Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Aspirin versus anticoagulation for prevention of venous thromboembolism major lower extremity orthopedic surgery: a systematic review and metaanalysis
ORIGINAL RESEARCH
Aspirin Versus Anticoagulation for Prevention of Venous
Thromboembolism Major Lower Extremity Orthopedic Surgery: A
Systematic Review and Meta-analysis
Frank S. Drescher, MD1*, Brenda E. Sirovich, MD, MS2, Alexandra Lee, MS3, Daniel H. Morrison, MD, MS4, Wesley H. Chiang, MS2,
Robin J. Larson, MD, MPH2
1Geisel School of Medicine at Dartmouth, Pulmonary and Critical Care Medicine, Veterans Affairs Medical Center, White River Junction, Vermont;2Geisel School of Medicine at Dartmouth, and the Dartmouth Institute for Health Policy and Clinical Practice, Center for Education, Lebanon, NewHampshire; 3Herbert Wertheim College of Medicine at Florida International University, Miami, Florida; 4Geisel School of Medicine at Dartmouth, Sec-tion of Otolaryngology, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire.
BACKGROUND: Hip fracture surgery and lower extremity
screened participants for deep venous thrombosis (DVT).
arthroplasty are associated with increased risk of both
Overall rates of DVT did not differ statistically between aspi-
venous thromboembolism and bleeding. The best pharma-
rin and anticoagulants (relative risk [RR]: 1.15 [95% confi-
cologic strategy for reducing these opposing risks is
dence interval {CI}: 0.68–1.96]). Subgrouped by type of
surgery, there was a nonsignificant trend favoring anticoa-gulation following hip fracture repair but not knee or hip
PURPOSE: To compare venous thromboembolism (VTE)
arthroplasty (hip fracture RR: 1.60 [95% CI: 0.80–3.20], 2 tri-
and bleeding rates in adult patients receiving aspirin versus
als; arthroplasty RR: 1.00 [95% CI: 0.49–2.05], 5 trials). The
anticoagulants after major lower extremity orthopedic
risk of bleeding was lower with aspirin than anticoagulants
following hip fracture repair (RR: 0.32 [95% CI: 0.13–0.77], 2
DATA SOURCES: Medline, Cumulative Index to Nursing
trials), with a nonsignificant trend favoring aspirin after
and Allied Health Literature, and the Cochrane Library
arthroplasty (RR: 0.63 [95% CI: 0.33–1.21], 5 trials). Rates
through June 2013; reference lists, ClinicalTrials.gov, and
of pulmonary embolism were too low to provide reliable
scientific meeting abstracts.
STUDY SELECTION: Randomized trials comparing aspirin
CONCLUSION: Compared with anticoagulation, aspirin
to anticoagulants for prevention of VTE following major
may be associated with higher risk of DVT following hip
lower extremity orthopedic surgery.
fracture repair, although bleeding rates were substantially
lower. Aspirin was similarly effective after lower extremity
extracted data on rates of VTE, bleeding, and mortality.
arthroplasty and may be associated with lower bleedingrisk. Journal of Hospital Medicine 2014;000:000–000.
DATA SYNTHESIS: Of 298 studies screened, 8 trials includ-
C 2014 Society of Hospital Medicine
ing 1408 participants met inclusion criteria; all trials
Each year in the United States, over 1 million adults
ity and mortality for patients, as well as substantial
undergo hip fracture surgery or elective total knee or
costs to the healthcare system.6 Although VTE is con-
sidered to be a preventable cause of hospital admis-
improving functional status and quality of life,2,3 each
sion and death,7,8 the postoperative setting presents a
of these procedures is associated with a substantial
particular challenge, as efforts to reduce clotting must
risk of developing a deep vein thrombosis (DVT) or
be balanced against the risk of bleeding.
pulmonary embolism (PE).4,5 Collectively referred to
Despite how common this scenario is, there is no
as venous thromboembolism (VTE), these clots in the
consensus regarding the best pharmacologic strategy.
venous system are associated with significant morbid-
thromboprophylaxis," leaving the clinician to selectthe specific agent.4,5 Explicitly endorsed optionsinclude aspirin, vitamin K antagonists (VKA), unfrac-tionated heparin, fondaparinux, low-molecular-weight
*Address for correspondence and reprint requests: Frank Drescher,MD, Assistant Professor of Medicine, Geisel School of Medicine at Dart-
heparin (LMWH) and IIa/Xa factor inhibitors. Among
mouth, Pulmonary and Critical Care Medicine, Veterans Affairs Medical
these, aspirin, the only nonanticoagulant, has been the
Center,(111) 215 North Main Street, White River Junction, VT 05009;Telephone: 802-295-9363; Fax: 802-291-6257; E-mail:
source of greatest controversy.4,9,10
Two previous systematic reviews comparing aspirin
Additional Supporting Information may be found in the online version of
to anticoagulation for VTE prevention found conflict-
this article.
ing results.11,12 In addition, both used indirect com-
Received: February 12, 2014; Revised: May 9, 2014; Accepted: May 20,
parisons, a method in which the intervention and
comparison data come from different studies, and sus-
2014 Society of Hospital Medicine DOI 10.1002/jhm.2224Published online in Wiley Online Library (Wileyonlinelibrary.com).
ceptibility to confounding is high.13,14 We aimed to
An Official Publication of the Society of Hospital Medicine
Journal of Hospital Medicine Vol 00 No 00 Month 2014
VTE Prevention After Orthopedic Surgery
overcome the limitations of prior efforts to address
our inclusion criteria. We used exploded Medical Sub-
this commonly encountered clinical question by con-
ject Headings terms and key words to generate sets
ducting a systematic review and meta-analysis of
for "aspirin" and "major orthopedic surgery" themes,
randomized controlled trials that directly compared
then used the Boolean term, "AND," to find their
the efficacy and safety of aspirin to anticoagulants for
VTE prevention in adults undergoing common high-risk
Additional Search Methods
We manually reviewed references of relevant articlesand
MATERIAL AND METHODS
ongoing studies or unpublished data. We further
searched the following sources: American College of
Prior to conducting the review, we outlined an
Chest Physicians (ACCP) Evidence-Based Clinical
approach to identifying and selecting eligible studies,
Practice Guidelines,4,17 American Academy of Ortho-
prespecified outcomes of interest, and planned sub-
paedic Surgeons guidelines (AAOS),5 and annual
group analyses. The meta-analysis was performed
meeting abstracts of the American Academy of Ortho-
according to the Preferred Reporting Items for System-
paedic Surgery,18 the American Society of Hematol-
ogy,19 and the ACCP.20
Study Eligibility Criteria
Two pairs of 2 reviewers independently scanned the
We prespecified the following inclusion criteria: (1)
titles and abstracts of identified studies, excluding only
the design was a randomized controlled trial; (2) the
those that were clearly not relevant. The same reviewers
population consisted of patients undergoing major
independently reviewed the full text of each remaining
orthopedic surgery including hip fracture surgery or
study to make final decisions about eligibility.
total knee or hip arthroplasty; (3) the study compared
Data Extraction and Quality Assessment
aspirin to 1 or more anticoagulants: VKA, unfractio-
Two reviewers independently extracted data from
nated heparin, LMWH, thrombin inhibitors, pentasac-
each included study and rendered judgments regarding
charides (eg, fondaparinux), factor Xa/IIa inhibitors
the methodological quality using the Cochrane Risk
dosed for VTE prevention; (4) subjects were followed
for at least 7 days; and (5) the study reported at least1 prespecified outcome of interest. We allowed the use
of pneumatic compression devices, as long as devices
We used Review Manager (RevMan 5.1) to calculate
were used in both arms of the study.
pooled risk ratios using the Mantel-Haenszel methodand random-effects models, which take into account
the presence of variability among included stud-
We designated the rate of proximal DVT (occurring
ies.16,22 We also manually pooled absolute event rates
in the popliteal vein and above) as the primary out-
for each study arm using the study weights assigned in
the pooled risk ratio models.
included rates of PE, PE-related mortality, and all-cause mortality. We required that DVT and PE were
Assessment of Heterogeneity and Reporting Biases
diagnosed by venography, computed tomography
We assessed statistical variability among the studies
(CT) angiography of the chest, pulmonary angiogra-
contributing to each summary estimate and considered
phy, ultrasound Doppler of the legs, or ventilation/
studies unacceptably heterogeneous if the test for het-
perfusion scan. We allowed studies that screened par-
erogeneity P value was <0.10 or the I2 exceeded
ticipants for VTE (including the use of fibrinogen leg
50%.14,16 We constructed funnel plots to assess for
publication bias but had too few studies for reliable
A bleeding event was defined as any need for post-
operative blood transfusion or otherwise clinically sig-nificant bleeding (eg, prolonged postoperative wound
Subgroup Analyses
bleeding). We further defined major bleeding as the
We prespecified subgroup analyses based on the indica-
requirement for blood transfusion of more than 2 U,
tion for the surgery: hip fracture surgery versus total
hematoma requiring surgical evacuation, and bleeding
knee or hip arthroplasty, and according to class of anti-
into a critical organ.
coagulation used: VKA versus heparin compounds.
Study Identification
We searched Medline (January 1948 to June 2013),
Results of Search
Cochrane Library (through June 2013), and CINAHL
Figure 1 shows the number of studies that we eval-
(January 1974 to June 2013) to locate studies meeting
uated during each stage of the study selection process.
An Official Publication of the Society of Hospital Medicine
Journal of Hospital Medicine Vol 00 No 00 Month 2014

VTE Prevention After Orthopedic Surgery
FIG. 1. Flow diagram of the search results. ACCP, American College of Chest Physicians; AOOS, American Academy of Orthopedic Surgeons; ASH; AmericanSociety of Hematology; CINAHL, Cumulative Index to Nursing and Allied Health Literature.
After full-text review, 8 randomized trials met all
was 7 to 21 days. Clinical follow-up extended up to 6
months after surgery. Patients in all included studieswere screened for DVT during the trial period by I-
fibrinogen leg scanning,23,25–27 venography,24,28 or
Table 1 presents the characteristics of the 8 included
ultrasound29,30; some trials also screened all partici-
randomized trials. All were published in peer-reviewed
pants for PE with ventilation/perfusion scanning.27,28
journals from 1982 through 2006.23–30 The trialsincluded a combined total of 1408 subjects, and took
Methodological Quality of Included Studies
place in 4 different countries, including the United
Only 3 studies described their method of random
States,24,26,28–30 Spain,23 Sweden,27 and Canada.25
sequence generation,24–26 and 2 studies specified their
Enrolled patients had a mean age of 76 years (range,
method of allocation concealment.25,26 Only 1 study
74–77 years) among hip fracture surgery studies and
used placebo controls to double blind the study arm
66 years (range, 59–69 years) among elective knee/hip
assignments.25 We judged the overall potential risk of
bias among the eligible studies to be moderate.
Pneumatic compression devices were used in addi-
tion to pharmacologic prevention in 2 studies.29,30
Rate of Proximal DVT
The different classes of anticoagulants used included
Pooling findings of all 7 studies that reported proxi-
warfarin,26,28,30 heparin,23,27 LMWH,29 heparin or
mal DVT rates, we observed no statistically significant
warfarin,24 and danaparoid.25 Treatment duration
difference between aspirin and anticoagulants (10.4%
An Official Publication of the Society of Hospital Medicine
Journal of Hospital Medicine Vol 00 No 00 Month 2014

VTE Prevention After Orthopedic Surgery
TABLE 1. Characteristics of Included Studies
Aspirin (Total/Day)
Heparin or warfarin
NOTE: Abbreviations: N/A, not available; THA, total hip arthroplasty; TKA, total knee arthroplasty.
*Gent reported venous thromboembolism events in the subset of screened patients only: aspirin: n 5 84, danaparoid: n 5 88.
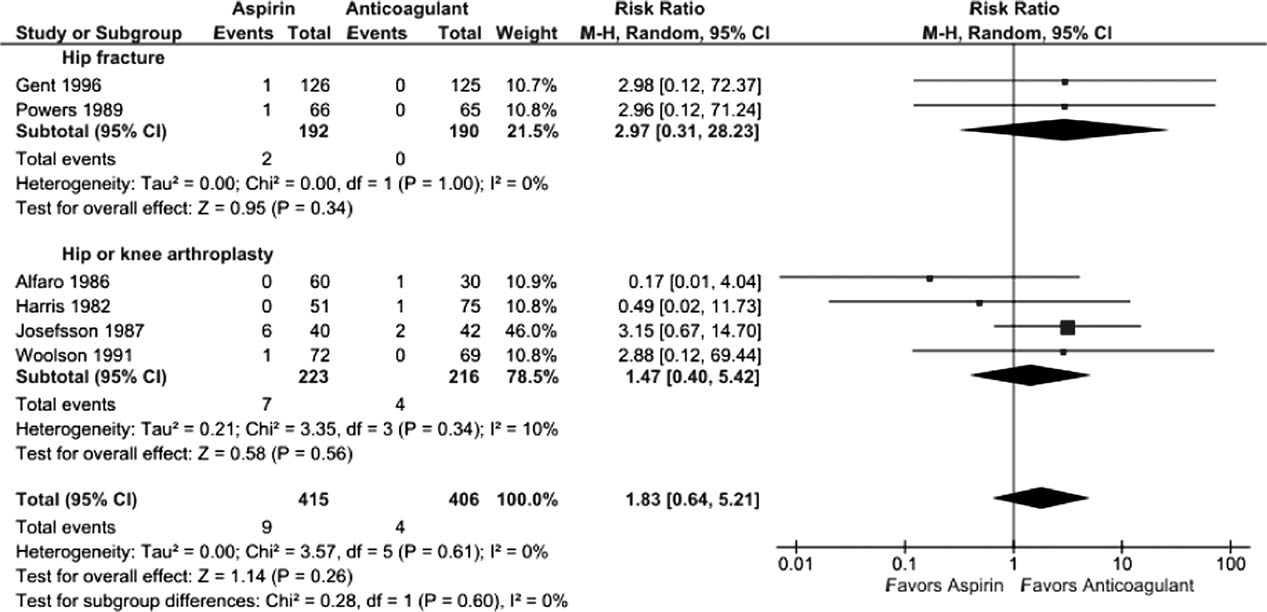
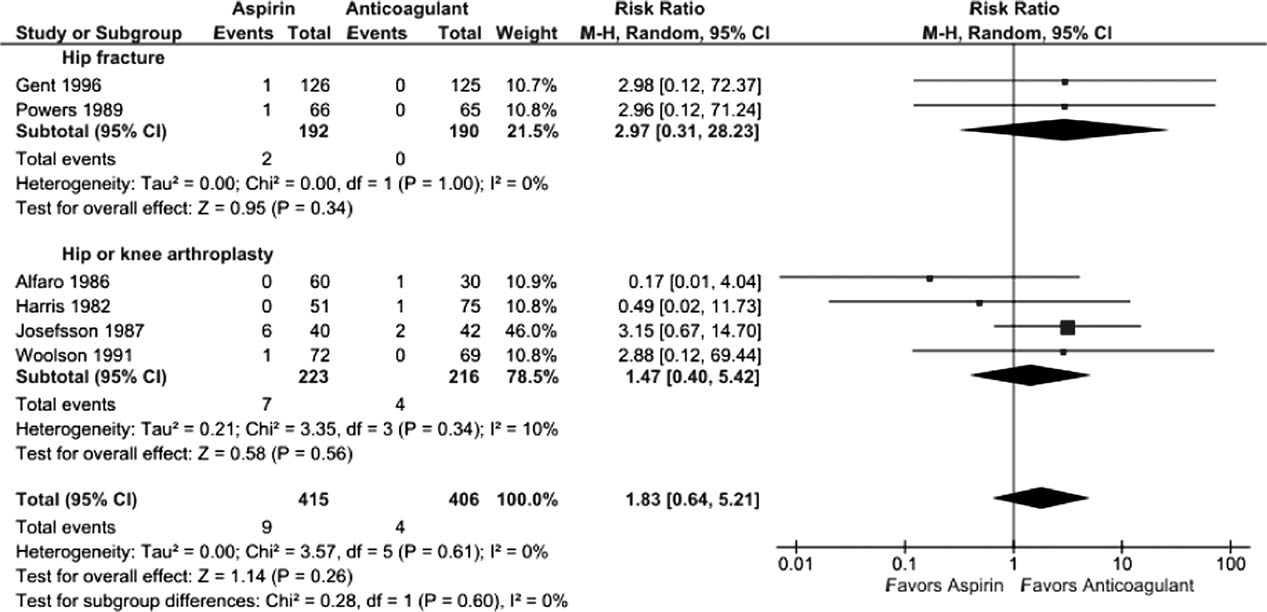
FIG. 2. Effects of aspirin versus anticoagulation on rates of proximal deep venous thrombosis. CI, confidence interval; M-H, Mantel-Haenszel.
vs 9.2%, relative risk [RR]: 1.15 [95% confidence
0.9%, RR: 1.83 [95% CI: 0.64, 5.21], I2 5 0%). The
interval {CI}: 0.68-1.96], I2 5 41%). Although rates
very small number of events rendered extremely wide
did not statistically differ between aspirin and anticoa-
95% CIs in operative subgroup analyses (Figure 3).
gulants in either operative subgroup, there appearedto be a nonsignificant trend favoring anticoagulation
Rates of All-Cause Mortality
after hip fracture repair (12.7% vs 7.8%, RR: 1.60
Only 2 trials, both evaluating aspirin versus anticoa-
[95% CI: 0.80-3.20], I2 5 0%, 2 trials) but not
gulation following hip fracture repair, reported death
following knee or hip arthroplasty (9.3% vs 9.7%,
events, both after 3 months follow-up.25,26 Pooling
RR: 1.00 [95% CI: 0.49-2.05], I2 5 49%, 5 trials)
these results, there was no statistically significant dif-
ference (7.3% vs 6.8%, RR: 1.07 [95% CI: 0.51–2.21], I2 5 0%).
Rate of Pulmonary Embolism
Just 14 participants experienced a PE across all 6 tri-
Pooling all 8 studies, aspirin was associated with a stat-
als reporting this outcome (aspirin n 5 9/405 versus
istically significant 48% decreased risk of bleeding
anticoagulation n 5 5/415). Although PE was numeri-
events compared to anticoagulants (3.8% vs 8.0%, RR:
cally more likely in the aspirin group, this difference
0.52 [95% CI: 0.31–0.86], I2 5 8%). When subgrouped
was not statistically significant (overall: 1.9% vs
An Official Publication of the Society of Hospital Medicine
Journal of Hospital Medicine Vol 00 No 00 Month 2014
VTE Prevention After Orthopedic Surgery
FIG. 3. Effects of aspirin versus anticoagulants on pulmonary embolism rates. CI, confidence interval; M-H, Mantel-Haenszel.
statistically significantly lower in the aspirin group fol-
anticoagulants. This benefit, however, was associated
lowing hip fracture (3.1% vs 10%, RR: 0.32 [95% CI:
with a nonsignificant increase in screen-detected proximal
0.13–0.77], I2 5 0%, 2 trials); however, the observed
DVT. Conversely, among patients undergoing knee or hip
trend favoring aspirin was not statistically significant
arthroplasty, we found no difference in proximal DVT
following arthroplasty (3.9% vs 7.8%, RR: 0.63 [95%
risk between aspirin and anticoagulants and a possible
CI: 0.33–1.21], I2 5 14%, 5 trials) (Figure 4).
trend toward less bleeding risk with aspirin. The rarity of
Five studies reported major bleeding; event rates
pulmonary emboli (and death) made meaningful compari-
were low and no statistically significant differences
sons between aspirin and anticoagulation impossible for
between aspirin and anticoagulants were observed(hip fracture: 3.5% vs 6.3%, RR: 0.46 [95% CI:
either type of surgery.
Our systematic review has several strengths that dif-
5 0%, 2 trials; knee/hip arthroplasty:
2.1% vs 0.6%, RR: 2.86 [95% CI: 0.65–12.60],
ferentiate it from previous analyses. First, we only
included head-to-head randomized trials such that all
5 0%, 3 trials).
included data reflect direct comparisons between aspi-rin and anticoagulation in well-balanced populations.
Subgroup Analysis
Conversely, both recent reviews11,12 were based on
Rates of proximal DVT did not differ between aspirin
indirect comparisons, a type of analysis in which data
and anticoagulants when subgrouped according to
for the intervention and control arms are taken from
anticoagulant class (aspirin vs warfarin: 9.7% vs
different studies and thus different populations. This
10.7%, RR: 0.90 [95% CI: 0.56–1.45], I2 5 0%, 3
methodology is not recommended by the Cochrane
trials; aspirin vs heparin: 10.5% vs 7.9%, RR: 1.37
Collaboration13,14 because of the increased risk of an
[95% CI: 0.47–3.96], I2 5 44%, 4 trials) (data not
unbalanced comparison. For example, Brown and col-
leagues' meta-analysis, which pooled data from
Bleeding rates were lower with aspirin when sub-
selected arms of 14 randomized controlled trials,
grouped according to type of anticoagulant, but the
found the efficacy of aspirin comparable to that of
finding was only statistically significant when com-
anticoagulants, but all aspirin subjects came from a
pared to VKA (aspirin vs VKA: 4.2% vs 11.1%, RR:
single trial of patients at such low risk of VTE that a
0.43 [95% CI: 0.22–0.86] I2 5 0%, 4 trials; aspirin vs
placebo arm was considered justified.31 Similarly, in
heparin: 3.7% vs 7.7%, RR: 0.44 [95% CI: 0.15–
the indirect comparison of Westrich and colleagues,12
1.28], I2 5 44, 4 trials) (data not shown).
which found anticoagulation superior to aspirin, thelikelihood of an unbalanced comparison was further
heightened by their inclusion of observational studies,
We found the balance of risk versus benefit of aspirin
with the attendant risk of confounding by indication.
compared to anticoagulation differed markedly according
Our systematic review further differs from previous
to type of surgery. After hip fracture repair, we found a
analyses by examining both beneficial and harmful
68% reduction in bleeding risk with aspirin compared to
clinical outcomes, and doing so separately for the 2
An Official Publication of the Society of Hospital Medicine
Journal of Hospital Medicine Vol 00 No 00 Month 2014

VTE Prevention After Orthopedic Surgery
FIG. 4. Effects of aspirin versus anticoagulants on bleeding rates (any significant bleed). CI, confidence interval; M-H, Mantel-Haenszel.
most common types of major orthopedic lower
and intermittent pneumatic compression devices are
extremity surgery. This allowed us to discover impor-
standard prophylaxis against postoperative VTE. In
tant differences in the comparative efficacy (benefit vs
fact, only 2 trials used concomitant pneumatic com-
harm) of aspirin versus anticoagulants across different
pression devices, and none treated patients longer
procedure types. Finding that aspirin may have lower
than 21 days, the current standard being up to 35
efficacy for preventing VTE following hip fracture
days.4 Although these limitations may affect overall
repair than arthroplasty may not be surprising in light
event rates, this bias should be balanced between
of the nature of the 2 procedures, the disparate mean
ages typical of patients who undergo each procedure,
randomized controlled trials.
and the underlying trauma in hip fracture patients.
What is a clinician to do? Based on our findings,
The limitations of our review largely reflect the
current guidelines recommending aspirin prophylaxis
quality of the studies we were able to include. First,
against VTE as an alternative following major lower
our pooled sample size remains relatively small, mean-
extremity surgery may not be universally appropriate.
ing that observed nonsignificant differences between
We found that although overall bleeding complica-
aspirin and anticoagulation groups (eg, a nonsignifi-
tions are lower with aspirin, concerns about poor effi-
cant 60% increased risk of DVT for aspirin after hip
cacy remain, specifically for patients undergoing hip
repair, 95% CI: 0.80–3.20) could reasonably reflect
fracture repair. Although some have suggested that
up to 3-fold differences in DVT risk and 5-fold differ-
aspirin use be restricted to low risk patients, this strat-
ences in PE rates. Second, screening for DVT, which
egy has not been experimentally evaluated.33 On the
is neither recommended nor common in clinical prac-
other hand, switching to aspirin after a brief initial
tice, was used in all studies. Reported DVT incidence,
course of LMWH may be an approach warranting
therefore, is undoubtedly higher than what would be
further study, in light of a recent randomized con-
observed in practice; however, the effect on the direc-
trolled trial of 778 patients after elective hip replace-
tion and magnitude of observed relative risks is unpre-
ment, which found equivalent efficacy using 10 days
dictable. Third, included studies used a wide range of
of LMWH followed by aspirin versus additional
aspirin doses, as well as a variety of anticoagulant
LMWH for 28 days.34
types. Although supratherapeutic aspirin doses are
We are able to be more definitive, based on our
unlikely to confer additional benefit for venous throm-
study of best available trial data, in making recom-
boprophylaxis, they may be associated with excess
mendations to investigators embarking on further
bleeding risk.32 Finally, several of the studies were
study of optimal VTE prophylaxis following major
conducted more than10 years ago. Given changes in
orthopedic surgery. First, distinguishing a priori
treatment practices, surgical technique, and prophy-
between the 2 major types of lower extremity major
laxis options, the findings of these studies may not
orthopedic surgery is a high priority. Second, both
reflect current practice, in which early mobilization
bleeding and thromboembolic outcomes must be
An Official Publication of the Society of Hospital Medicine
Journal of Hospital Medicine Vol 00 No 00 Month 2014
VTE Prevention After Orthopedic Surgery
evaluated. Third, only symptomatic events should be
12. Westrich GH, Haas SB, Mosca P, Peterson M. Meta-analysis of
thromboembolic prophylaxis after total knee arthroplasty. J Bone
used to measure VTE outcomes; clinical follow-up
Joint Surg Br. 2000;82(6):795–800.
must continue well beyond discharge, for at least 3
13. Song F, Loke YK, Walsh T, Glenny A-M, Eastwood AJ, Altman DG.
months to ensure ascertainment of clinically relevant
Methodological problems in the use of indirect comparisons for evalu-ating healthcare interventions: survey of published systematic reviews.
should be standardized and represent the standard of
14. Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews
of Interventions Version 5.1.0. Available at:
care, including early immobilization and mechanical
Accessed June 2013.
15. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Pre-
ferred reporting items for systematic reviews and meta-analyses: the
In summary, although definitive recommendations
PRISMA statement. PLoS Med. 2009;6(7):e1000097.
for or against the use of aspirin instead of anticoagu-
16. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for
reporting systematic reviews and meta-analyses of studies that evalu-
lation for VTE prevention following major orthope-
ate health care interventions: explanation and elaboration. PLoS Med.
dic surgery are not possible, our findings suggest
17. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous throm-
that, following hip fracture repair, the lower risk of
boembolism: American College of Chest Physicians evidence-based
bleeding with aspirin is likely outweighed by a prob-
clinical practice guidelines (8th edition). Chest. 2008;133(6 suppl):381S–453S.
able trend toward higher risk of VTE. On the other
18. Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical
hand, the balance of these opposing risks may favor
patients: antithrombotic therapy and prevention of thrombosis, 9thed: American College of Chest Physicians evidence-based clinical prac-
aspirin after elective knee or hip arthroplasty. A
tice guidelines. Chest. 2012;141(2 suppl):e195S–e226S.
comparative study of aspirin, anticoagulation, and a
19. ASH Annual Meeting Abstracts-Blood. Available at:
hybrid strategy (eg, brief anticoagulation followed by
Accessed June 2013.
aspirin) after elective knee or hip arthroplasty should
20. CHEST Publications Meeting Abstracts. Available at:
be a high priority given our aging population and
increasing demand for major orthopedic lower
21. Higgins JPT, Altman DG, Gotzsche PC, et al. The Cochrane Collabo-
extremity surgery.
ration's tool for assessing risk of bias in randomised trials. BMJ.
2011;343:d5928.
22. Review Manager (RevMan) [computer program]. Version 5.1. Copen-
hagen, Denmark: The Nordic Cochrane Centre, The Cochrane Col-
laboration; 2011.
The authors thank Dr. Deborah Ornstein (Associate Professor of Medi-
23. Alfaro MJ, Paramo JA, Rocha E. Prophylaxis of thromboembolic dis-
cine, Geisel School of Medicine at Dartmouth, Section of Hematology
ease and platelet-related changes following total hip replacement: a
Mary Hitchcock Memorial Hospital, Lebanon, New Hampshire) for
sparking the idea for this systematic review.
Thromb Haemost. 1986;56(1):53–56.
Disclosures: Nothing to report.
24. Harris WH, Athanasoulis CA, Waltman AC, Salzman EW. High and
low-dose aspirin prophylaxis against venous thromboembolic diseasein total hip replacement. J Bone Joint Surg Am. 1982;64(1):63–66.
25. Gent M, Hirsh J, Ginsberg JS, et al. Low-molecular-weight heparinoid
1. Healthcare Cost and Utilization Project (HCUP). Available at: http://
orgaran is more effective than aspirin in the prevention of venous
hcupnet.ahrq.gov. Accessed June 2013.
thromboembolism after surgery for hip fracture. Circulation. 1996;
2. March LM, Cross MJ, Lapsley H, et al. Outcomes after hip or knee
replacement surgery for osteoarthritis. A prospective cohort study
26. Powers PJ, Gent M, Jay RM, et al. A randomized trial of less intense
comparing patients' quality of life before and after surgery with age-
postoperative warfarin or aspirin therapy in the prevention of venous
related population norms. Med J Aust. 1999;171(5):235–238.
thromboembolism after surgery for fractured hip. Arch Intern Med.
3. Ng CY, Ballantyne JA, Brenkel IJ. Quality of life and functional out-
come after primary total hip replacement. A five-year follow-up.
27. Josefsson G, Dahlqvist A, Bodfors B. Prevention of thromboembolism
J Bone Joint Surg Br. 2007;89(7):868–873.
in total hip replacement. Aspirin versus dihydroergotamine-heparin.
4. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in
Acta Orthop Scand. 1987;58(6):626–629.
orthopedic surgery patients: antithrombotic therapy and prevention of
28. Lotke PA, Palevsky H, Keenan AM, et al. Aspirin and warfarin for
thrombosis, 9th ed: American College of Chest Physicians evidence-
thromboembolic disease after total joint arthroplasty. Clin Orthop
based clinical practice guidelines. Chest. 2012;141(2 suppl):e278S–
Relat Res. 1996;(324):251–258.
5. American Academy of Orthopaedic Surgeons (AAOS). American
29. Westrich GH, Bottner F, Windsor RE, Laskin RS, Haas SB, Sculco
Academy of Orthopaedic Surgeons clinical practice guideline on pre-
TP. VenaFlow plus Lovenox vs VenaFlow plus aspirin for throm-
venting venous thromboembolic disease in patients undergoing elec-
boembolic disease prophylaxis in total knee arthroplasty. J Arthro-
tive hip and knee arthroplasty. Rosemont, IL: American Academy of
plasty. 2006;21(6 suppl 2):139–143.
Orthopaedic Surgeons; 2011. Available at: http://www.aaos.org/
30. Woolson ST, Watt JM. Intermittent pneumatic compression to pre-
research/guidelines. Accessed June 2013.
vent proximal deep venous thrombosis during and after total hip
6. MacDougall DA, Feliu AL, Boccuzzi SJ, Lin J. Economic burden of
replacement. A prospective, randomized study of compression alone,
deep-vein thrombosis, pulmonary embolism, and post-thrombotic syn-
compression and aspirin, and compression and low-dose warfarin.
drome. Am J Health Syst Pharm. 2006;63(20 suppl 6):S5–S15.
J Bone Joint Surg Am. 1991;73(4):507–512.
7. Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hos-
31. Prevention of pulmonary embolism and deep vein thrombosis with
pital patients: are we detecting enough deep vein thrombosis? J R Soc
low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet.
8. Lindblad B, Eriksson A, Bergqvist D. Autopsy-verified pulmonary
32. Yu J, Mehran R, Dangas GD, et al. Safety and efficacy of high- versus
embolism in a surgical department: analysis of the period from 1951
low-dose aspirin after primary percutaneous coronary intervention in
to 1988. Br J Surg. 1991;78(7):849–852.
ST-segment elevation myocardial infarction: the HORIZONS-AMI
9. Colwell CW Jr. What is the state of the art in orthopaedic thrombo-
(Harmonizing Outcomes With Revascularization and Stents in Acute
prophylaxis in lower extremity reconstruction? Instr Course Lect.
Myocardial Infarction) trial. JACC Cardiovasc Interv. 2012;5(12):
10. Stewart DW, Freshour JE. Aspirin for the prophylaxis of venous
33. Intermountain Joint Replacement Center Writing Committee. A pro-
thromboembolic events in orthopedic surgery patients: a comparison
spective comparison of warfarin to aspirin for thromboprophylaxis in
of the AAOS and ACCP guidelines with review of the evidence. Ann
total hip and total knee arthroplasty. J Arthroplasty. 2011;27:e1–e9.
34. Anderson DR, Dunbar MJ, Bohm ER, et al. Aspirin versus low-
11. Brown GA. Venous thromboembolism prophylaxis after major ortho-
molecular-weight heparin for extended venous thromboembolism pro-
paedic surgery: A pooled analysis of randomized controlled trials.
phylaxis after total hip arthroplasty: a randomized trial. Ann Intern
J Arthroplasty. 2009;24(6 supplement 1):77–83.
An Official Publication of the Society of Hospital Medicine
Journal of Hospital Medicine Vol 00 No 00 Month 2014
Source: https://www.manamed.net/docs/clinicals/DrescherAspirin.pdf
Foreword from Chairperson The summary presentation of SEBAC-Nepal's Social Undertakings pertaining to 2015 AD has come to Publication. It is extremely a jubilant occasion to share & cherish the meaningful outcomes and the degree of social economic transformation implanted in the social milieu entailing excluded, deprived, marginalized, vulnerable, resource poor, exploited
The Top 101 Superfoods That Fight Aging The Best Youth-Enhancing Foods, Spices, Herbs, and Other Tricks to Look and Feel 10 Years Younger, Protect Your Skin, Muscles, Organs and Joints to SLOW Aging By Catherine Ebeling RN BSNand Mike Geary, Certified Nutrition Specialist, DISCLAIMER: The information provided by this book and this company is not a substitute for a face-to-face consultation with your physician, and should not be construed as individual medical advice. If a condition persists, please contact your physician. This book is provided for personal and informational purposes only. This book is not to be construed as any attempt to either prescribe or practice medicine. Neither is the book to be understood as putting forth any cure for any type of acute or chronic health problem. You should always consult with a competent, fully licensed medical professional when making any decisions regarding your health. The authors of this book will use reasonable efforts to include up-to-date and accurate information on this book, but make no representations, warranties, or assurances as to the accuracy, currency, or completeness of the information provided. The authors of this book shall not be liable for any damages or injury resulting from your access to, or inability to access, this book, or from your reliance upon any information provided in this book. All rights reserved. No part of this publication may be reproduced, transmitted, transcribed, stored in a retrieval system, or translated into any language, in any form, by any means, without the written permission of the author.