabetes
achieved adequate control with metformin
and/or a sulfonylurea. A sustained release
Although some of the agents described
formulation is currently awaiting FDA ap-
above are still in the early phases of investi-
gation, there is little doubt that the therapy
The long-acting GLP-1 agonist liraglutide
of diabetes will undergo major changes in
was approved by the same authority for the
the near future. It is important to diagnose
treatment of type 2 diabetes in 2010.
all type 2 diabetics at an earlier stage (for
6) DPP IV inhibitors represent another
example by making self monitoring of blood
approach for the treatment of diabetes. Si-
glucose easier) and begin treatment in an
tagliptin is the fi rst candidate of this novel
attempt to minimize the diabetes-associat-
class of antihyperglycemic agents that
ed complications.
has been approved by the FDA. Linagliptin,
The identifi cation of the genetic com-
saxagliptin, and vildagliptin have been ap-
ponents of type 1 and type 2 diabetes is
proved as well in various countries world-
an important area of research, because
wide. These DPP IV inhibitors can be used
elucidation of the diabetes genes will infl u-
either alone or in combination with other
ence all efforts towards an understanding
oral antihyperglycemic agents (such as
of the disease, its complications, and its
metformin or a thiazolidinedione) for treat-
treatment, cure, and prevention. Recently,
ment of diabetes mellitus type 2.
genomic DNA from subjects with severe
7) Pramlintide, a soluble amylin analog, has
insulin resistance has been screened for
gained FDA approval as an adjunct to in-
mutations in genes that are implicated in
sulin therapy in type 1 and type 2 diabetes.
insulin signaling. Thereby, a mutation in the
Like amylin it acts centrally and decreases
gene encoding the serine/threonine kinase
glucagon secretion, slows gastric emptying
AKT2 (also known as PKBβ) was identifi ed.
and induces satiety.
AKT2 is highly expressed in insulin-sensi-
8) Insulin therapy is also indicated in
tive tissues and has been implicated in in-
the treatment of type 2 diabetes for the
sulin-regulated glucose uptake into muscle
management of severe hyperglycemia after
and fat cells by promoting the translocation
failure of oral agents.
of glucose transporter 4 (GLUT4) to the cell
9) C-Peptide is biologically active. Recent
clinical studies showed that administration
Advances in genomics, proteomics and
of C-peptide to diabetes type 1 patients
metabolomics will help us to further un-
lacking the peptide alleviates nerve and
derstand the causes of type 1 and type 2
renal dysfunctions associated with the
diabetes and might eventually lead to novel
R.J. Mahler and M.L. Adler
J.M. Egan et al.
In the 1970s, the insulin
Clinical Review 102: Type 2 diabe-
GLP-1 receptor agonists are growth
receptor was discov-
tes mellitus: update on diagnosis,
and differentiation factors for pan-
ered, and 10 years
later, its tyrosine kinase
pathophysiology, and treatment.
creatic islet beta cells.
activity was demon-
J. Clin. Endocrinol. Metab. 84, 1165
Diabetes Metab. Res. Rev. 19, 115-
strated.
-1171 (1999)
123 (2003)
L.B. Knudson et al.
R.I.G. Holt et al.
GLP-1 derivatives as novel com-
The role of the growth hormone-
pounds for the treatment of type 2
insulin-like growth factor axis in
diabetes: selection of NN2211 for
Diabet. Med. 20, 3-15 (2003)
Drugs Future 26, 677-685 (2001)
G.G. Holz and O.G. Chepurny
A.D. Baron et al.
Glucagon-like peptide-1 synthetic
Novel peptides under development
analogs: new therapeutic agents
for the treatment of type 1 and type
for use in the treatment of diabetes
2 diabetes mellitus.
Curr. Drug Targets Immune Endocr.
Curr. Med. Chem. 10, 2471-2483
Metabol. Disord. 2, 63-82 (2002)
D.J. Drucker
G. Jiang and B.B. Zhang
Biological actions and therapeu-
Glucagon and regulation of glucose
tic potential of the glucagon-like
Am. J. Physiol. Endocrinol. Metab.
Gastroenterology 122, 531-544
284, E671-E678 (2003)
T.J. Kieffer
J.J. Holst
GIP or not GIP? That is the question.
Gastric inhibitory polypeptide ana-
Trends Pharmacol. Sci. 24, 110-112
logues: do they have a therapeutic
role in diabetes mellitus similar to
L. Marzban et al.
that of glucagon-like
Islet amyloid polypeptide and type 2
BioDrugs 16, 175-181 (2002)
Exp. Gerontol. 38, 347-351 (2003)
J.J. Holst
P.G. McTernan et al.
Therapy of type 2 diabetes mellitus
Resistin and type 2 diabetes: regula-
based on the actions of glucagon-
tion of resistin expression by insulin
like peptide-1.
and rosiglitazone and the effects of
Diabetes Metab. Res. Rev. 18, 430-
recombinant resistin on lipid and
441 (2002)
glucose metabolism in human dif-
S. Yakar et al.
The role of circulating IGF-I.
J. Clin. Endocrinol. Metab. 88, 6098-
Lessons from human and animal
6106 (2003)
J.J. Meier et al.
Endocrine 19, 239-248 (2002)
Glucagon-like peptide 1 and gastric
inhibitory polypeptide: potential
Gut peptides and type 2 diabetes
applications in type 2 diabetes mel-
mellitus treatment.
Current Diabetes Reports 3, 365-372
BioDrugs 17, 93-102 (2003)
N. Moller et al.
D.J. Drucker
Effects of ageing on insulin secre-
Enhancing incretin action for the
tion and action.
treatment of type 2 diabetes.
Horm. Res. 60, 102-104 (2003)
Diabetes Care 26, 2929-2940 (2003)
Peptides and Diabetes
T. Perry and N.H. Greig
L.L. Nielsen et al.
As with humans, diabe-
The glucagon-like peptides: a
Pharmacology of exenatide (syn-
tes has become a grow-
double-edged therapeutic sword?
thetic exendin-4): a potential thera-
ing problem with dogs
and cats in recent years
Trends Pharmacol. Sci. 24, 377-383
peutic for improved glycemic control
due to their increasing
of type 2 diabetes.
life expectancy in com-
B. Thorens
Regul. Peptides 117, 77-88 (2004)
bination with obesity
Gluco-incretin hormones in insulin
A. Nourparvar et al.
and lack of exercise.
secretion and diabetes.
Novel strategies for the pharma-
Med. Sci. (Paris) 19, 860-863 (2003)
cological management of type 2
T. Vahl and D. D'Alessio
Enteroinsular signaling: perspec-
Trends Pharmacol. Sci. 25, 86-91
tives on the role of the gastrointesti-
nal hormones glucagon-like peptide
S.M. Rangwala and M.A. Lazar
1 and glucose-dependent insuli-
Peroxisome proliferator-activated
notropic polypeptide in normal and
receptor γ in diabetes and metabo-
abnormal glucose metabolism.
Curr. Opin. Clin. Nutr. Metab. Care 6,
Trends Pharmacol. Sci. 25, 331-336
461-468 (2003)
M.F. White
Y. Sato et al.
Insulin signaling in health and
C-peptide fragments stimulate glu-
cose utilization in diabetic rats.
Science 302, 1710-1711 (2003)
Cell. Mol. Life Sci. 61, 727-732 (2004)
P.E. Wiedeman and J.M. Trevillyan
T.P. Vahl and D.A. D‘Alessio
Dipeptidyl peptidase IV inhibitors for
Gut peptides in the treatment of
the treatment of impaired glucose
diabetes mellitus.
tolerance and type 2 diabetes.
Expert. Opin. Investig. Drugs. 13, 177-
Curr. Opin. Investig. Drugs 4, 412-420
188 (2004)
J.F. Gautier et al.
Y. Dor et al.
Biological actions of the incretins
Adult pancreatic β-cells are formed
GIP and GLP-1 and therapeutic
by self-duplication rather than
perspectives in patients with type 2
Nature 429, 41-46 (2004)
Diabetes Metab. 31, 233-242 (2005)
E.A. Gale et al.
E.M. Sinclair and D.J. Drucker
European Nicotinamide Diabetes
Proglucagon-derived peptides:
Intervention Trial (ENDIT) Group:
mechanisms of action and thera-
A randomised controlled trial of
peutic potential.
intervention before the onset of type
Physiology 20, 357-365 (2005)
D.J. Drucker and M.A. Nauck
Lancet 363, 925-931 (2004)
The incretin system: glucagon-like
S. George et al.
peptide-1 receptor agonists and
A family with severe insulin resis-
dipeptidyl peptidase-4 inhibitors in
tance and diabetes due to a muta-
type 2 diabetes.
tion in AKT2.
Lancet 368, 1696-1705 (2006)
Science 304, 1325-1328 (2004)
K. Fujioka
J.F. List and J.F. Habener
Pathophysiology of type 2 diabetes
Glucagon-like peptide 1 agonists
and the role of incretin hormones
and the development and growth of
and beta-cell dysfunction.
JAAPA Suppl, 3-8 (2007)
Am. J. Physiol. Endocrinol. Metab.
R. Gadsby
New treatments for type 2 diabetes - the DPP4 inhibitors.
Prim. Care Diabetes 1, 209-211 (2007)
W. Benalla et al.
Pancreatic islet dysfunction in type
Antidiabetic medicinal plants as a
2 diabetes: a rational target for
source of alpha glucosidase inhibi-
Curr. Med. Res. Opin. 23, 933-944
Curr. Diab. Rev. 6 247-254 (2010)
M. Christensen and F.K. Knop
J. Wahren et al.
Once-weekly GLP-1 agonists: How
C-Peptide is a bioactive peptide.
do they differ from exenatide and
Diabetologia 50, 503-509 (2007)
A.M. Abbatecola et al.
Curr. Diab. Rep. 10, 124-132 (2010)
New approaches to treating type 2
B. Gallwitz
diabetes mellitus in the elderly: role
Benefi t-risk assessment of exena-
of incretin therapies.
tide in the therapy of type 2 diabetes
Drugs Aging 25, 913-925 (2008)
S.E. Inzucchi and D.K. McGuire
Drug Saf. 33, 87-100 (2010)
New drugs for the treatment of dia-
J. Gerich
betes: part II: Incretin-based therapy
DPP-4 inhibitors: what may be the
Circulation 117, 574-584 (2008)
Diabetes Res. Clin. Pract. 90, 131-
A.M. Lambeir et al.
140 (2010)
DPP4 inhibitors for diabetes - what
The future of incretin-based thera-
Biochem. Pharmacol. 76, 1637-1643
py: novel avenues - novel targets.
Diabetes Obes. Metab. 13 Suppl 1,
N. Mikhail
158-166 (2011)
Incretin mimetics and dipeptidyl
M.J. Davies et al.
peptidase 4 inhibitors in clinical
Liraglutide - overview of the preclini-
trials for the treatment of type 2
cal and clinical data and its role in
the treatment of type 2 diabetes.
Expert Opin. Investig. Drugs 17, 845-
Diabetes Obes. Metab. 13, 207-220
853 (2008)
Y. Ng et al.
B. Gallwitz
Rapid activation of Akt2 is suffi cient
GLP-1 agonists and dipeptidyl-pep-
to stimulate GLUT4 translocation in
tidase IV inhibitors.
3T3-L1 adipocytes.
Handb. Exp. Pharmacol. 53-74 (2011)
Cell. Metab. 7, 348-356 (2008)
D.M. Irwin and K.J. Prentice
P.R. Flatt et al.
Incretin hormones and the ex-
Recent advances in antidiabetic
panding families of glucagon-like
drug therapies targeting the entero-
sequences and their receptors.
insular axis.
Diabetes Obes. Metab. 13 Suppl 1,
Curr. Drug Metab. 10, 125-137 (2009)
69-81 (2011)
R. Gupta et al.
G.J. Ryan and Y. Hardy
Despite the steady
Emerging drug candidates of dipep-
Liraglutide: once-daily GLP-1
progress in research,
tidyl peptidase IV (DPP IV) inhibitor
agonist for the treatment of type 2
the dramatic spread of
diabetes mellitus which
class for the treatment of type 2
is observed throughout
J. Clin. Pharm. Ther. 36, 260-274
the world remains one
Curr. Drug Targets 10, 71-87 (2009)
of the most challeng-
F.K. Knop et al.
P. Westermark et al.
ing health problems of
Incretin-based therapy of type 2
Islet amyloid polypeptide, islet amy-
the 21st century. Today,
diabetes mellitus.
loid, and diabetes mellitus.
diabetes mellitus is one
Curr. Protein Pept. Sci. 10, 46-55
Physiol. Rev. 91, 795-826 (2011)
of the main causes of
death in most devel-
Peptides and Diabetes
PEPTIDES
Bachem offers peptidic active pharmaceutical ingredients (generic APIs) and Clinalfa® basic ready-to-use formulations, sterile products for approved clinical studies, please see page18 or go to www.bachem.com
Amylin (human)
Acetyl-Amylin (8-37) (human)
(Amlintide; IAPP (human))
Amylin (8-37) (mouse, rat)
Amylin (mouse, rat)
Acetyl-Amylin (8-37) (mouse, rat)
Amylin (1-13) (human)
Amylin (20-29) (human)
Amylin (8-37) (human)
C-Peptide 2 (rat)
C-PEPTIDE
Proinsulin C-Peptide (31-63)
Proinsulin C-Peptide (55-89)
(human)
([D ]Val7·10)-C-Peptide (human)
EAEDLQ[D ]VGQ[D ]VELGGGPGAGSLQPLA-
Tyr-Proinsulin C-Peptide (55-89)
C-Peptide 1 (rat)
Peptides and Diabetes
Exenatide
Gastric Inhibitory Polypeptide
Gastric Inhibitory Polypeptide (1-30)
INHIBITORY
POLYPEPTIDE
Gastric Inhibitory Polypeptide (3-42)
Gastric Inhibitory Polypeptide
Gastric Inhibitory Polypeptide (6-30)
amide (human)
H-6102
FISDYSIAMDKIHQQDFVNWLLAQK-NH2
Glucagon (1-29) (human, rat, porcine)
(Des-His1,Glu9)-Glucagon (1-29) amide
GLUCAGON
(human, rat, porcine)
AND OXYNTO-
([13C ]Leu14)-Glucagon (1-29) (human,
(Des-Thr5)-Glucagon (1-29)
(Des-Thr7)-Glucagon (1-29)
Biotinyl-Glucagon (1-29)
(human, rat, porcine)
(Met(O)27)-Glucagon (1-29)
Oxyntomodulin (bovine, dog, porcine)
GLUCAGON
(human, rat, porcine)
(Glucagon-37 (bovine, dog, porcine))
AND OXYNTO-
Glucagon (19-29)
Oxyntomodulin (human, mouse, rat)
(human, rat, porcine)
(Glucagon-37 (human, mouse, rat))
GRPP (human)
H-6062
Oxyntomodulin (30-37)
(bovine, dog, porcine)
GLP-1 (1-36) amide (human, bovine,
GLP-1 (7-36)-Lys(6-FAM) amide (hu-
GLUCAGON-LIKE guinea pig, mouse, rat)
man, bovine, guinea pig, mouse, rat)
GLP-1 (1-37) (human, bovine,
GLP-1 (7-37) (human, bovine, guinea
guinea pig, mouse, rat)
pig, mouse, rat) (Acetate salt)
GRG (Acetate salt)
GLP-1 (7-36) amide
GLP-1 (7-37) (human, bovine, guinea
(chicken, common turkey)
pig, mouse, rat)
(Trifl uoroacetate salt)
GRG (Trifl uoroacetate salt)
GLP-1 (7-36) amide (human, bovine,
guinea pig, mouse, rat)
Liraglutide
(Ser8)-GLP-1 (7-36) amide (human,
bovine, guinea pig, mouse, rat)
H-4592
GLP-1 (9-36) amide (human, bovine,
guinea pig, mouse, porcine, rat)
GLP-1 (7-36)-Lys(biotinyl) amide (hu-
man, bovine, guinea pig, mouse, rat)
H-5956
HAEGTFTSDVSSYLEGQAAKEFIAWLVKG
RK(biotinyl)-NH2
Peptides and Diabetes
GLP-2 (1-33) (human)
GLP-2 (rat)
GLP-2 (1-34) (human)
H-4766
H-Asn-Pro-Glu-Tyr(PO H )-OH
rec IGF-II (1-67) (human)
INSULIN,
rec IGF-I (human)
FACTOR (IGF) IGF-I Analog
CYAAPLKPAKSC (Disulfi de bond)
Lys-Lys-IRS-1 (891-902)
(dephosphorylated) (human)
IGF-I (1-3)
Insulin B (22-25)
IGF-I (24-41)
Pancreastatin (33-48) (human)
Pancreastatin (33-49) (porcine)
Pseudin-2
(Pyr1)-Apelin-13 (human, bovine,
mouse, rat)
Calcitonin (8-32) (salmon I)
(Disulfi de bonds, air oxidized)
Peptides and Diabetes
Exendin (9-39) Acetate
Glucagon
GENERIC APIs
GLP-1 (7-36) amide Acetate
IGF-I (1-3)
*offered on request
** offered under Bolar Exemption:
This product is offered and sold in small quantities only and solely for uses reasonably related to privi-
leged trials and studies for obtaining marketing
Liraglutide Acetate**
authorization required by law (Bolar Exemption).
GLP-1 (7-37) Acetate*
Bachem cannot be made liable for any infringe-
ment of intellectual property rights. It is the sole
and only responsibility of the purchaser or user of this product to comply with the relevant national
rules and regulations.
(Pyr1)-Apelin-13 Acetate
GIP Acetate
1 mg/vial (Clinalfa basic)
500 μg/vial (Clinalfa basic)
Exendin (9-39) Acetate
10 mg/vial (Clinalfa basic)
GLP-1 (7-36) amide Acetate
100 μg/vial (Clinalfa basic)
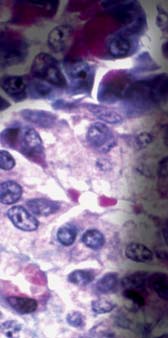
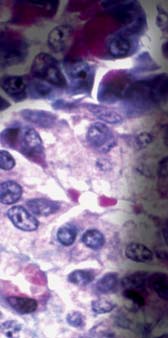
PANCREATIC
ISLET OF
LANGERHANS
Islets of Langerhans.
Light micrograph of a section through
an islet of Langerhans (pale, centre) in
pancreas tissue. This clump of secre-
tory cells forms part of the endocrine
system of the body, which releases
hormones into the blood. It is com-
posed of numerous beta cells (purple),
which secrete insulin, and the less
numerous alpha cells (pink), which
secrete glucagon. Insulin stimulates
the uptake of glucose and amino
acids from the bloodstream, whereas
glucagon has the opposite effect; it
stimulates the breakdown of glycogen
in the tissues. This causes glucose
and amino acids to be released into
the blood.
KEYSTONE/SCIENCE PHOTO LIBRARY/CNRI
Marketing & Sales Contact
Europe, Africa, Middle East and Asia Pacifi c:
Bachem AG
Tel. +41 61 935 2323
Bachem Americas, Inc.
Tel. +1 888 422 2436
[email protected]
Visit our website
www.bachem. com
or shop online
shop.bachem.com
All information is compiled to the best of our knowledge. We cannot be made liable for any possible errors or misprints. Some products may be
restricted in certain countries.
www.bachem. com
Source: http://www.chayon.co.kr/email/2014/0321_peptide/Diabetes_Peptides.pdf
VETimpulse · 20. Jahrgang · Ausgabe 14 · 15. Juli 2011 Bulbusexstirpation am stehenden Pferd Geringere Blutungsneigung Fotos (3): Roeckl und bessere Sichtverhältnisse Die Risiken bei der Allgemeinanästhesie des Pferdes liegen trotz moderner Anästhetika und Überwachungsmetho- den bei über einem Prozent. Damit sind sie immer noch zehn- bis 100-fach höher als bei Hund, Katze und
Nutrition Facts Oreo® Cookie Cheesecake Serving Size: 1/6 Cake (113g) Servings Per Container: 6 Oreo® Cookie pieces [sugar, enriched unbleached wheat flour (wheat flour, niacin, reduced iron, thiamin mononitrate, riboflavin, folic acid), high oleic canola and/or palm and/or canola and/or Amount Per Serving soybean oils, cocoa alkali processed, high fructose corn syrup, corn starch, leavening (baking