Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Md-booklet-08-6
Age-Related
K. Bailey Freund, M.D.
James M. Klancnik, Jr., M.D.
Lawrence A. Yannuzzi, M.D.
Bruce Rosenthal, O.D.
Anatomy of the Eye
The Retina
Early Macular Degeneration
Dry (Atrophic) Macular Degeneration
Wet (Neovascular) Macular Degeneration
Examination & Diagnosis
Optical Coherence Tomography (OCT)
Age-Related Macular Degeneration
2008 by The Macula Foundation, Inc.
All rights reserved.
This booklet, or any part thereof, may not be used or
reproduced in any manner without written permission.
Photodynamic Therapy (PDT)
The Macula Foundation, Inc.
LuEsther T. Mertz Retinal Research Center210 East 64th Street
Research and Experimental Treatments
New York, New York 10065
Inhibiting the Growth of
Abnormal Blood Vessels
Targeting the Immune System and
Booklet design by: Jana DeWitt Design and iKnow
Macular degeneration is the most common cause of
Low Dose Radiation Therapy
severe vision loss in people over the age of 50. More
than 8 million people in the United States alone have
some form of this disease. This booklet is intended
to educate patients and their families about macular
Implantable Miniature Telescope
degeneration, its treatment and low vision
Drug Delivery Methods
The term "macular degeneration" includes many
Laser Treatment of Drusen
different eye diseases, all of which affect central, or
Health & Nutrition
detail, vision. Age-related macular degeneration is
Risk Factors
the most common of these disorders, mainly
affecting people over the age of 60. Although age-
related macular degeneration is our primary focus
here, much of the information also applies to other
Living With Low Vision
types of macular degeneration.
A Low Vision Evaluation
Helpful Devices for Work, Home and
We hope that this booklet increases your
understanding of macular degeneration and
A Team Effort
enhances your communication with your
Resources for People with Low Vision
ophthalmologist and other health care providers.
The Amsler Grid
Instructions for Using the Amsler Grid

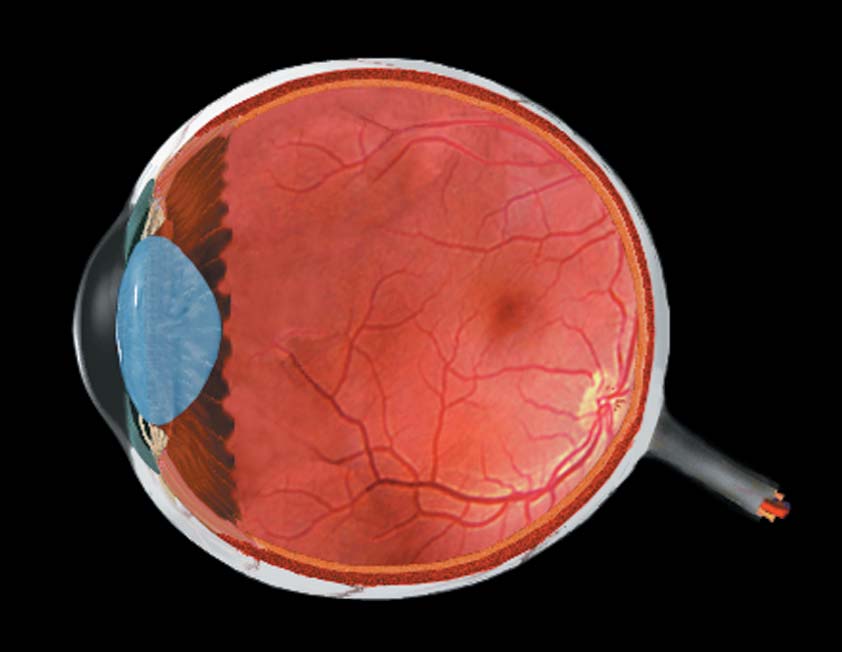
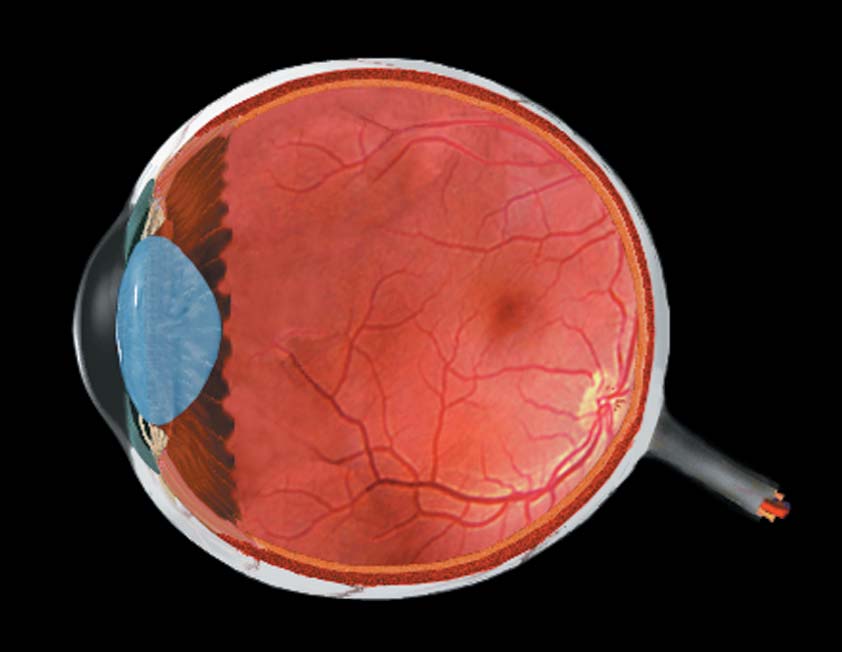
Anatomy of the Eye
The eye is a complex organ composed of many parts.
Good vision depends on how these parts work
optic nerve
together. It is helpful to understand how the eye
works before learning about macular degeneration.
As light enters the eye, it first passes through a
lubricating tear film that coats the cornea. The clear
cornea covers the front of the eye and helps to focus
incoming light.
The iris is the colored part of the eye. As light
conditions change, the iris may dilate to make the
pupil bigger or constrict to make the pupil smaller.
This allows more or less light into the eye.
Light then passes through the lens, a flexible,
transparent structure that can change its shape to
focus images on the retina.
After being focused by the lens, light passes through
the center of the eye on its way to the retina. The
eye is filled with a clear jelly called the vitreous.
Finally, light falls upon the retina, a thin, light-sensitive
tissue lining the back of the eye. The retina converts
light patterns into information the brain can use.
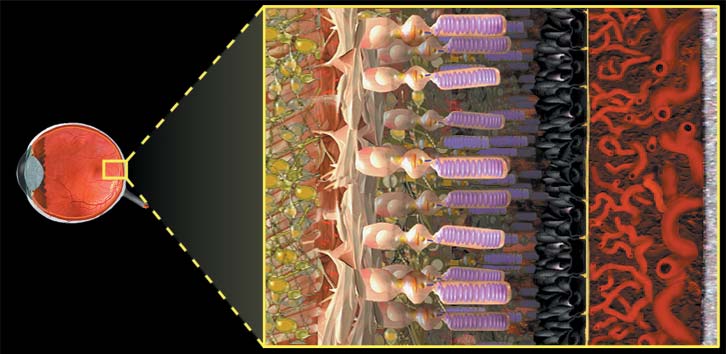
The Retina
The macula is the small central portion of the retina
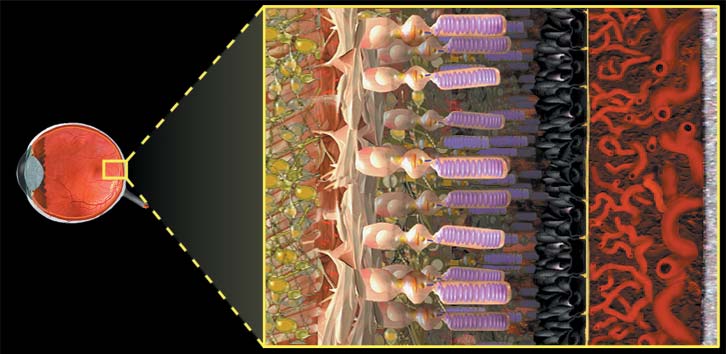
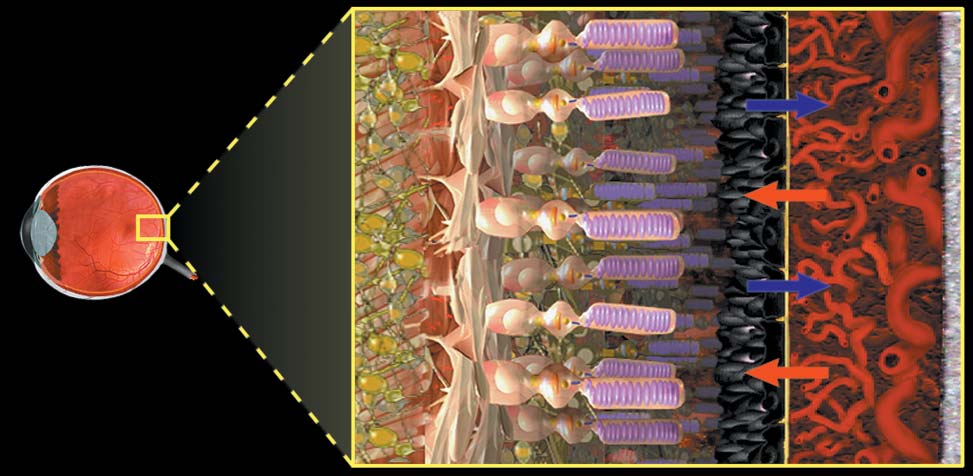
The retina is composed of many different tissue layers,
with the densest population of photoreceptors, the
each with a specific function. Some of these layers
light-sensing cells. The center of the macula is called
may not be working properly in an eye with macular
the fovea. With the highest density of photoreceptors,
the fovea is what allows one to see fine detail such
as small newsprint.
Behind the retina, a layer of blood vessels called the
choroid supplies oxygen and nutrients to outer
layers of the retina.
The optic nerve is a bundle of nerve fibers that
carries visual information from the eye to the brain.
optic nerve
This cross-section shows an enlarged view of the retina.
The photoreceptor layer is composed of light-sensitive
cells called rods and cones. Light images are
converted into electrochemical signals inside the
photoreceptors.


Early Macular Degeneration
Age-related macular degeneration is an eye disease
that primarily affects the central portion of the retina
known as the macula. The risk for developing
macular degeneration increases with age and is over
30% by age 75. Other risk factors include a family
history of the disease, cigarette smoking, diet,
excessive sunlight exposure, high blood pressure and
cardiovascular disease.
Bruch's membrane sclera
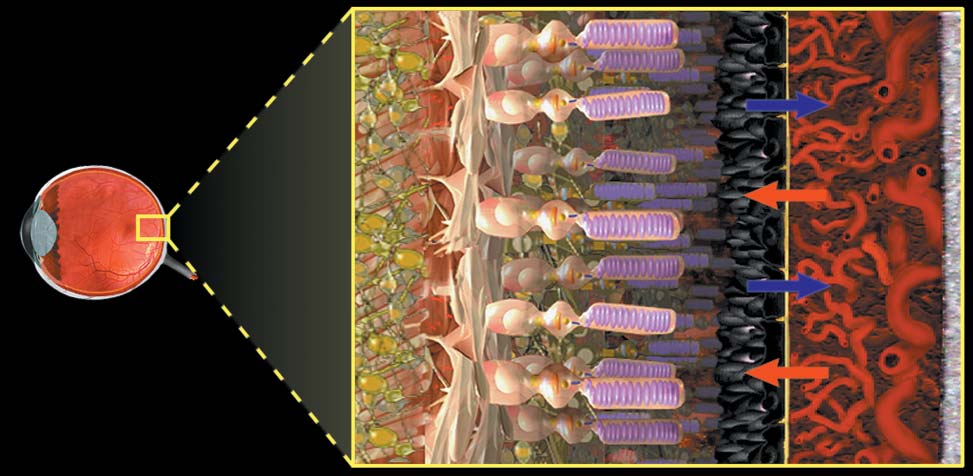
Under the photoreceptors is a dark layer called the
retinal pigment epithelium (RPE). Cells of the RPE
absorb excess light and transport oxygen, nutrients
and cellular wastes between the photoreceptors and
the choroid.
Bruch's membrane separates the blood vessels of the
choroid from the RPE layer.
The choroid is a layer of blood vessels that supplies
This photograph shows a normal, healthy
oxygen and nutrients to the outer layers of the retina.
retina as viewed by an eye doctor during
an examination. The ophthalmologist will
The sclera is the fibrous, white, outer covering of
pay careful attention to the appearance
of the macula and fovea when examining
the retina.

The majority of people with macular degeneration
An eye doctor examining a patient at this stage may
have an early form of the condition and experience
note the presence of these drusen, even though most
minimal vision loss. For many of these people,
people have no symptoms. Patients with drusen
macular degeneration will not progress.
need to be observed over time, although most will
not progress to develop vision loss. Many people
In the early stages of macular degeneration, the
over the age of 60 will have some drusen.
transport of nutrients and wastes by the retinal
pigment epithelium (RPE) slows down. As waste
A portion of people with drusen may begin to
products accumulate under the retina, they form
experience mild vision loss. At this point, macular
yellowish deposits called drusen.
degeneration may progress in one of two ways.
These two types of degeneration are known as the
dry (atrophic) and the wet (neovascular) forms of the
nutrients waste products
disease. Neovascular macular degeneration is
sometimes referred to as "exudative" macular
degeneration.
photoreceptors retinal pigment
In the healthy retina, a layer of cells called the retinal
pigment epithelium (RPE) supplies the photoreceptors
with nutrients and pumps out the waste products created
This retinal photograph shows numerous
as the photoreceptors convert light into nerve signals.
yellow drusen in and around the macular
region of the retina.

Dry (Atrophic) Macular Degeneration
Dry (atrophic) macular degeneration is a slowly
progressing condition characterized by the
accumulation of drusen beneath the retina with some
vision loss. Dry macular degeneration rarely causes
severe vision impairment or blindness.
As the retinal pigment epithelium (RPE) continues to
slow down in its transport of nutrients and wastes,
the overlying photoreceptors become damaged. The
retinal pigment
size and number of drusen in the macula increase.
Vision may be affected as RPE and photoreceptor
In dry macular degeneration, waste products from the
cells are lost due to atrophy.
photoreceptors accumulate underneath the retinal
pigment epithelium (RPE). The waste appears as
yellowish spots called drusen.
As areas of retina lose function, patients begin to
lose sight in certain areas of their central field of
vision. Occasionally, a large region of cells is lost.
This is called "geographic atrophy" and it produces a
blind spot in the central portion of vision. This blind
spot is called a scotoma.
This retinal photograph shows many
drusen in the macula. Drusen are
typical of dry macular degeneration.
14
There are certain steps you can take to help slow
down the progress of dry macular degeneration. In
the Health and Nutrition section on page 65, we
recommend dietary changes, taking nutritional
supplements, stopping smoking and controlling
blood pressure. While there is a great deal of
research currently under way, we have no other
proven prevention or treatment strategies for dry
macular degeneration. Fortunately, the majority of
area of atrophy
people who have reached this stage of the disease
will not progress to the more serious, wet form.
This retinal photograph shows
geographic atrophy in the macular
region resulting from advanced dry
If you have macular degeneration, it is essential that
you report any changes in your vision to your eye
doctor immediately. Careful self-monitoring with the
Amsler grid (see instructions at the end of this
booklet) and regular examinations by an eye doctor
are crucial for preserving your vision. This is because
some people with dry macular degeneration will
develop the more severe "wet" form of the disease
Regular use of the Amsler Grid is important if you have
which requires treatment as soon as possible.
macular degeneration (see the "Amsler Grid" section at the
end of this booklet). Small blind spots may appear in your
vision as dry macular degeneration progresses. The Amsler
Grid can help you notice changes in your vision that might
otherwise be missed.
Wet (Neovascular) Macular Degeneration
Wet macular degeneration is classified by wherethe CNV develops in the retina.
For reasons that are not fully understood, a minority
• CNV that develops directly beneath the
of people with macular degeneration develop a more
photoreceptors, which is easily seen by
serious form of the disease. People with large "soft"
angiography, is referred to as "classic" CNV.
drusen (drusen with indistinct borders), many drusen
• CNV that develops beneath the RPE layer, which
that run together, or pigment cells in the macula that
is more difficult to see by angiography, is
look abnormal are at greater risk for developing the
wet (neovascular) form of the disease.
referred to as "occult" CNV.
• CNV that forms within the retina is sometimes
In the wet form of macular degeneration, new blood
referred to as retinal angiomatous proliferation or
vessels begin to grow underneath the retina. The
proliferation of these new blood vessels is called
choroidal neovascularization (CNV).
• CNV that results in large, leaky blood vessels is
called polypoidal choroidal vasculopathy or
choroidal neovascularization (CNV)
"polypoidal." The polypoidal vessels in thiscondition tend to cause extensive leakage andbleeding under the retina.
photoreceptors retinal pigment
As CNV grows, the new vessels may leak blood or
fluid under and into the retina, causing the retinal
surface to become uneven. As a result, objects in
that portion of the visual field may appear wavy or
distorted. The neovascularization may even break
through some of the retinal layers. Blind spots may
appear in your vision if portions of the retina become
damaged by the CNV.
and blood
This retinal photograph shows fluid and
blood beneath the retina, which
suggests the presence of CNV.
It is believed that the diseased retina stimulates the
production of these new blood vessels in response
to a decreased supply of nutrients and slow
transport of wastes. Unfortunately, the new blood
vessels do not improve the health of the retina.
As the surface of the retina becomes
uneven, objects may appear blurred,
wavy or distorted. As the condition
progresses, blind spots may appear.
Often, the first sign of fluid or blood under the retina
Eventually, areas of neovascularization and leakage
is distortion of straight lines. Just as in a camera, if
can lead to the death of the overlying
the film is not lying flat, images will be distorted.
photoreceptors and scarring of the macula. Scarring
Because these changes can be subtle, regular testing
is the final stage of macular degeneration and it
with the Amsler grid at the end of this booklet can
frequently results in significant vision loss.
be helpful in the early detection of problems. Any
It is important to realize that this entire process
change in the appearance of the grid may be a sign
occurs only in the macula and affects only central, or
of CNV and should prompt a visit to the eye doctor.
detail, vision. Peripheral, or side vision, is rarely
If caught early enough, the CNV might be treatable
affected by macular degeneration. While macular
before it causes too much damage.
degeneration is the leading cause of legal blindness,
it rarely leads to total blindness.
Legal blindnessmeans vision is20/200 or worse in the better eye even with correctivelenses, or peripheralvision is restricted to the extent that
only "tunnel vision"remains.
This retinal photograph shows a
The first indication of fluid or blood under the retina may
large yellow scar in the macular
be a distortion of straight lines. The Amsler grid test,
region resulting from advanced CNV.
which you can do at home, is an important tool for the
A person with this type of scarring
early detection of any changes in your vision. Instructions
would experience a significant loss of
for using the Amsler grid are at the end of this booklet.
vision in that eye.
Examination & Diagnosis
Eyedrops are given to dilate your pupils. This will
allow your doctor to examine the retina through the
enlarged pupil. The drops typically take between 20
and 45 minutes to work and will wear off in several
A thorough examination by an eye doctor is the best
hours. While the pupils are dilated, it is usually difficult
way to determine if you have macular degeneration
to read, and bright lights may be uncomfortable. Some
or if you are at risk for developing the condition.
patients wear sunglasses after dilation to reduce
The exam begins with testing of your visual acuity or
the sharpness of your vision. There are several
After the dilating drops are administered and given
different tests for visual acuity. The most familiar one
time to work, the eye doctor seats the patient at a
has black letters on a white chart.
device called a slit lamp. The slit lamp is a special
Next, your eyes may be tested with an Amsler grid.
microscope that enables the doctor to examine the
This test helps your doctor to determine whether
different parts of the eye under magnification. When
you are experiencing areas of distorted or reduced
used with special lenses, the slit lamp gives the
vision, which are both common symptoms of
doctor a highly magnified view of the retina.
macular degeneration. If you do have macular
degeneration, your doctor will use the Amsler grid to
determine if your vision has changed. Your
ophthalmologist may provide you with a small
version of the Amsler grid to carry with you in your
purse or wallet. Instructions for using an Amsler grid
at home appear at the end of this booklet.
After these vision tests, the front part of your eyes
will be examined to determine if everything is
healthy. Your doctor may put anesthetic drops in
your eyes so that the level of pressure can be
The slit lamp is a microscope that shows a
measured in each eye.
magnified view of the retina. Your eye doctor will
look for drusen and other areas of the retina that
appear suspicious or abnormal.
The doctor will look for drusen and other areas of the
A technique called angiography is the most useful
retina that might appear suspicious or abnormal.
test to look for CNV. The procedure is painless and
Because the new blood vessel growth found in the
very safe. The patient is seated at a fundus camera
"wet" form of macular degeneration (choroidal
so pictures of the retina can be taken. A small IV
neovascularization or CNV) occurs beneath the
catheter is inserted into a large vein, usually in the
retina, the blood vessels themselves are not usually
arm. A dye is injected through the catheter into the
visible. But the examination can reveal clues, such as
vein. The dye circulates throughout the blood
bleeding, elevation of the retina or fluid behind the
vessels of the body. As the dye enters the blood
retina, that suggest the presence of CNV. In these
vessels of the eye, a series of pictures is taken of the
cases, further testing may be necessary.
retina. Special filters make the dye stand out against
the background of the retina.
fluid under
the retina
This retinal photograph shows many drusen
and fluid under the retina, which suggests the
presence of choroidal neovascularization
(CNV). Additional testing would be required
The fundus camera takes pictures of the retina
for complete diagnosis and treatment.
(see examples at right). The camera may use
film or it may be digital, displaying the images
on a computer screen.
By looking at the pattern of the blood vessels and
procedure, and it has been performed in millions of
observing whether dye leaks from any of the vessels,
patients for more than 25 years. Most patients
the ophthalmologist can locate sites of CNV if they
experience no symptoms when the dye is injected. A
are present.
small minority may feel flushed or briefly nauseated.
Rarely, someone has an allergy to fluorescein and may
experience itching or other symptoms that require
treatment. After the test, your kidneys remove the
fluorescein dye from your body; therefore, your urine
will turn orange or dark yellow for up to 24 hours.
Sometimes, an area of CNV is not clearly defined, or it
may be obscured by overlying fluid or blood. In these
cases, your ophthalmologist may find it helpful to
perform angiography using ICG dye instead of
fluorescein. ICG is also useful for visualizing the deeper
blood vessels located in the choroid. ICG can show
This fluorescein angiogram shows CNV in
how the choroidal circulation is interacting with other
the macula. The bright area indicates dye
layers of the retina and whether variant forms of CNV,
leaking from the newly formed vessels.
such as retinal angiomatous proliferation (RAP) or
polypoidal choroidal vasculopathy are present. ICG
Two dyes are commonly used in ophthalmology: an
angiograms are typically performed using a digital
orange dye called fluorescein and a green dye called
fundus camera or another instrument called a scanning
indocyanine green (ICG). These dyes are different from
laser ophthalmoscope (SLO). Side effects from ICG dye
those used for angiograms of the heart or brain. X-
are rare and similar to those from fluorescein. ICG dye
rays are not used in this procedure because the blood
does contain a form of iodine, so if you are allergic to
vessels can be directly viewed and photographed
iodine you should tell your ophthalmologist.
through the pupil.
Your ophthalmologist may also perform high-speed
Most of the time, CNV can be seen with fluorescein
video angiography. This type of angiography also
dye. Fluorescein angiography is an extremely safe
requires dye, but it captures dynamic "movies" of
Optical Coherence Tomography
This ICG angiogram shows a bright area of
An optical coherence tomography (OCT) device
CNV in the macula. The CNV was not visible
is used to map the anatomy of the retina.
with fluorescein dye because of abnormal
fluid beneath the retina.
Optical coherence tomography (OCT) is an additional
technique for imaging the retina. It is a non-invasive
blood flow patterns in the retina instead of still
test that records the features of the retina and
pictures. This reveals additional information about
displays this information as cross-sectional views, or
CNV. For example, it may provide a view of smaller
optical ‘slices.' For this procedure, the patient is
vessels that are "feeding" the growth of the CNV. The
seated at the OCT device. Laser light is used to map
feeder vessels can then be precisely treated, sparing
the anatomy of the retina, and the resulting computer
healthier areas of the retina.
images are saved for analysis. OCT evaluations are
not a replacement for angiography. OCT is used as an
The different types of angiography can be used
additional test that provides different information
separately or together to provide as much information
such as whether excess fluid is present in the retina.
as possible about the location, size, number and type
OCT may be used to monitor how well treatment for
of CNV areas that may be present in the eyes.
wet macular degeneration is working.
Evaluating the specific characteristics of areas of CNV
is useful for determining which type of treatment is
Inside the newest OCT instruments, a spectrometer
likely to be most successful.
is used along with the laser light to map the
Autofluorescence imaging of the retina is a new
technique that involves capturing a response from
molecules in the RPE. There are two ways to obtain
these images. One uses a specialized scanning laser,
and the other uses special filters attached to the
fundus camera. Both types are noninvasive. The
This is an OCT image of the macula in a normal,
images show areas of stress and damage to the
healthy eye. The depression in the center is the
retina and can be used to monitor these changes
fovea. Note how smooth and even the layers are.
over time.
This is an OCT image of the macula in an eye with
wet macular degeneration. Because of fluid build-
up, the tissue layers are no longer smooth and flat.
anatomy of the retina. This technology, known as
"spectral domain" or "Fourier domain," allows the
instrument to scan the retina much faster, providing
very high resolution 3-D images of the retina. The
ophthalmologist gets a clearer, more accurate view
of individual tissue layers. This is similar to the
view of other body parts that is obtained with an
MRI. The power of spectral domain OCT also allows
This is an autofluorescence image
repeat examination of the exact same areas of the
of the retina in a normal, healthy
retina at each patient visit, which results in a more
eye. The macula is at the center.
precise measurement of the effects of treatment.
At this time, there is no way to prevent or cure either
the dry (atrophic) or wet (neovascular) form of
macular degeneration. However, significant progress
has been made in treating the condition, and a great
deal of research is currently under way. The most
significant advance has been the development of a
This is an autofluorescence image of the retina in
new class of drugs now being used to treat wet
an eye with dry macular degeneration. The dark
macular degeneration. The drugs are based on the
spots represent areas of lost cells or atrophy. The
brighter spots are sick areas, which may develop
discovery that a group of proteins in the body called
into atrophy in the future.
vascular endothelial growth factor (VEGF) play a
significant role in the formation of the abnormal
blood vessels that damage the retina in wet macular
degeneration. As explained in the Wet Macular
Degeneration section, these abnormal blood vessels
are called choroidal neovascularization (CNV).
The anti-VEGF drugs are injected directly into the
jelly-like substance that fills the back of the eye,
which is called the vitreous. Before the injection,
drops are used to numb the eye and a speculum may
be put in place to hold the eyelids out of the way.
While it may seem scary to receive an injection into
This autofluorescence image shows a more
advanced form of dry macular degeneration
the eye, most patients find that they experience
called geographic atrophy. The dark spot in the
minimal discomfort. Once inside the eye, the
center shows a large area of atrophy in the
medication diffuses throughout the retina and
choroid. It binds strongly to the abnormal VEGF
proteins, preventing the proteins from stimulating
further unwanted blood vessel growth and leakage.
The newest drug for
the treatment of wet
attaches to VEGF
molecules in the
retina and choroid,
preventing them from
abnormal growth of
Before injection of an anti-vascular endothelial
growth factor (VEGF) drug, the eye is numbed
and a speculum may be put in place to keep the
eyelids out of the way.
Two anti-VEGF drugs have been approved by the U.S.
Also, many patients in the study gained a small
Food and Drug Administration (FDA) for the
amount of vision, and some experienced significant
treatment of wet macular degeneration. The one
improvement. It is important to note that the patients
most widely used is Lucentis (ranibizumab). In the
in the study had fairly recently diagnosed macular
studies that evaluated Lucentis, the results were
degeneration that had not yet progressed to scarring.
more favorable than for any other previously FDA-
Each person responds differently to treatment,
approved treatment. Instead of only slowing the rate
depending on his or her individual situation.
of vision loss, the drug appeared to stop disease
progression in most people for as long as two years.
In the studies of Lucentis, patients were given
Your ophthalmologist will explain the advantages
injections every month for up to two years. More
and disadvantages of all available treatments for wet
recent evidence suggests that it may be possible to
macular degeneration and choose your treatment
obtain similar results by giving several injections at
based on your individual case.
monthly intervals and then increasing the time
The FDA-approved anti-VEGF drugs are costly, but
between subsequent injections. Retinal specialists
the pharmaceutical companies that make them offer
are still investigating the optimal timing of injections.
assistance programs for patients who qualify. Ask
Also, research is under way to develop other
your ophthalmologist for information about these
methods of delivering drugs to the eye to reduce the
need for frequent injections.
The first anti-VEGF drug to be approved by the FDA
for the treatment of wet macular degeneration was
Macugen (pegaptanib sodium). It works in a similar
manner to Lucentis, but is not as effective. This is
most likely because it acts against only one form of
the VEGF protein, called VEGF-165, whereas Lucentis
targets all forms of VEGF.
In theory, if Lucentis from the eye were to travel to
other parts of the body and interfere with VEGF, it
could lead to problems, such as an increased risk of
heart attack or stroke. However, the amount of drug
injected is small, and no safety problems have
emerged with the use of Lucentis.
The term "off-label" means using a drug to treat a
been evaluated by a large, formal macular
condition for which the drug was not originally
degeneration study the way Lucentis has. The
intended. For example, aspirin was used to prevent
National Eye Institute is currently conducting a
heart attacks and for blood thinning even though for
study, called the CATT Trial, to directly compare the
a long time the FDA label did not initially list these
safety and effectiveness of Lucentis and Avastin in
wet macular degeneration. The results of the study
should help to provide a final answer to the question
Physicians may use any available drug to treat
of which of these drugs should be routinely used.
macular degeneration, including drugs approved for
other reasons. A drug commonly used off-label for
Another off-label treatment used for wet macular
the treatment of wet macular degeneration is
degeneration is the injection of a steroid, often
Avastin (bevacizumab). Avastin is similar to Lucentis
triamcinolone, into the back of the eye. Steroids fight
because it is an anti-VEGF drug. It is approved by the
inflammation, which recent research has indicated
FDA for the treatment of certain kinds of cancerous
plays a role, along with VEGF, in macular
tumors, which, like CNV, form and grow with the
degeneration. Steroids are typically used in
help of abnormal blood vessels.
combination with other macular degeneration
treatments, such as photodynamic therapy (PDT)
Before the FDA approval of Lucentis, retinal
(see next page) and/or an anti-VEGF drug. If your
specialists had started using Avastin to treat wet
ophthalmologist uses steroids as part of your
macular degeneration. Like Lucentis, Avastin is
macular degeneration treatment, he or she will
injected into the back of the eye. Avastin is being
closely monitor you for potential side-effects, which
used worldwide in the treatment of wet macular
may include the formation of cataracts and elevated
degeneration, and the results appear to be similar to
pressure inside the eye.
the results achieved with Lucentis. However, there
has been a great deal of media attention and some
controversy surrounding these drugs. Although both
may help in wet macular degeneration, Avastin is far
less expensive. On the other hand, Avastin has not
Photodynamic Therapy (PDT)
Photodynamic therapy (PDT) is a treatment for some
forms of wet macular degeneration approved by the
FDA in 2000 and still used in some cases today.
Unlike the anti-VEGF drugs, which affect the
underlying disease process, PDT targets only the
results of the process, the newly formed, abnormal,
leaking blood vessels known as choroidal
neovascularization (CNV). PDT couples a low-
intensity laser with a light-sensitive drug to close the
leaking blood vessels beneath the retina.
To begin the treatment, a special light-sensitive drug
called Visudyne (verteporfin) is infused into a vein in
In PDT, the injected drug accumulates in
the arm and allowed to circulate throughout the
the abnormal blood vessels in the retina.
body. In the bloodstream, the drug attaches itself to
molecules of low-density lipoprotein (LDL) that are
Next, eye drops are used to numb the eye and a
present in the abnormal blood vessels (CNV) in eyes
special contact lens is placed on the eye to focus
with wet macular degeneration.
the laser. At this point, low-intensity laser energy is
directed through the contact lens onto the area of
CNV. The laser energy activates the drug that has
accumulated in the abnormal blood vessels causing
the vessels to close and stop leaking. Using this
low-intensity laser spares the overlying retina
from damage.
Usually, the entire PDT procedure takes less than 30
minutes. For the next several days, as the drug is
clearing from your system, you should not expose
yourself to direct sunlight or other bright lights.
Typically, several sessions of PDT are required to
control CNV. It is common for patients to have as
many as three or four treatments in the first year of
therapy. Your ophthalmologist will use angiograms
and/or optical coherence tomography (OCT) imaging
of your retina to determine if additional treatments
After injection of the drug for PDT, low-intensity
might be beneficial. The goal of treatment is to
laser energy is applied to the area of choroidal
stabilize your vision. Your ophthalmologist will
neovascularization (CNV). The laser helps to
discuss the risks, benefits and limitations of PDT and
close the abnormal vessels where the light-
alternatives for your particular case.
sensitive drug has accumulated.
After successful PDT therapy, the CNV recedes
while leaving the overlying retina intact.
It is increasingly common for wet macular
Another treatment for wet macular degeneration
degeneration to be treated with a combination of
used today in a limited number of cases is thermal
therapies. An anti-VEGF drug may be used in
laser therapy. In this treatment, a thermal (heat-
conjunction with both a steroid and PDT. PDT and
producing) laser is used to coagulate CNV and stop
steroid or PDT and an anti-VEGF drug may also be
the vessels from leaking and spreading. In some
used together. The initial results of using steroids in
cases, the area of involvement may be too extensive
combination with PDT, for example, have shown
or too close to the fovea to treat. Your doctor will
better vision results than would be expected with
discuss with you the risks, benefits and limitations of
PDT alone. Also, adding a steroid to PDT has been
thermal laser treatment and alternatives in your
shown to decrease the number of PDT treatments
required to control CNV. Several large studies are
under way to confirm these findings.
Combination therapy appears to be effective because
the different treatments combat CNV in different
ways. PDT closes already leaking vessels, steroids
act against inflammation and possibly VEGF, and
anti-VEGF drugs address the underlying molecular
events that lead to CNV. The goal of combination
therapy is to control CNV while decreasing the
number of times it must be treated.
When thermal laser is used to treat wet macular
degeneration, a series of precisely controlled
beams of laser energy are directed through the
pupil. Only minimal discomfort is felt as several
pulses of energy are directed at the area of CNV.
Thermal laser treatment for wet macular
The laser light passes through the tissues of the
degeneration is done on an outpatient basis with
retina where the light is absorbed by the CNV and
anesthetic eye drops. To begin the procedure, the
pigmented tissues of the retinal pigment epithelium
patient is seated at a special slit lamp. A lens is
(RPE) and choroid. The absorption of laser energy
placed on the eye to give the ophthalmologist a
produces heat that burns the CNV and some of the
magnified view of the retina through the pupil. Next,
surrounding retinal tissues, causing a small scar to
the laser is aimed directly at the CNV under the
form. After treatment, the scarred area may appear
retina. Only minimal discomfort is felt as several
as a permanent blind spot in your vision.
small pulses of laser light are directed at the CNV.
angiogram shows a
well-defined area of
CNV underneath the
the same eye after
treatment. The
During treatment with thermal laser, the laser light
CNV beneath the
(shown in green) passes through the tissues of the
macula has been
retina. In the area of CNV, the laser energy is
converted into heat (white spot). This heat burns the
CNV and some of the surrounding retinal tissues.
laser scar
Research and Experimental Treatments
It is important to realize that laser treatment
While the efforts of the scientific community have
generally doesn't improve your vision. Laser
already produced new treatments for macular
treatment is a compromise: a small portion of retina
degeneration, the search for even better therapies
is sacrificed in order to prevent more widespread
continues. Many new treatment strategies are being
damage that would occur if the CNV were allowed to
developed and tested. Some of these strategies have
continue growing. When laser treatment is
not yet lived up to expectations, but others continue
successful, the scar produced by the laser is smaller
to show great promise. This chapter provides an
than the scar that would have resulted if the CNV
overview of ongoing research.
had been left untreated.
Even if successful, thermal laser therapy treats the
CNV but not the underlying disease process of
macular degeneration. Therefore, it is common for
Inhibiting the Growth of
CNV to come back in the future. Following laser
Abnormal Blood Vessels
treatment, it is often necessary to use angiography
and OCT to detect any recurrences of CNV. If new CNV
In the wet (neovascular) form of macular degeneration,
is found, your eye doctor may recommend additional
the retina is damaged by the growth of abnormal
treatment to preserve your remaining vision.
blood vessels called choroidal neovascularization
(CNV). It has recently been discovered that a protein
called vascular endothelial growth factor (VEGF) is a
main culprit in this process. Three treatments that
inhibit the activity of VEGF, Lucentis (ranibizumab),
Avastin (bevacizumab) and Macugen (pegaptanib
sodium), are currently available, but other methods of
blocking it are now being studied.
One such method is called RNA interference (RNAi).
While VEGF plays a major role in CNV, other
RNAi, also known as "gene silencing," is being
substances and/or processes in the body may also be
studied for the treatment of a variety of diseases.
involved. Researchers are exploring other targets such
RNA, which is similar to DNA, helps to direct the
as Placental Growth Factor, !5"1 integrin, and the
functions of genes, in particular their production of
nicotinic acetylcholine (nACh) receptor pathway in
proteins in the body. Fragments of RNA, called short
hopes of finding even better treatments.
interfering RNA (siRNA) have been engineered to
An experimental treatment known as AdPEDF
disrupt the production of VEGF once they are
represents a somewhat different approach to
injected into the eye. The potential advantage of
inhibiting the growth of abnormal blood vessels and
siRNA treatment would be its ability to prevent the
causing those that are already present to regress.
production of VEGF. Other anti-VEGF treatments
AdPEDF uses an adenovector, which is a carrier of
work at a later stage in the macular degeneration
DNA, to deliver the Pigment Epithelium-Derived Factor
disease process when excess VEGF has already been
(PEDF) gene to the eye. Once inside, this gene
produced. Some researchers have described this
promotes increased production of PEDF, which serves
difference as "turning off the faucet" instead of
two important functions: regulation of normal blood
"mopping up the floor." SiRNA may also produce
vessel growth and protection of the photoreceptors
fewer unwanted side effects because it works inside
from damage. Protection of the photoreceptors is a
unique aspect of this potential treatment.
Another anti-VEGF treatment which has entered late-
phase clinical trials is called VEGF Trap-Eye. This drug
binds more tightly to VEGF than other anti-VEGF
drugs so, hopefully, its effects will last longer before
repeat treatment is needed.
Targeting the Immune System
and Inflammation
Strong evidence has emerged that a large
Retaane (anecortave acetate) is a medication similar
percentage of macular degeneration cases can be
to but not the same as a steroid. It inhibits the
explained by variations in a gene called Complement
formation of new blood vessels (CNV) that occurs in
Factor H (CFH). This gene is important for helping the
wet macular degeneration.
body's immune system respond to threats. When a
Retaane is very safe, lasts up to six months, and,
variant, or mutated, form of this gene is inherited,
unlike Lucentis, Avastin, and Macugen, it is delivered
the body is less able to control inflammation, which
behind the eye through a curved flexible tube called a
is now believed to be a major contributor to the
cannula. The cannula is slid alongside the eye until the
development of macular degeneration. Multiple
end is resting directly underneath the macula. The
pharmaceutical companies are currently conducting
cannula does not pierce the eye like an injection. Once
research in this area.
the medication is in place, the cannula is removed.
Other genes at work in the immune system have also
Retaane has so far not lived up to expectations.
been linked to the risk of developing macular
degeneration. This body of new knowledge can
potentially lead to earlier detection and treatment of
both the wet and dry forms of the disease.
Anecortave acetate (Retaane) is administered
with a curved cannula. The cannula is slid
alongside the eye until the end is resting
directly under the macula.
Low Dose Radiation Therapy
Radiation therapy for wet macular degeneration is
In many cases of macular degeneration, it appears
under investigation in a number of research centers.
that the retinal pigment epithelium (RPE) is the first
Because growing blood vessels are sensitive to
component of the retina to fail. RPE transplantation is
radiation, it has been suggested that radiation may
an attempt to replace diseased RPE tissue with
stop or slow CNV. The studies completed so far have
healthy RPE cells.
not yielded consistent results. Several small studies
First, a vitrectomy is performed to remove the
have demonstrated some beneficial effects of
vitreous gel from the eye. Then, a small incision is
radiation while other trials have shown no benefit.
made in the retina to gain access to the space beneath
the retina. At this point, RPE cells are injected into
blood vessels are
that space. As time passes and the retina heals, it is
sensitive to radiation,
hoped that these transplanted RPE cells will arrange
it has been suggested
themselves properly to replace lost or diseased RPE.
that radiation may
stop or slow choroidal
For many surgeries
involving the retina,
the vitreous gel must
first be removed from
the eye in a procedure
The type of radiation and the method of delivery are
key factors in how successful such treatments can be.
The ideal radiation therapy would target and affect
only areas of CNV and spare surrounding healthy
tissue and blood vessels. Radiation therapy utilizing
Although RPE cells can be implanted successfully, they
precisely delivered strontium 90 is currently making
may not form the necessary connections with
its way through clinical trials. It is being studied in
neighboring cells and tissues. Additionally, rejection of
conjunction with an anti-VEGF therapy.
these cells by the body is possible.
New RPE cells are
Surgical strategies for treating wet macular
injected under the retina
degeneration have also been explored. For example,
to replace atrophied or
submacular surgery is an attempt to remove CNV, scar
diseased RPE tissue.
tissue and blood from underneath the retina. After a
vitrectomy to remove the vitreous, a small incision is
made in the retina to gain access to the area
underneath. Using fine microsurgical instruments, the
surgeon removes the abnormal vessels from the eye.
In macular degeneration, as in other areas of
In one surgical
medicine, using stem cells to treat or cure disease is
an exciting possibility. Current efforts are aimed at
generating replacement RPE cells from stem cells. The
used to remove
cells could then be inserted into the retina where they
would hopefully develop into functional cells and
photoreceptors, restoring lost vision.
the retina.
Another potential strategy for using human cells to
treat macular degeneration is known as encapsulated
cell technology. This treatment is an implant that is
inserted into the eye. The implant contains human
Early results using this technique have been
cells that have been genetically engineered to
somewhat disappointing. A series of large studies
produce a protein called CNTF. This protein is
known as the Submacular Surgery Trials failed to
believed to protect the retina's specialized nerve
show any significant benefits for these techniques.
cells, the photoreceptors, from damage due to the
Vision is rarely significantly improved, and the blood
dry form of the disease. The implant would regularly
vessels tend to grow back.
release CNTF for an extended period of time,
approximately 18 months.
Implantable Miniature Telescope
Another kind of macular degeneration surgery that
The Implantable Miniature Telescope (IMT) is a tiny
has been performed is called "macular translocation."
optical device that is implanted directly into the eye. It
This technique aims to move the macula when it
magnifies the central visual images onto a larger retinal
overlies diseased subretinal tissues. After a
area than normal to improve vision and the quality of
vitrectomy, a flap of retina is detached from the
life for patients who have lost significant vision to
underlying tissues, cut, and rotated into a new
macular degeneration. After surgical implantation,
position. The rotated retina is reattached to an area
patients undergo a vision rehabilitation program.
of healthier subretinal tissue. In most cases, a second
A second IMT-like device is also currently being tested.
surgery, involving the muscles of the eye, must also
It functions in a similar manner but addresses a
shortcoming of the original design, the loss of
While this experimental technique has helped some
peripheral vision in the IMT eye.
patients, it has been associated with a high percentage
of serious complications. It is only performed at a
handful of medical centers around the country.
With the IMT, central
vision is projected on
the central and
Because macular degeneration results in impaired
Sustained-release drug-delivery devices are also of
functioning of the retina, researchers are attempting
interest. These devices are already in use for other
to bypass the retina using electronics or silicon chips
eye conditions and will likely be applicable to
to send signals to the brain to improve vision.
macular degeneration in the near future. The devices
Typically, surgery is required to implant such devices.
are implanted or inserted into the back of the eye
This type of technology is many years away from
and slowly and continuously release the drugs they
helping people with macular degeneration, but it may
contain. They are capable of doing so for up to
offer hope for improved vision in the future.
several years, reducing or eliminating the need for
other treatments.
Drug Delivery Methods
Most of the available and experimental drug
therapies for macular degeneration currently require
Rheopheresis is a procedure that attempts to remove
injections into the eye. The injections are safe but do
abnormal, harmful circulating proteins from the
carry some risks such as the potential for infection,
bloodstream. Blood is removed from the veins in the
especially when they are given frequently. Therefore,
arm and filtered with a machine to remove heavy
a major goal of ongoing research is the development
proteins. The rest of the blood is returned to the
of less invasive and longer-lasting ways to deliver
bloodstream. This treatment was being evaluated for
drugs to the eye.
dry macular degeneration, but the studies have been
suspended due to financial difficulties within the
Eye drops are one attractive possibility. To be
effective against macular degeneration, an eye drop
formulation must be able to travel from the surface
of the eye into the back of the eye, which has
remained a challenge.
Laser Treatment of Drusen
Health & Nutrition
As explained in previous chapters, most people with
macular degeneration have some drusen or yellow
Risk Factors
deposits underneath the retina. It had been proposed
that applying low intensity laser treatment to the
drusen might cause them to shrink or disappear, thus
A number of factors are known to increase the risk of
eliminating the potential for advancing disease. This
developing age-related macular degeneration. These
theory was evaluated in a large study known as CAPT.
risk factors are: age, family history of the disease,
Unfortunately, in this study, the treatment was neither
smoking, high blood pressure, history of
harmful nor helpful.
cardiovascular disease, elevated serum lipids,
variants of the Complement Factor H gene, and
A different kind of laser treatment may hold more
excessive exposure to bright sunlight. Some of these
promise. In a method called "selective RPE laser
factors are within an individual's control and can be
treatment" (SRT), short laser pulses are applied to
modified through changes in behavior.
damaged areas of the RPE. Researchers believe the
laser will not affect the retina's other layers or cells,
and the treated areas of the RPE will renew
The following factors may increase the risk of
themselves and function normally.
developing age-related macular degeneration:
• age
• family history of the disease
• smoking
• high blood pressure
• history of cardiovascular disease
• elevated serum lipids
• variants of the Complement Factor H gene
• excessive exposure to bright sunlight
The rate of macular degeneration in the population
Elevated serum lipids (cholesterol and triglycerides)
clearly increases with age. By age 75, the odds of
have been associated with an increased risk of
having this condition are greater than 1 in 3.
macular degeneration. If you have either of these
conditions, it is important to follow your doctors'
If your parent or sibling has macular degeneration,
recommendations for diet and medication.
you have an increased risk of developing the disease
yourself.
The Complement Factor H gene is involved in
regulating inflammation in the body. Abnormalities
Smoking has been identified as a strong risk factor for
in this gene have been linked with macular
macular degeneration in many studies. Smoking
degeneration. Ongoing research may lead to new
triples the risk of developing macular degeneration.
insights, diagnostic testing or treatments.
Even secondhand smoking doubles the risk of macular
degeneration compared with the general population.
Excessive exposure of the eyes to sunlight,
It is good to know that stopping smoking will reduce
particularly the blue and ultraviolet wavelengths, is
the risk. And, after 20 years of not smoking, the risks
considered to be a risk factor for both macular
are no different than for non-smokers. It is particularly
degeneration and cataract formation. To protect the
important for people with macular degeneration to try
eyes from excessive exposure to sunlight, sunglasses
to stop smoking in order to protect their vision and to
that block UVB and UVA light should be worn. It is
improve their overall health.
also advisable to wear a hat with a wide brim.
Hypertension (high blood pressure) and cardiovascular
disease may place additional stress on the blood
vessels of the eye, which could accelerate the
development of macular degeneration and vision loss.
The role of nutrition in the development of macular
degeneration is of great interest to patients and
Supplements Used in the AREDS Study:
researchers. Many studies have been conducted over
• Vitamin C 500 mg
the past several years to test whether nutritional
• Vitamin E 400 IU
supplements can prevent or slow the progression of
• Vitamin A as 15 mg beta-carotene 25,000 IU*
macular degeneration.
• Zinc 80 mg as zinc oxide
• Copper 2 mg as cupric oxide
contains a specific list
of ingredients has
*Individuals who smoke should not take supplements
been shown to slow
containing beta-carotene or Vitamin A because they have
the progression of
been associated with an increased risk of developing lung
cancer in smokers. Individuals with other forms of macular
in some people. It is
degeneration such as Stargardt's Disease should consult
important to talk with
their ophthalmologist before taking any supplements.
your doctor before
The supplements used in AREDS appeared to be safe
The largest research study of its kind, the Age-Related
when taken for the duration of the study. Several
Eye Disease Study (AREDS), showed that one group of
brands of supplements containing the AREDS
age-related macular degeneration patients, those who
ingredients are available over-the-counter, but
are at high risk for developing advanced age-related
patients with macular degeneration should consult
macular degeneration, may be helped by taking a
with their eye doctor before taking them. It is
specific combination of antioxidants and zinc. In this
important to note that the supplements only benefit
study, patients in this high-risk group lowered their
people with certain macular degeneration
risk for disease progression by approximately 25
characteristics. Since the supplements contain 5 to
percent when they took the recommended high doses
15 times the recommended daily dietary intake of
of both zinc and antioxidants.
Vitamin E, Vitamin C, copper, zinc and Vitamin
A/beta-carotene, they can be harmful for some people,
Research has shown that people who eat diets high in
such as those with certain health conditions or those
spinach or collard greens are less likely to develop
taking certain medications such as blood thinners.
macular degeneration. These and other green leafy
Additionally, high doses of beta-carotene/Vitamin A
vegetables, such as kale, mustard greens, turnip
have been shown to increase the risk of lung cancer in
greens and romaine lettuce, are good sources of two
individuals who smoke. Also, there are concerns that
important macular pigments: lutein and zeaxanthin.
excessive beta-carotene/Vitamin A could aggravate a
These recommended nutrients are also found in
juvenile form of macular degeneration known as
orange peppers, yellow corn, broccoli, avocados,
oranges and egg yolks.
The National Eye Institute is currently conducting a
second AREDS research project called AREDS2. This
new study is testing the effects of supplements
containing macular xanthophylls (lutein and
zeaxanthin) and/or long-chain Omega-3 fatty acids
(docosahexaenoic acid and eicosapentaenoic acid) on
the progression to advanced age-related macular
degeneration. AREDS2 involves 4,000 people who
have either large drusen in both eyes or large drusen
in one eye and advanced macular degeneration
(neovascular or geographic atrophy) in the other eye.
Based on your particular case and the information
already available about nutrition and age-related
Lutein and zeaxanthin are important
macular degeneration, your eye doctor may
nutrients found in kale, mustard
recommend that you use supplements containing
greens, turnip greens, romaine lettuce,
lutein/zeaxanthin and/or Omega-3 fatty acids.
orange peppers, yellow corn, broccoli,
avocados, oranges and egg yolks.
Lutein and zeaxanthin supplements were not
Good dietary sources
available at the time of the first AREDS study and
of Omega-3 fatty
therefore could not be tested. They are being tested
acids are oily fish
now in AREDS2, and many physicians recommend
tuna), fish oils,
taking supplement formulations containing these
walnuts and some
ingredients or adding these nutrients to your diet.
plant oils (flaxseed,
Some people with macular degeneration have diets
deficient in the mineral zinc. Zinc is found naturally in
shellfish, fish, meat, oats, beans and peas.
Research has shown that patients who eat diets high
acids are fish, fish oils, walnuts and certain plant oils
in Omega-3 fatty acids are less likely to develop
such as flaxseed and canola. Further research is
macular degeneration. These compounds may also
being conducted to obtain a more complete
have a protective role against ongoing retinal
understanding of the impact of these unsaturated
damage. Good dietary sources of Omega-3 fatty
fatty acids on macular degeneration.
For macular health, it is recommended to eat a well-
balanced diet with plenty of fruit, fish and green leafy
vegetables and to avoid excessive saturated fats and
cholesterol. You should talk with your doctor about
also taking a daily multivitamin such as Centrum.
Several substances such as bilberry, ginkgo biloba,
bioflavinoids and shark cartilage have received
attention in the popular media. There is no good
scientific evidence regarding the safety or
effectiveness of these preparations in preventing or
The mineral zinc is found in shellfish, fish, meat,
treating macular degeneration. If you have questions
oats, beans and peas.
about such claims, ask your eye doctor.
Living with Low Vision
The pictures on the following pages illustrate how
the world might look to people with different kinds
of vision impairments that can cause low vision,
including macular degeneration.
Age-related macular degeneration and other types of
macular degeneration can cause central vision to
deteriorate. When central vision deteriorates, it may
be difficult to perform tasks that require detailed
sight, such as recognizing people's faces and seeing
street signs and curbs. Also, it may be difficult or
impossible to read a newspaper or small print on a
pill bottle. Vision impairments such as these cannot
be fixed with regular eyeglasses or contact lenses.
When they interfere with daily activities, they are
referred to as "low vision."
A person with normal vision
A cataract occurs when the
or vision corrected to 20/20
normally transparent lens of
Reading the
with glasses sees this street
the eye starts to become
small print on a
opaque. This street scene
pill bottle may
looks blurred because of
be difficult or
reduced visual acuity, and the
colors do not seem as vivid.
someone with
These effects become more
low vision.
noticeable in glaring light.
With cataracts, print may
appear hazy or lacking in
contrast.
Vision deterioration and low vision can be
frightening. You may fear the loss of your job, a
decrease in your quality of life or the loss of your
independent lifestyle. Thankfully, people rarely lose
all of their vision as a result of macular degeneration
alone. Even if you are "legally blind," which means
your visual acuity on an eye chart is 20/200 or worse
even with glasses, you can continue to lead a
productive and satisfying life. Low vision doesn't
With macular degeneration, With macular degeneration,
signal an end to independent living for most people.
a spot called a scotoma may
print may appear distorted,
appear in central vision. The
and parts of words may be
There are many things you can do to help yourself.
scotoma may look light, dark
For example, you can see a low vision specialist or
or blurred. Sometimes, part of
participate in vision rehabilitation, both of which
an image may look wavy or
help you to learn skills and strategies for making
maximum use of your vision. Also, a wide variety of
low vision optical devices and non-optical devices
are available to help you with everything from
reading, cooking and performing other daily activities
to completing work-related tasks, using a computer
and enjoying leisure activities.
In some individuals with
Central vision often remains
glaucoma, the optic nerve
unchanged by glaucoma.
becomes damaged, causing
some loss of peripheral vision.
A Low Vision Evaluation
If you have experienced some vision loss from
In addition, the low vision specialist will test a very
macular degeneration, your eye doctor may refer you
important aspect of vision called contrast sensitivity.
to a low vision specialist for an evaluation. The
Contrast sensitivity is a measurement of the ability to
specialist will begin your evaluation by asking you
visually separate objects from their backgrounds. For
about your medical, eye and vision history.
example, seeing a large bold black letter on a white
page is easier and requires less contrast sensitivity
To get a better idea of exactly what you can see, the
than seeing a gray car coming over a foggy horizon.
specialist will perform vision tests. Special charts will
The black letter stands out from its background; the
be used to evaluate the acuity, or sharpness, of your
gray car does not. Contrast sensitivity declines as we
near and distance vision. Functional vision tests will
age and as a result of macular degeneration. Poor
also be performed. Functional vision tests evaluate
contrast sensitivity interferes with tasks such as
not only how well you see letters on an eye chart,
reading and seeing a restaurant menu in dim lighting.
but also how well you see faces, clocks, street signs,
It also impedes the ability to move around safely and
newspaper print and many other visual cues that
help guide all of us through the day.
During the evaluation, it is important to tell the
specialist what activities you need or want to do but
During a low vision
are having difficulty with because of your vision
evaluation, special charts
limitations. Also, let the low vision specialist know if
are used to assess your
you have difficulty adapting to changing levels of
ability to detect contrast.
light when you come indoors or go outside. Tell him
or her if glare bothers you or if you can't seem to find
good lighting for a particular task.
Helpful Devices for Work,
Home and Hobbies
After performing the vision tests and talking with
Examples of low vision optical devices appear on the
you about your interests and what you are having
following pages.
trouble doing, the low vision specialist will help you
test some optical devices that can help.
The types of optical devices the specialist can
• strong reading lenses, also known as
• hand-held and stand magnifiers that have
Strong reading glasses are a
If strong reading glasses do
convenient option because
not provide enough
both hands are free to hold
• electronic magnification devices
and move reading material or
magnifiers can also be used.
to work on a project.
Some have a built-in light
• computer software that includes screen
source that provides increased
magnification, voice output or speech
contrast for reading.
• telescopic devices
Stand magnifiers rest
directly on a page of print.
• absorptive lenses
As long as the magnifier sits
on the page, the letters
remain in focus. Stand
magnifiers are more
powerful than hand-held
devices may also be
referred to as reading
machines or video
magnifiers. They provide
the greatest possible
highest contrast for
reading and performing
close-up tasks.
Some kinds of electronic magnification devices are
Some models are
hand-held. Others are worn on the head, similar to a pair
designed to sit on a
of glasses, and can be focused to see objects at a distance,
desktop; others are
up close or any range in between.
advances in flat screen
higher resolution, which
is an important
with older monitors.
Also, with an electronic
magnification device, you
can make black letters
appear on a white
Telescopic devices make an
Telescopes can also be
background or vice versa,
object appear closer than it
mounted on spectacles for one
whichever is more helpful
really is. Hand-held telescopes or both eyes. They allow the
for you. Advanced
are monocular (for use with
hands to remain free, making
models can scroll words
one eye) and are useful for
them useful for activities such
in continuous lines or up
looking at items like a street
as going to the theater or
the screen like a
sign, a building directory or a playing cards. In some states
teleprompter used by
they can be used for driving.
Also known as tints, filters and sunwear,
Large-print books can be
Telephones with large
absorptive lenses block different
purchased or borrowed from
buttons are easier to use.
wavelengths of light, making it easier for
some people to see. Absorptive lenses
are also available.
may be used indoors or outdoors to
reduce glare, to block ultraviolet or
infrared light or to enhance contrast.
If you have low vision, you may also benefit from
non-optical devices. Hundreds of these products,
such as large-print books, cooking aids, talking
clocks, writing guides and special lighting, can make
everyday living easier. Examples of non-optical low
Writing guides can be used for Many talking devices, such as
vision devices appear on the following pages.
tasks such as addressing an
this calculator, can make daily
envelope or writing a check.
tasks easier for the visually
A Team Effort
The low vision specialist or your eye doctor may
If you have low vision due to macular degeneration,
connect you with other professionals who can help
you may find the following types of resources helpful.
you in a variety of ways. Such professionals may
You can also ask your eye doctor for a list of resources.
• certified low vision therapists
• occupational therapists
Making Life More Livable: Simple Adaptations for
Living at Home After Vision Loss
• vision rehabilitation specialists
Edited by Maureen A. Duffy, M.S.
• orientation and mobility instructors
American Foundation for the Blind Press
• social workers and mental health professionals
Macular Degeneration: The Complete Guide to
Saving and Maximizing Your Sight
• technology specialists
Lylas G. Mogk, M.D., Marja Mogk, Ph.D.
• employment specialists
The Random House Publishing Group
Vision rehabilitation specialists, for example, teach a
Mayo Clinic Guide to Better Vision
skill called eccentric viewing, which would allow you
Edited by Sophie J. Bakri, M.D.
to "look around" dark spots in your vision and use a
Mayo Clinic Health Solutions
more healthy area of your retina to see. Orientation
Coping With Vision Loss: Maximizing
and mobility instructors teach strategies and
What You Can See and Do
techniques for important actions, such as finding
your place in a room or moving around indoors or
Hunter House Publishers
outdoors safely. The ultimate goal of the team of
professionals is to enable you to make absolutely the
best use of the vision you have and to make sure you
receive all of the services that meet your needs.
Information and Support
Library of Congress
National Library Service for the Blind and
Physically Handicapped
American Foundation for the Blind
(800) 232-5463
www.afb.org
Association for Macular Diseases, Inc.
(212) 605-3719
www.macula.org
The Macula Foundation, Inc.
(800) 622-8524
www.macula.org
Large Print and Audio Materials
The American Printing House for the Blind, Inc.
(800) 223-1839
www.aph.org
Eyes Only Quarterly Newsletter
Association for Macular Diseases, Inc.
(212) 605-3719
www.macula.org
The Amsler Grid
The Amsler grid is a quick and simple test you can take
at home to monitor changes in your vision. People with
macular degeneration should test their eyes with the
Amsler grid several times a week.
Directions for using the Amsler grid:
1. If you wear reading glasses, put them on for this test.
2. Hold this book at a comfortable reading distance.
3. Cover one of your eyes.
4. Look at the grid. Keep your eye focused on the white
dot at the center of the grid throughout the test.
5. Without moving your eye from the center dot, notice
the lines that make up the grid. All of the lines should
be straight and all of the squares should look the
same. There shouldn't be any blank, dark, or distorted
areas on the grid.
6. Call your eye doctor right away if you notice anything
unusual or abnormal in your vision.
7. Use the same procedure to test your other eye.
This publication was made possible by The Macula Foundation, Inc.
and the staff of the LuEsther T. Mertz Retinal Research Center,particularly Joan R. Daly, R.N. and Vishnu Hoff.
Source: https://www.digisight.us/fe/documents/AMD-booklet-final.pdf
calendar of events: the Children's asthma and allergy Network @ University Children's medical institute March 2010 "I CAN!" Public Symposium Some babies are allergic to cow's milk. June 2010 " I CAN!" Sports Event miCa (P)079/11/2009 dECEmBEr 09 * Details of the events are correct at the time of print.
The diabetic foot infection can lead to tissue necrosis and amputation. Diabetes is the leading non-traumatic cause of major amputation of the lower limbs. Miles J levyJonathan ValabhjiQ2 NeuropathyNerve damage due to disease of the vasa nervorum results in a ‘glove and stocking' sensorimotor peripheral neuropathy that may progress proximally. The motor component results in dener-vation of the small muscles of the foot, leading to: • hyperextension at the metatarsophalangeal joints