Cialis ist bekannt für seine lange Wirkdauer von bis zu 36 Stunden. Dadurch unterscheidet es sich deutlich von Viagra. Viele Schweizer vergleichen daher Preise und schauen nach Angeboten unter dem Begriff cialis generika schweiz, da Generika erschwinglicher sind.
Microsoft powerpoint - sept 2011 falls prevention for pt (1)
Prevention of Falls in the Person with PD
Prevention of Falls in
Course Description
70 % of persons with Parkinson's
Disease (PD) fall annually. Postural Instability is one the the 4 primary symptoms of PD. Persons with PD have unique intrinsic risk factors that
by Maria Walde-Douglas, PT
put them at risk for falls. Learn about
evidence-based assessment tools and
Struthers Parkinson's Center,
practical intervention strategies to
an NPF Center of Excellence
reduce fall risk in this patient population.
Course Objectives
1. Identify appropriate assessment tools
to assess balance and fall risk in the Parkinson's population
2. Describe risk factors for falls unique to
the person with Parkinson's Disease (PD)
3. Design intervention and treatment
strategies to reduce falls risk for the person with PD
Parkinson's Review:
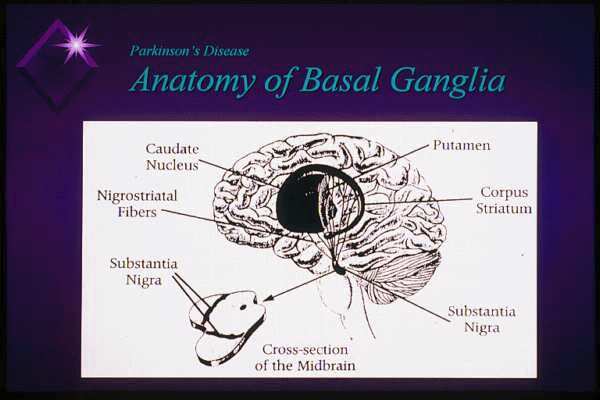
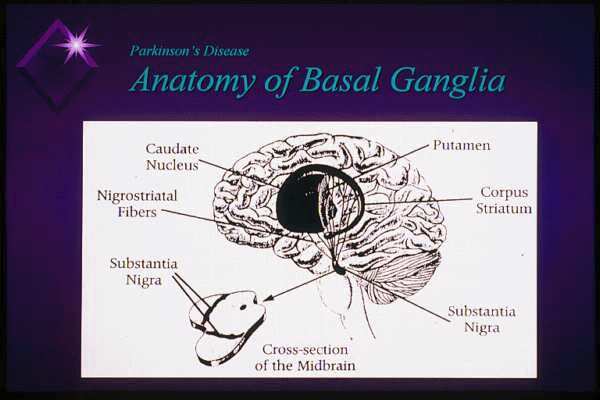
Basic Pathology in Parkinson's
4 Primary Symptoms
• Loss of brain cells in the substantia
• Tremor-resting
nigra that produce the neurotransmitter dopamine
• Rigidity: resistance to passive motion;
can affect trunk/neck (axial) or limbs
• Dopamine is a chemical messenger for
Akinesia or bradykinesia: poverty of
control of movement and coordination
movement or reduced speed
Hypokinesia: reduced amplitude (size) of
• Affects automatic movements so
person experiences loss of "automatic
• Postural Instability-balance
pilot" and is unable to control
impairment; under-scaled balance
movement normally
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Medications in Parkinson's
Common Medication Side Effects
That May Influence PT Plan of Care
• Pharmacologic treatment is aimed at
• Orthostatic hypotension
dopamine replacement :
• Hallucinations
• Most potent, "gold standard"medication is
carbidopa/levadopa (trade name Sinemet)
• Nausea or vomiting
• Dopamine agonists: stimulate parts of the
• Agonists linked with sedation/sleep attacks
brain influenced by dopamine-pramipexole
and compulsive behaviors
(Mirapex) and ropinirole (Requip)
• Dyskinesia: writhing, twisting involuntary
• Many others: anticholinergics, MAO-B
movements caused by PD medication side
Inhibitors, COMT Inhibitors, tremor-control
* only a problem if interferes with function
Modified Hoehn and Yahr Scale
Motor Fluctuations
• Stage 1: Unilateral Symptoms
• The longer the duration on levadopa
• Stage 1.5: Unilateral plus axial involvement
therapy, the greater the change of
• Stage 2: Bilateral symptoms, without balance
variability in motor function:
• Stage 2.5: Mild bilateral symptoms with
– ON: optimal motor function on meds;
recovery on Pull Test
may have dyskinesia
• Stage 3: Mild to mod bilateral symptoms;
some postural instability; physically
– OFF: wearing off of meds or suboptimal
• Stage 4: Severe disability; still able to walk
functioning with increase in PD
or stand unassisted
symptoms such as bradykinesia, rigidity,
• Stage 5: Wheelchair bound or bedridden
Research Synthesis
(Dr. Meg Morris, PT- World Parkinson Congress 2006)
• Fall: unexpected descent into a
• Fall incidence 60% in PD
support surface (floor, chair, steps)
• 20% resulting in a fracture
• Near fall: situation in which a fall
• Near falls 60-75%
almost occurs but a person catches themselves, regains stability with a
• 60% in ON phase
support surface (wall, furniture) or is caught
• Dynamic activities (walking, turning)
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
PD Falls and Injuries
Falls and Parkinson's
Struthers Parkinson's Center
Movement Disorders Journal April 2005
• Age-related changes contribute to
falls but persons with Parkinson's
• 1131 responses (79% response rate)
have twice the fall risk of their peers
• Median disease duration of 7 years• 55.9% had at least one fall in past 2
• Extra intrinsic risk-factors because of
• 65% sustained an injury• 33% sustained a fracture• 75% required health care service
• More risk factors=more falls
Gait and Balance Initiative (GABI)
Struthers Parkinson's Center
supported by a grant from the National Parkinson Foundation
Publication pending
• Cross-sectional study of 453 people with
• Near-falls more frequent than falls
• Direction of falls: 45% forward, 26% backward,
• Applies a multidisciplinary strategy to address
relationship between number of falls and demographic and clinical measures
• Associated symptoms: Wearing off (27%),
• Involved assessments by Neurologists/RNs, PT,
fatigue (24%), freezing (21%), dizziness (15%)
OT, Speech and patient self-assessment tools and falls diary
• Associated activities: Walking (41%), Standing
(27%), Reaching (22%), getting up/down (15%)
Physical Therapy
"Those who fail to study history are
for Balance, Gait and Falls
doomed to repeat it"
Risk in the Person with
Winston Churchhill
Parkinson's Disease
***View every fall as a
learning experience***
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
The WHY of Falling:
Fall/Near Fall Event Log
Keeping a Falls Diary
• Greater clarity about the frequency,
• Record time of day and where you were
cause and circumstances of falls and
in medication cycle (ON, OFF)
• What you doing at the time;
• Useful tool to determine what
changes in activity, behavior, environment need to happen
• Direction of fall
• Useful info for PT to issue on Day
• Witness's perspective or unwitnessed
One of assessment-have
• Symptoms: dizziness, freezing,
patient/carepartner complete for 1-2
dyskinesia, confusion
• Injuries, Medical Attention
Unified Parkinson's Disease
Ask Pertinent Questions
Rating Scale (UPDRS)
• Interview patient /carepartner
Currently the most widely used
carefully including questions listed in
and accepted scale
• "Describe the most recent falls/near
Developed to assess effects of
falls you have had"
medications and/or surgery
• Gives insight into some of the
Can be long and cumbersome
causes/reasons and PD symptoms
for purposes of PT examination
that are leading to falls
*How could it have been prevented?*
Unified Parkinson's Disease
UPDRS Motor Examination
Rating Scale (UPDRS)
Numerical system provides
Components may be useful
common language/rating for
during PT examination to
Parkinson's primary and
quantify Parkinson's symptoms
secondary symptoms
at impairment level:
Not sensitive for assessing progress of PT treatment
Designed for neurologists not
PT; not a functional measure
Postural instability
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
UPDRS Pull Test-for postural
Postural Stability / Pull Test
Scoring from UPDRS
• Patient stands with feet slightly apart
and eyes open and is prepared
0 = Normal1 = Retropulsion but recovers unaided
• Examiner is behind the patient (and is
2 = Absence of postural response, would
also prepared to catch the patient!)
if not caught by examiner.
• A sudden, strong posterior
3 = Very unstable, tends to lose balance
displacement is produced by pull on
patient's shoulders
4 = Unable to stand without assistance
Reactive Postural Response
( Push Release Test )
Postural Response Scoring
Fay Horak-BESTest
Journal of Phys Ther, May 2009
• (3) Recovers stability with ankles, no
One component of BESTest (Balance Evaluation
added arms or hips motion
• (2) Recovers stability with arm or hip
In Place Response forwardIsometric push on anterior shoulders
In Place Response backwardIsometric push on scapulae
• (1) Takes a step to recover stability
Patient stands with feet shoulder width apart, arms
• (0) Would fall if not caught OR
requires assist OR will not attempt
Instructions: Don't let me push you. When I let go,
keep your balance without taking a step
Pushing or Pulling to Detect
Berg Balance Test
Berg, K et al Physiotherapy Canada 1989
Nature Clinical Practice-Neurology
Bloehm, Okun oct 2008
• 2 groups of PD patients: prior fallers and non-
• 14 items, scored 0-4, (56 max score)
• Pull Test and Push Release (PR) Test performed
in dopaminergic On and OFF state
• Self-initiated tasks related to
• Similar diagnostic accuracy but in ON state PR
everyday function (sit to stand,
more accurate in classifying retrospective
forward reach, picking up item on
"Patients with abnormal PR Test should be
floor, 360 degree turn)
candidates for an intensive, multifactorialintervention program, including optimization
• Designed for frail, community
of Parkinson medication, physical therapy and education"
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Percent Probability of Falling
Limitations of Berg
Based on Berg & Fall History
Grid of falls probability
• Documented ceiling effect; fails to
calculated by Diane Wrisley
identify more subtle balance deficits
MS, PT, NCS (from equation in
Shumway-Cook et al, Phys Ther 1997 77:812 -819)
• Less sensitivity to identify
Based on Berg score
abnormalities in postural responses
combined with reports of
seen in persons with PD
number of falls within the
Balance Assessment Tool:
The Mini-BESTest (Dr. Fay Horak)
• Condensed version of Balance
• Identifies more subtle deficits and
Evaluation Systems Test (Phys Ther Vol 89,
changes with therapy; less of a
• 14 item, 32 point test-less cumbersome
ceiling effect than Berg
and time-consuming; more clinically relevant
• Includes Anticipatory, Sensory, Postural
• Found to be as reliable as the BEST
• Contains elements of the Functional
and slightly greater discriminitive
Gait Assessment and includes a Timed
properties for identifying fallers in
Up and Go (TUG) with divided attention
individuals with PD (JNPT, June 2011, Vol 35 )
Research on Best Tool to ID
Balance Resource Website
Fallers in Persons with PD
PT Journal Jan 2011
• Developed by Fay Horak, PhD, PT
• Functional Gait Assessment and
BESTest have reliability and validity
• Contains copies of BESTest MiniBEST
for balance assessment in PD
and various other clinical balance
• BESTest is most sensitive for
identifying fallers
• Cutoff scores for identifying fallers:
– Berg 47/56; 15/30 FGA; 69% BESTest
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Timed Up and Go (TUG)
Posiadlo et al, JAGs
• Subject walks a distance of 3 meters
• Arm chair 18 inches high
(approximately 10 feet).
• Instructions: "When I say go, I
• Performs a practice test first.
want you to stand up and walk to the line, then walk back to this
• Uses customary walking aid.
chair and sit down again. Walk at your normal pace."
• Performance is timed.
TUG Research in PD
PT Journal Jan. 2011
• Older subjects who took 13.5 seconds
or longer were classified as fallers.
• Minimal detectable change (MDC):
• Scores >30 seconds identified patients
smallest amount of difference in
to have significant difficulties with
scores that represent true change
• Normal ranges for young adults were
around 10 seconds.
• Found to sensitive and specific indicator
*MDC in TUG score in persons with PD
of whether falls occur in community
was found to be 3.5 sec
dwelling adults.
• Reliable tool for PD (Meg Morris, et al)
Divided Attention TUG
(Shumway-Cook, et al PT Journal, Sept. 2000)
Can add secondary task to TUG
• Performance in persons with PD
Motor: carrying tray with water
deteriorates with divided attention (dual tasks).
Cognitive: subtract by 3s from 50
or male/female names through
• Cognitive vs. motor tasks proved equally
Combined cognitive and motor task*more relevance to real-life
Need to assess under dual task
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Blood Pressure Screening
Assessing Mental/Emotional
Orthostatic Hypotension
Factors Impacting Fall Risk
Fainting when upright or just upon standing may be cause for falls in PD
Individuals who fall develop a risk
May occur as a result of ANS impairment
for fear of falling, which adds
especially in atypical Parkinsonism or as PD
spiraling risk for additional falling,
greater fear and functional decline
Screen blood pressures in both sitting and standing (wait one minute between position
(Friedman et al, J Am Geri Soc 2002 Aug)
Drop of more than 20 mm Hg systolic or 10
46% fear of falling (self-report
mm Hg diastolic considered orthostatic hypotension
tools) in persons with PD
Patient may be asymptomatic
Fear of Falling and PD
Modified Falls Efficacy Scale
Mov Disorders Journal, May 2003
Arch Phys Med Rehab 1996; 77
14 daily activities self rated on 10 point scale to address confidence with various
• Studied Fear of Falling ( FOF) with
qualitative and quantitative measures of postural control
Updated: Yardley, L et al: Age and Aging 2005)
9 are within home and 5 are in
• FOF an important, independent risk
factor in persons with PD
copies available on www.bestest.us/resources
Activities Specific Balance Confidence Scale
Psychosocial Impact of Falling
Powell et al J Gerentol Med
Sci 50A(1) M28-M34
16 item self rated scale from 0% (no)
• Reduction in community outings social
to 100% (complete) confidence to
isolation decreased activity , decreased
complete each daily task
strength, and endurance
• Issues of pride
Contains more community ambulation
– Reluctance to use assistive device
tasks with 7 activities within the home
– Difficulty accepting assistance
• Embarrassment of PWP or carepartner
Copies available at
• Frequent injury; need to seek medical
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Functional Gait Assessment
Wrisley, DM, Marchetti, GF, Kuharsky, DK and
• Course of known distance.
• 10 items; based on the Dynamic Gait
• Record time (in seconds) to complete
• Developed for use with vestibular disorders
distance ÷ time = feet/second
• Useful for clients with balance dysfunction
that have a ceiling effect score on the Berg
• Gait velocity <2.5 ft/s determined to be
• Head turns, stop and pivot, obstacle,
speed changes, eyes closed, tandem and
higher fall risk (Susan Whitney, PhD, PT,
retro-walking and stairs
University of Pitt.)
• Components of it included in the Mini-BEST• Copies available at
• Useful tool at determining effectiveness of an
• Count the number of steps per
Parkinson's- Related Risk
Factors for Falls
• Useful to quantify a festinating
pattern or document step
Slow, Shuffling Gait
Training BIG for Hypokinesia
Exp Brain Res, 2005, Farley BG, Koshland, GF
• Amplitude problem caused by hypokinesia
• Motor Disorder: Inappropriate scaling
• Reduced foot clearance common cause of
trips particularly on non-level surfaces
• Sensory Disorder: Sensory
• Often worsens with wearing-off of
proprioceptive processing problem
medication or with fatigue
– Mismatch between what person with PD
• Treatment strategies aimed at increasing
perceives their movement to be and
step size to improve foot clearance
how it actually appears
Struthers Parkinson's Center, Golden
Valley, Minnesota
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Large Amplitude Movement
Large Amplitude Gait Training
Dr. Becky Farley, PT
• High effort, intensive training on
• Treadmill and overground walking
increasing SIZE of steps
• Have BIG STEPS be primary focus of
• Can use taped markers on floor (horizontal
lines) agility ladders, footprint cutouts
• Obstacle clearance (foam noodles)
• Intensity is key for best results
(LSVT BIG protocol was 4
• Surface transitions and uneven surface
Turning Instability
Turning Instability
Treatment Strategies
• Multi-step turns common in PD ("wind-
• Focus on wide base of support with rocking
• Often base of support is too narrow
• Train in U Turn method for more open areas
• Rock and Turns with wide base and
• Incomplete weight shift
exaggerated weight shift for confined spaces
• Inappropriate strategies used-crossing
one foot over the other
• Step and turn exercise
Turning Instability
Treatment Strategies
• Incorporate individual turning
• Akinesia: absence of movement; a
strategies into function
temporary motor block
– Build a course that incorporates large and
confined space turns, pivots, 45-90-180-360 turns
• May begin as a start-hesitation or be
• Agility drills that involve quick direction
changes without warning
• Base of support usually too narrow
• Navigation around cones, chairs
• Incomplete weight shift
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Freezing Triggers
• Sudden direction changes, turning, or
• Doorways or thresholds.
• Approaching furniture / obstacles.
STOP (don't force your way through a
• Turning around to sit.
• Change in floor pattern.
STAND TALL (COG over BOS)
• Confined spaces.
SWAY SIDE TO SIDE
STEP LONG ("sticky" foot first)-most
• Stress, anxiety, hurrying.
Struthers Parkinson's Center, Golden
Valley, Minnesota
Rhythmic/Auditory Cues
Tactile/Kinesthetic Cues
• Counting aloud (in synch with weight
• Touch affected foot or knee (with cane or
shift) or chanting
• Clapping or snapping fingers
• Manual weight shift; hands on pelvis
• Metronome (portable-beeps)
• "Dancing" with partner
• Rhythmic Auditory Stimulation (RAS):
specialized technique employed by music therapists
• Complex movement: marching, kick
– Timing music bpm with movement
Struthers Parkinson's Center, Golden
Struthers Parkinson's Center, Golden
Valley, Minnesota
Valley, Minnesota
Carepartner Instruction
• Focus on object BEYOND point of
• Remain calm, avoid hurrying
freeze (i.e. doorway)
• Taped horizontal lines on floor or X
• Avoid pulling on person with PD or their
AD: let them take YOUR arm if necessary
• Laser device on U Step walker or
• Give them space if safety permits; don't
• Foot in front of patient's foot as
obstacle to step over
• Short, simple verbal cues given one at a
• Patterns in tile
Struthers Parkinson's Center, Golden
Struthers Parkinson's Center, Golden
Valley, Minnesota
Valley, Minnesota
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
• Exaggerated weight shifts in wide base of
• Hastening of gait combined with
support in all directions-rocking
reduction in step size; "runaway train"
• Step estimation technique: have patient
estimate how many steps to get from Point
• Often triggered when center of gravity
A to Point B and count them out as they
gets too far ahead of base of support
• Specificity of training in areas that likely to
• Common triggers: reaching into a
trigger freezing; lots of repetition
closet, approach to a chair ("horse sees
• Externally driven locomotion-treadmill,
• Can occur as a result of forcing way
Retropulsion-backward balance
Treatment Strategies
• Focus attention on what leads up to an
episode to trigger it
• Backing up to sit down
• Cues for upright posture and
• Reaching overhead
immediately STOP when shorter, quicker steps occur, widen base of
• Stepping away from sink, counter
support and start again with big step
• Weighted walkers or U Step walker with
• Carrying items close to body in both
resistance control feature may be
• Being approached closely/suddenly
• Rhythmic gait training with metronome
to slow cadence; pacing activities
Compensatory strategies
Treatment Techniques
• Weight shift activities in Power Stance;
add resistance as able (Theraband,
• Power Stance: martial arts split
stance with wide base
• Sidestepping vs. backing away from
• Retro-walking on treadmill (if high
objects like countertops
level) or over-ground with emphasis on
• Heavy duty walker such as U Step
big steps-can add resistance as able
may be necessary to counterbalance
• Backward alternating lunges-
using/near support if needed
Struthers Parkinson's Center, Golden
Valley, Minnesota
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Assistive Devices in PD
• 5 inch swivel casters for front of standard
• Axial (core muscle) rigidity creates
altered trunk mechanics and loss of
• 4 wheeled walker with hand brakes
segmental rotation
• Difficulty moving in multiple planes
• Laser cane-www. U Step.com
• Difficulty initiating and completing
• U Step walker-www. U Step.com
protective responses during activities
• All contribute to increased risk of
• Dashaway Walker-www.dashaway.net
Concepts from Parkinsons Wellness Recovery Training, Dr.
Treatment Strategies
• Multi-plane, reciprocal, rhythmical rotational
Can be major contributor to falls:
movements in varying postures
• Active stretching of flexor musculature
• Exhaustion from sleep disorder or poor
• Yoga Poses: spinal twist, modified revolving
triangle using a chair
• Vicious cycle of feeling tired>becoming
• Transitions from varied positions
more sedentary >muscle atrophy>loss
exaggerating axial rotation and extension
– 4 point to side-sitting to long-sitting with arms
positioned in extension behind trunk
• Imbalance between rest and activity• Fatigue of PD different than ordinary
– Concepts from Parkinsons Wellness Recovery Training, Dr.
Orthostatic Hypotension
Patient Education
Patient Education
• Ankle pumps and leg kicks in seated
• Balance rest and activity: take short rest periods,
position prior to standing to increase
break projects into smaller tasks, one short
daytime nap if needed
• Keep legs moving/weight shifting if
• Healthy sleep habits: avoid excessive daytime
• Encourage regular fluid intake-
sleeping, consistent bedtimes and waking
hydration to increase blood volume
• May need to wear support hose
• Frequent bouts of activity throughout the day:
• Report back to MD for further medical
develop an activity schedule
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Vision and Perceptual Changes:
Vision and Perceptual Changes
Patient Education Strategies
Rick Vandendolder, OT Struthers Parkinsons Center
Rick Vandendolder, OT Struthers Parkinsons Center
• Mark edge of stairs, armrests, walker
handles with brightly colored tape
• Reduced contrast sensitivity
• Bright lighting; especially path to
• Impaired visual spatial perception
bathroom at night or dark stairways
• Slower speed of eye scanning
• Taped markers (X) on floor for
movements in walking path
proper positioning in front of toilet or chair
Impaired Cognitive Function:
Impaired Cognitive Function
Patient Education Strategies
Marjorie Johnson, SLP, CCC Struthers Parkinsons Center
Marjorie Johnson, SLP, CCC Struthers Parkinsons Center
• Lack of attention; selective, dividing, alternating
• Enlist help of carepartner for gentle reminders
and supervision if needed
• Impaired short-term memory
• Post visual cue cards to jog memory
– Remembering to use safety devices and
strategies taught in OT or PT
• Simplify tasks; do one piece at a time
– Do not bombard patient with multiple verbal cues
• Reduced executive function:
Plan>Act>Assess Outcome>Revise Plan
– Problem- solving in novel situations, generalize
**consult Occupational and Speech Therapist for more specific
learning, recognize risky situations, learn from
recommendations and training
past mistakes, "motor recklessness"
Divided Attention
Treatment Strategies
Work on building blocks of floor transfers:
Early Stage PD: Focus on training with motor and cognitive secondary tasks
– Prone to sidelying
Ideas: category naming, backward spelling
– Sidelying to sidesitting
Perform while walking through obstacle
– Sidesitting to 4 point
course, on "stepping stones", or
– 4 point to half kneel with/without support
retrowalking to increase complexity
– Supported ½ stand with wide base
Add to exercise: forward, sideways,
– Pivot to sit in chair safely
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Prevention of Falls in the Person with PD
Interdisciplinary Team
Community Programs
• Comprehensive team approach
• Study of 10 wk comm ex class 2X/wk
works best in area of fall prevention
– Improved grip strength and 6 min walk– Long-term participants (14 mo) showed
similar improvement and NO DECLINE
• Important for compliance and
accountability upon discharge from PT
• PT, OT, SLP, SW, MD, RN collaboration
• Exercise groups: Silver Sneakers,
Modified yoga, Tai Chi, NeuroFit
• Develop an integrated network of
• Each member addresses their scope
providers-education about PD and when
to refer back to PT
"Our greatest glory lies not in
never falling but
in rising every time we fall"
This information is property of Maria Walde-Douglas and should not be copied or otherwise used without express written permission of author
Source: http://www.mnapta.org/associations/11650/files/Parkinsons%20Disease%20and%20Falls%20Prevention.pdf
Kurze Geschichte des Würfels (unknown author) Jede Erfindung hat ein offizielles Geburtsdatum. Das Geburtsdatum des Würfels ist 1974, das Jahr, in dem der erste funktionsfähige Prototyp entstand und die erste Patentanmeldung entworfen wurde. Der Geburtsort war Budapest, die Hauptstadt Ungarns. Der Name des Erfinders ist inzwischen überall bekannt. Damals war Erno Rubik ein Dozent an der Fakultät für Innenarchitektur an der Akademie der angewandten Kunst in Budapest.
The Postural Tachycardia Syndrome A Concise Guide to Diagnosis and Management Blair P. Grubb, M.D., Yousuf Kanjwal, M.D., Daniel J. Kosinski, M.D. J Cardiovasc Electrophysiol. 2006;17(1):108-112. © 2006 Blackwell Publishing During the last 20 years, there has been a tremendous growth in our knowledge of disorders that affect theautonomic nervous system. While at first these investigations centered on neurocardiogenic syncope, a subgroupof patients was identified who suffered from a similar, yet distinct, disorder manifested by postural tachycardia andexercise intolerance. This disorder is now referred to as the postural tachycardia syndrome (POTS) andencompasses a heterogenous group of disorders that share similar clinical characteristics.[1] The aim of this briefreport is to outline the clinical picture, subtypes, diagnosis, and management of POTS.